Overview
This article serves as a comprehensive guide for health tech developers aiming to master ECG analysis. It addresses the challenges faced in ECG interpretation and emphasizes the importance of understanding fundamental concepts, recording techniques, data interpretation, and troubleshooting strategies. By focusing on ECG terminology and proper recording procedures, the article lays a solid foundation for effective analysis.
The guide highlights advanced technologies that can enhance diagnostic accuracy and efficiency. These innovations not only streamline the recording process but also improve the overall quality of ECG data interpretation. By leveraging these technologies, health tech developers can create solutions that significantly benefit healthcare professionals, ultimately leading to better patient outcomes.
In conclusion, understanding ECG analysis is crucial for the development of effective health tech solutions. This article not only provides essential knowledge but also encourages the integration of advanced tools to support accurate diagnostics. By mastering these concepts, developers can contribute to the evolution of health technology in a meaningful way.
Introduction
Mastering the intricacies of electrocardiography (ECG) is increasingly vital as health technology continues to evolve. For health tech developers, a solid understanding of ECG fundamentals, the ability to perform accurate recordings, and effective data interpretation can significantly enhance diagnostic capabilities.
However, the journey toward proficiency is filled with challenges, including the need to master complex terminology and troubleshoot common analysis errors. This raises an important question: how can developers navigate these complexities to ensure accurate and reliable ECG assessments?
