Introduction
Bifascicular block is a cardiac conduction disorder that impacts the heart's electrical pathways, presenting significant risks to patient health, especially when it remains undiagnosed or untreated. Understanding the nuances of this condition is essential for healthcare professionals, as timely intervention can greatly enhance patient outcomes and reduce the likelihood of progression to more severe cardiac issues.
Clinicians face challenges in diagnosing and treating bifascicular block effectively. This article outlines six essential steps that illuminate the intricacies of this condition while providing actionable strategies for effective management and treatment:
- Assess the patient's history and symptoms.
- Perform a thorough physical examination.
- Utilize appropriate diagnostic tests.
- Interpret the results in the context of the patient's overall health.
- Develop a tailored treatment plan.
- Monitor the patient's progress and adjust the plan as necessary.
By navigating these complexities, healthcare providers can ensure optimal patient care and improve overall health outcomes.
Define Bifascicular Block: Understanding the Condition
Bifascicular obstruction is a cardiac conduction disorder that arises from the impairment of electrical impulses in two of the three primary fascicles within the heart's conduction system. This condition is often recognized as a combination of right bundle branch obstruction (RBBB) and either left anterior fascicular obstruction (LAFB) or left posterior fascicular obstruction (LPFB). The disruption in conduction can lead to delayed or blocked electrical signals, potentially compromising the heart's pumping efficiency.
Recent studies indicate that this specific type of conduction disturbance occurs in 1-2% of the adult population and is frequently associated with structural cardiac disease in 50-80% of cases, as well as ischemic cardiac disease in 40-60% of instances. Notably, in critical situations, a specific conduction issue may manifest without ST elevation in up to 30% of cases, underscoring the importance of thorough ECG analysis.
Complications arising from this conduction disturbance include a significant risk of progression to total cardiac interruption, which ranges from 1% annually in asymptomatic individuals to as high as 17% in those exhibiting symptoms such as syncope. For instance, a study revealed that individuals experiencing syncope had a 17% yearly risk of advancing to complete heart failure, necessitating careful monitoring and potential intervention.
Case studies further illustrate the clinical relevance of this conduction disturbance. One notable case involved a patient with RBBB and LAFB who presented with chest pain and was ultimately diagnosed with a 99% proximal left anterior descending artery occlusion. This highlights the critical importance of recognizing ECG changes associated with a dual bundle branch issue in the context of acute coronary syndrome.
Integrating advanced technologies like Neural Cloud Solutions' MaxYield™ platform can significantly enhance the effectiveness of ECG analysis in patients with a dual fascicle issue. MaxYield™ excels in identifying and labeling critical data amidst high levels of noise and artifact, facilitating the rapid isolation of ECG waves affected by baseline wander and muscle artifact. This capability is essential for salvaging previously obscured segments of lengthy Holter, 1-Lead, and patch monitor recordings, thereby improving diagnostic accuracy.
Understanding bifascicular block treatment is vital for healthcare professionals, as it aids in diagnosis and informs management strategies to mitigate risks associated with fascicular obstruction. By leveraging the advanced capabilities of MaxYield™, clinicians can more effectively address the challenges of diagnosing this specific conduction issue, ultimately leading to better patient outcomes.

Identify Causes of Bifascicular Block: Key Factors and Triggers
Bifascicular block can arise from several key factors:
-
Ischemic Heart Disease: This condition is the leading cause of bifascicular block, accounting for 40-60% of cases. It is frequently associated with coronary artery disease or previous cardiac events, which can harm the organ's electrical conduction pathways. For instance, a recent case highlighted a patient with right bundle branch obstruction (RBBB) and left anterior fascicular obstruction (LAFB) who presented with chest pain, ultimately diagnosed with a 99% proximal left anterior descending artery occlusion.
-
Structural Cardiac Disease: Conditions such as cardiomyopathy and valvular cardiac issues can disrupt normal conduction, leading to a dual bundle interruption. These structural abnormalities significantly impact the heart's electrical system, necessitating careful monitoring and management.
-
Hypertension: Chronic high blood pressure is a significant risk factor for developing conduction abnormalities, including dual fascicle obstruction. Research indicates that individuals with high blood pressure face a higher risk of encountering specific heart conduction issues, underscoring the necessity for proper management of this condition.
-
Age: The risk of bifascicular obstruction increases with age due to degenerative changes in the conduction system. Older adults are more susceptible to the cumulative effects of cardiovascular risk factors, making regular monitoring essential.
-
Congenital Heart Defects: Some individuals may have structural abnormalities from birth that predispose them to conduction issues. These congenital issues can complicate the clinical picture and require specialized care.
Recognizing these causes is vital for implementing appropriate treatment, including bifascicular block treatment and monitoring strategies, particularly in patients with a history of heart disease or those presenting with symptoms such as dizziness, fatigue, or palpitations. Regular monitoring is advised for individuals with mild or asymptomatic conduction issues involving two fascicles, as emphasized by public health initiatives.