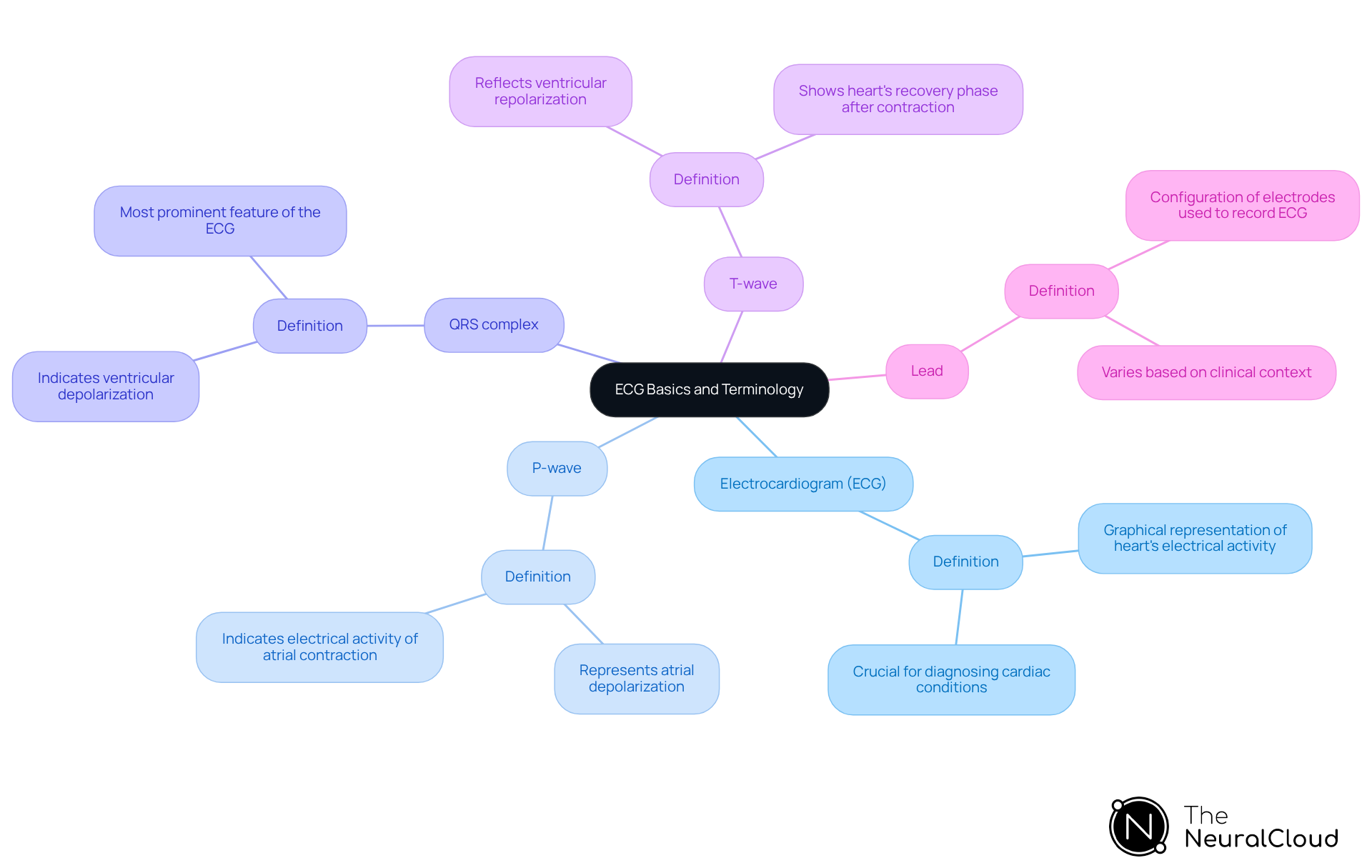
Understand ECG Basics and Terminology
To master how to analyze ECG, it is essential to familiarize yourself with the key terms and concepts that form the foundation of electrocardiography.
- Electrocardiogram (ECG): A graphical representation of the heart's electrical activity over time, crucial for diagnosing various cardiac conditions.
- P-wave: Represents atrial depolarization, indicating the electrical activity associated with the contraction of the atria.
- QRS complex: Indicates ventricular depolarization and is the most prominent feature of the ECG, reflecting the electrical impulses that trigger ventricular contraction.
- T-wave: Reflects ventricular repolarization, showing the heart's recovery phase after contraction.
- Lead: Refers to the configuration of electrodes used to record the ECG, which can vary based on the specific clinical context.
Understanding these terms is vital for navigating the complexities of ECG data and improving your ability to analyze ECG. As the adoption of advanced ECG technologies continues to rise, particularly with the integration of AI-driven solutions, a solid grasp of ECG terminology will empower health tech developers to create more effective diagnostic tools. For further enrichment, consider exploring specialized resources such as cardiology textbooks or online courses that delve deeper into these concepts and their applications in real-world healthcare settings.
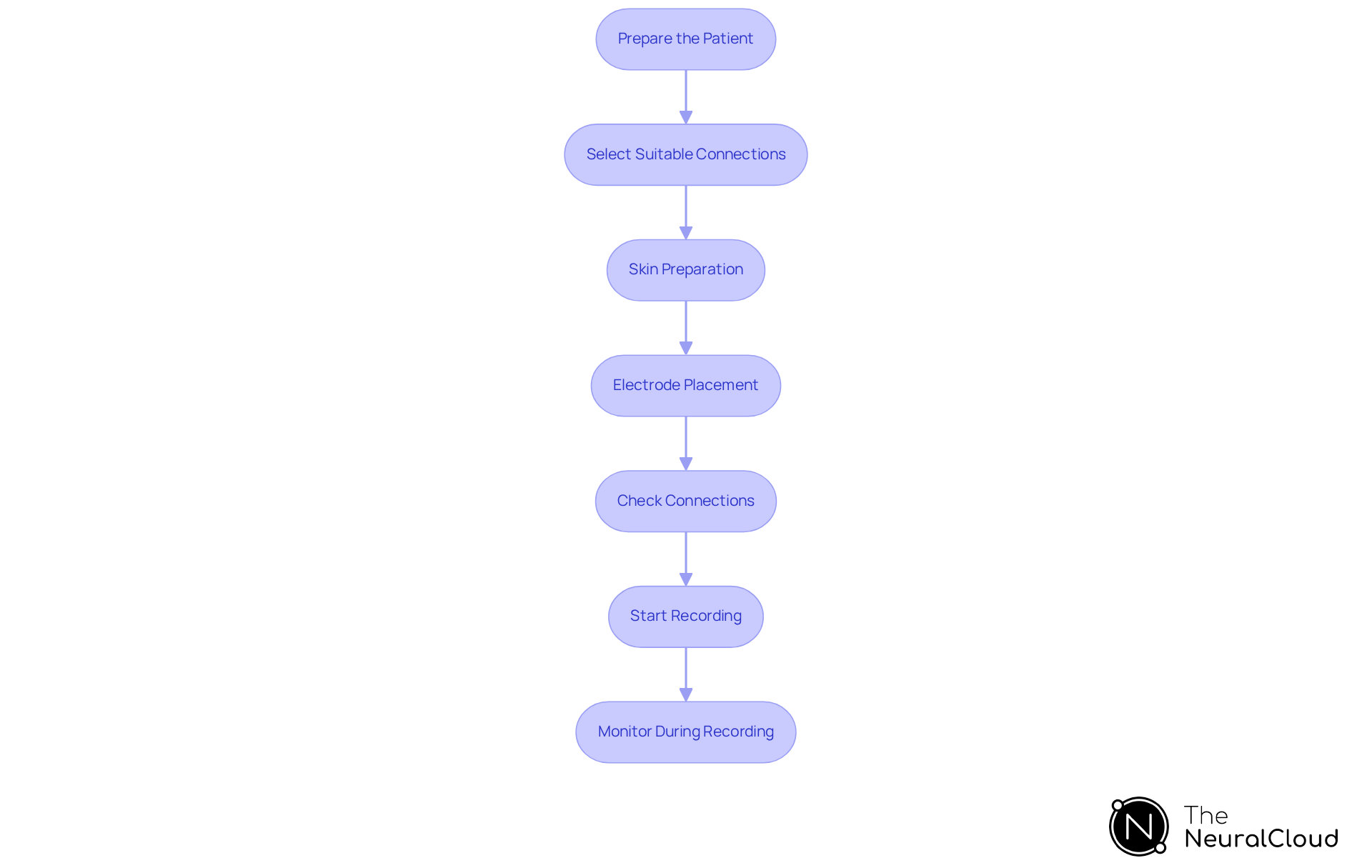
Perform ECG Recording Accurately
To perform accurate ECG recordings, follow these essential steps:
- Prepare the Patient: Ensure the patient is relaxed and in a comfortable position. Clearly explain the procedure to alleviate any anxiety, as patient comfort can significantly impact the quality of the recording.
- Select the Suitable Connections: Choose the correct connection configuration based on the clinical scenario. For comprehensive analysis, a 12-lead ECG is typically recommended, as it provides detailed information about heart activity.
- Skin Preparation: Clean the skin where electrodes will be placed to reduce impedance. Using alcohol wipes to remove oils and dirt is crucial for optimal signal quality.
- Electrode Placement: Follow standard positions for electrode placement, ensuring that limb connections and precordial electrodes are positioned accurately. Precise positioning is essential; research shows that incorrect placement can cause misleading ECG patterns, potentially resulting in misdiagnosis or unnecessary treatments. Notably, only 10% of healthcare workers place all leads correctly, highlighting the critical nature of proper placement. Employing this technology can further enhance the process by providing automated annotations that ensure consistent and precise electrode placement. For optimal use, refer to the user manual for specific guidelines on incorporating the product during the recording process.
- Check Connections: Verify that all electrodes are securely connected to the ECG machine to prevent artifacts. Proper connections are essential for reliable readings.
- Start Recording: Initiate the ECG recording, ensuring that the machine is set to the correct speed (usually 25 mm/s) and gain (typically 10 mm/mV). This configuration is essential for obtaining clear and understandable information. The system supports this process by optimizing information extraction and minimizing the time spent on noise filtering, ultimately aiding in operational cost reduction.
- Monitor During Recording: Continuously observe the ECG trace for any abnormalities or artifacts during the recording process. Immediate identification of issues can help in making necessary adjustments. The AI-powered algorithms of MaxYield™ ensure smooth signals, enhancing the accuracy and reliability of the readings.
By following these steps, healthcare professionals can ensure high-quality ECG information collection, which is foundational for effective analysis ECG and accurate diagnosis. Proper electrode placement, in particular, enhances patient safety and the reliability of ECG results, as evidenced by guidelines from the American Heart Association. As highlighted by cardiologists, "Patient preparation is essential for obtaining precise ECG readings, as it directly affects the quality of the information gathered.
Interpret ECG Data and Identify Key Features
To interpret ECG data effectively, follow these steps:
-
Review the Rhythm: Determine if the rhythm is regular or irregular by measuring the R-R intervals. For irregular rhythms, assess the number of complexes on a 10-second rhythm strip and multiply by 6 to find the heart rate.
-
Measure Heart Rate: Calculate the heart rate by counting the number of R waves in a 6-second strip and multiplying by 10. For a regular rhythm, divide 300 by the number of large squares in one R-R interval to determine the heart rate accurately. A normal heart rate ranges from 60-100 bpm.
-
Identify Key Features: Look for the P-wave, QRS complex, and T-wave:
- P-wave: Should be present before each QRS complex, indicating atrial depolarization.
- QRS Complex: Measure the duration; a normal duration is less than 0.12 seconds. Broad QRS complexes (>0.12 seconds) may suggest abnormal depolarization sequences.
- T-wave: Evaluate the form and orientation; it should be upright in most positions, with small T waves characterized as <5mm in limb positions or <10mm in chest positions.
-
Analyze Intervals: Measure the PR interval (normal range: 0.12-0.20 seconds) and QT interval, correcting for heart rate. A prolonged PR interval (>200 ms) suggests first-degree heart block, which is critical for accurate diagnosis.
-
Look for Abnormalities: Identify any deviations from normal patterns, such as ST-segment elevation or depression, which may indicate ischemia or infarction. For example, ST elevation greater than 1 mm in two or more contiguous limb leads is commonly caused by acute myocardial infarction.
By mastering these interpretation skills, you can enhance your ability to analyze ECG data and provide actionable insights. Utilizing Neural Cloud Solutions' platform can significantly enhance your productivity by automating manual tasks and improving the accuracy of your analysis through advanced noise reduction techniques. The platform's continuous learning model ensures that its diagnostic capabilities evolve with each use, further enhancing your interpretation skills. Cardiologists emphasize the importance of recognizing these key features to analyze ECG, which can improve diagnostic accuracy and patient outcomes. Furthermore, it is crucial to record the interpretation of the ECG in the patient’s notes to guarantee continuity of care, which can be enhanced through the platform's features.

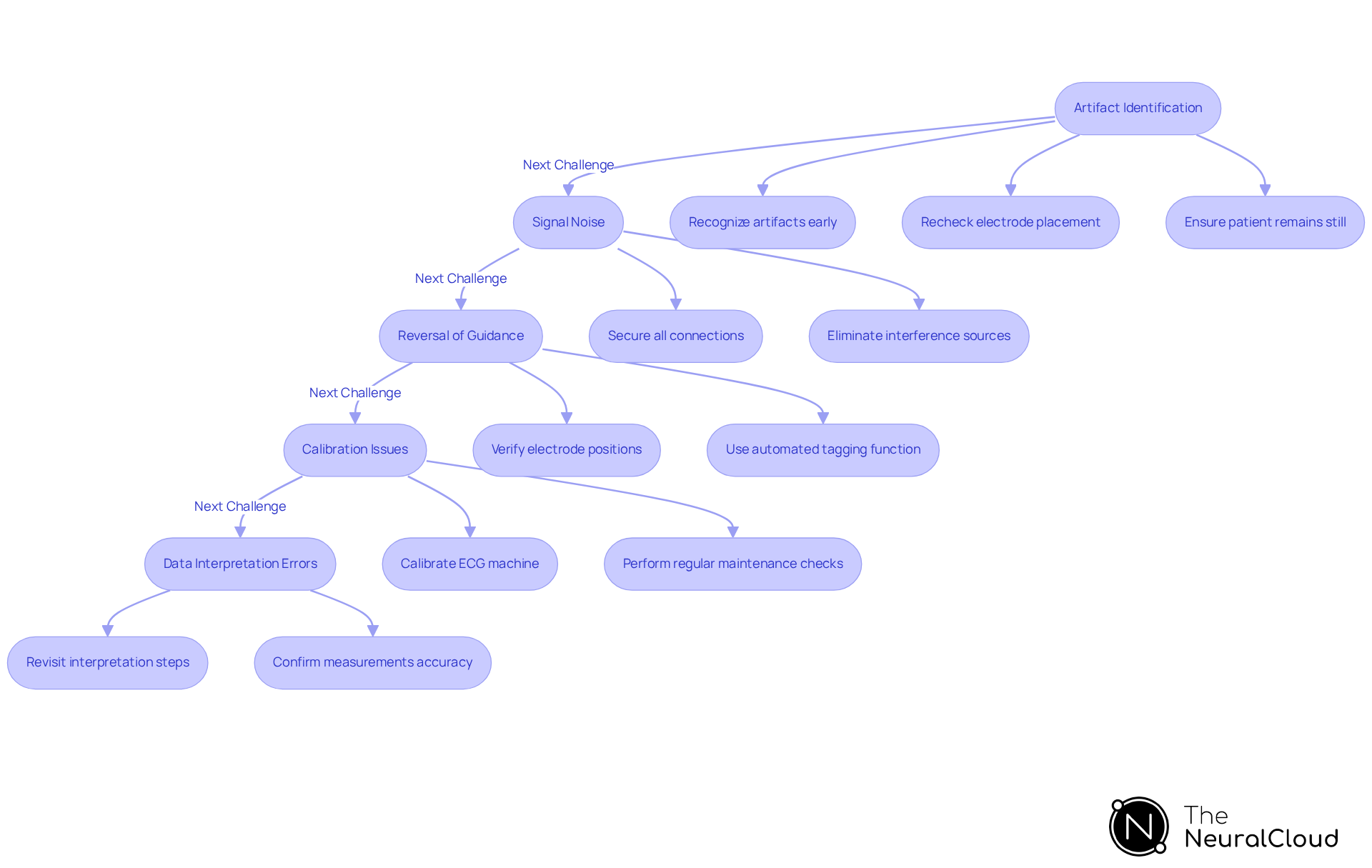
Troubleshoot Common ECG Analysis Challenges
To effectively troubleshoot common ECG analysis challenges, consider the following strategies enhanced by Neural Cloud Solutions' MaxYield™ platform:
-
Artifact Identification: Artifacts may arise from muscle movement, electrical interference, or poor electrode contact. Recognizing these artifacts early is essential. If detected, recheck electrode placement and ensure the patient remains still during recording. Continuous muscle twitching, particularly in patients with Parkinson's disease, can mimic atrial flutter at a rate of 300 bpm, necessitating careful analysis to exclude such artifacts. The Continuous Learning Model within the platform evolves with each use, enhancing its capacity to recognize and eliminate these artifacts over time.
-
Signal Noise: Noisy ECG signals often result from loose connections or external electromagnetic interference. Ensure that all connections are secure and that the recording environment is free from potential interference sources, such as cell phones or fluorescent lights. Studies indicate that errors in electrode placement occur in 0.4% to 4% of ECGs, significantly impacting signal clarity. The MaxYield™ platform automates the filtering process to analyze ECG signals, resulting in crisp and clear outputs that enhance diagnostic yield.
-
Reversal of Guidance: Misplaced indicators can lead to significant misinterpretations of ECG data. For instance, left arm-left leg reversal may produce a pseudo-inferior myocardial infarction pattern. Always verify that electrodes are positioned correctly, as incorrect placements can result in misleading readings, such as inverted P waves in positions I and II. The automated tagging function of the system minimizes the likelihood of such mistakes by offering immediate feedback on placements.
-
Calibration Issues: Proper calibration of the ECG machine is crucial for accurate readings. Ensure that the machine is calibrated to the standard settings of 25 mm/s and 10 mm/mV. Regular maintenance checks can help prevent calibration-related problems that may distort the ECG output. The platform's AI-driven automation assists in maintaining optimal calibration settings, ensuring consistent performance.
-
Data Interpretation Errors: If results appear inconsistent, revisit the interpretation steps. Confirm that all measurements are accurate and correlate with clinical history. Misinterpretation can occur due to artifacts or lead misplacement, emphasizing the need for a systematic approach to ECG analysis. With the sophisticated X-Factor Signal Mapping capability of this system, healthcare professionals can attain improved clarity in information interpretation, minimizing the chances of mistakes.
By proactively addressing these challenges and utilizing the capabilities of Neural Cloud Solutions' MaxYield™ platform, you can significantly enhance the reliability of your ability to analyze ECG, ensuring that the data provided is both actionable and trustworthy.
Conclusion
Mastering ECG analysis is crucial for health tech developers aiming to create effective diagnostic tools. By thoroughly understanding the fundamentals of electrocardiography, including key terminology and ECG components, developers can enhance their analytical skills and contribute significantly to patient care.
The article outlines essential steps for performing accurate ECG recordings, interpreting data, and troubleshooting common challenges. Key points include:
- The importance of patient preparation
- Correct electrode placement
- Systematic analysis of ECG features such as heart rate and rhythm
Emphasizing the role of advanced technologies like AI-driven platforms can streamline these processes, ensuring high-quality data collection and interpretation.
In conclusion, a comprehensive grasp of ECG analysis not only empowers health tech developers but also plays a vital role in improving diagnostic accuracy and patient outcomes. Embracing continual learning and utilizing innovative solutions will be instrumental in overcoming challenges and advancing the field of electrocardiography. As the landscape of healthcare evolves, staying updated with best practices and technological advancements in ECG analysis is essential for driving progress in cardiac care.
Frequently Asked Questions
What is an electrocardiogram (ECG)?
An electrocardiogram (ECG) is a graphical representation of the heart's electrical activity over time, which is crucial for diagnosing various cardiac conditions.
What does the P-wave represent in an ECG?
The P-wave represents atrial depolarization, indicating the electrical activity associated with the contraction of the atria.
What is the significance of the QRS complex in an ECG?
The QRS complex indicates ventricular depolarization and is the most prominent feature of the ECG, reflecting the electrical impulses that trigger ventricular contraction.
What does the T-wave signify in an ECG?
The T-wave reflects ventricular repolarization, showing the heart's recovery phase after contraction.
What is meant by the term 'lead' in the context of ECG?
In the context of ECG, 'lead' refers to the configuration of electrodes used to record the ECG, which can vary based on the specific clinical context.
Why is understanding ECG terminology important?
Understanding ECG terminology is vital for navigating the complexities of ECG data and improving the ability to analyze ECG, especially as advanced ECG technologies and AI-driven solutions are adopted.
How can one further enhance their knowledge of ECG concepts?
One can enhance their knowledge of ECG concepts by exploring specialized resources such as cardiology textbooks or online courses that delve deeper into these concepts and their applications in real-world healthcare settings.