Recognize Symptoms of Bifascicular Block: Clinical Indicators
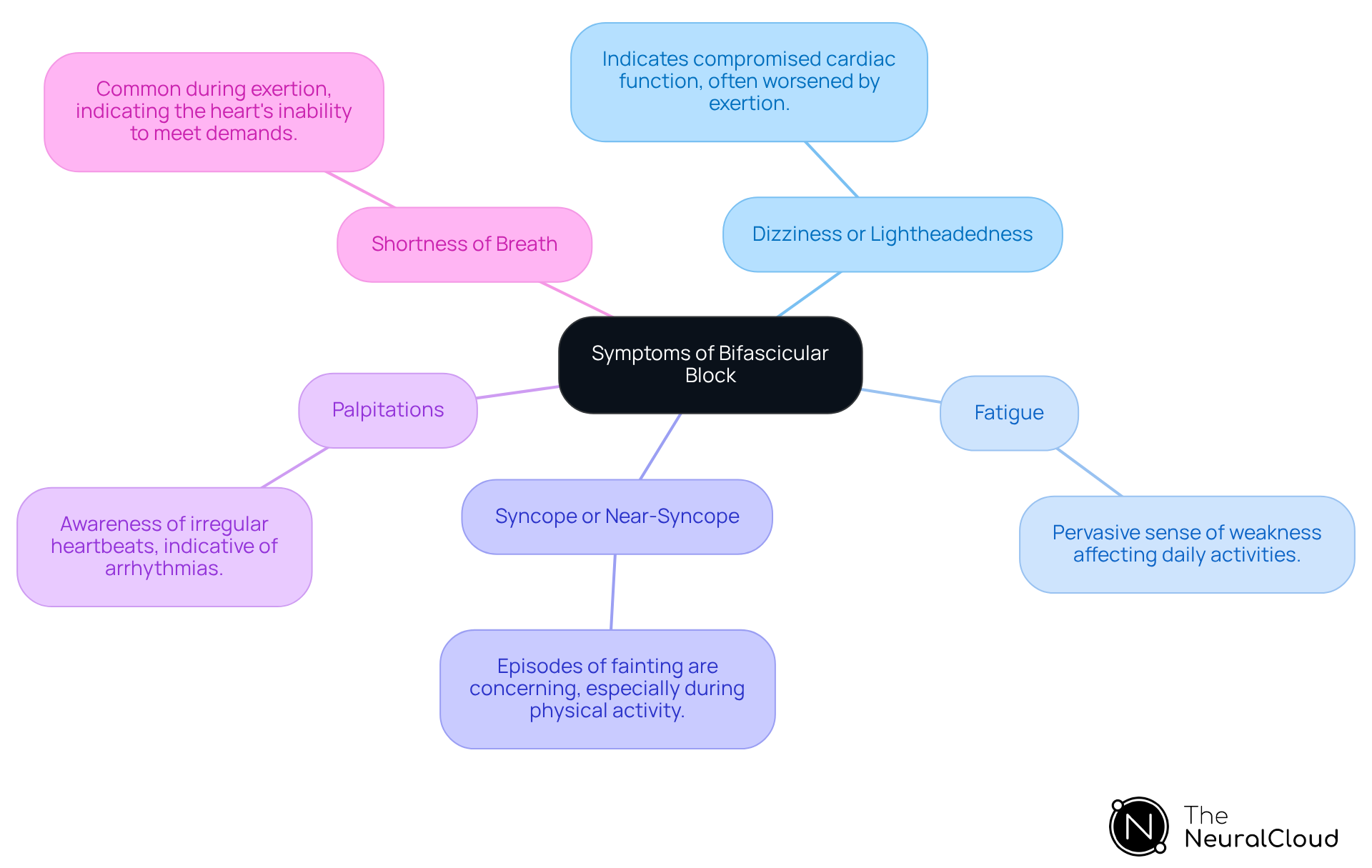
Individuals with a specific type of heart conduction issue may exhibit a range of symptoms that are essential for the diagnosis and bifascicular block treatment. These include:
- Dizziness or Lightheadedness: Often worsened by physical exertion, this symptom can indicate compromised cardiac function.
- Fatigue: Patients frequently report a pervasive sense of weakness or tiredness, which may affect daily activities.
- Syncope or Near-Syncope: Episodes of fainting or near-fainting are particularly concerning, especially during physical activity, and may signal significant conduction issues.
- Palpitations: Patients may experience an awareness of irregular heartbeats, which can be distressing and indicative of underlying arrhythmias.
- Shortness of Breath: This symptom is particularly common during exertion and can indicate the organ's inability to meet increased demands.
Recognizing these clinical indicators is essential for healthcare providers, as they help assess the severity of the condition and determine the necessity for bifascicular block treatment or further diagnostic testing. The main diagnostic instrument for identifying the need for bifascicular block treatment is an electrocardiogram (ECG), which captures the organ's electrical activity and detects irregular conduction patterns.
MaxYield™ Platform Features
With the integration of Neural Cloud Solutions' MaxYield™ platform, healthcare professionals can enhance ECG analysis efficiency through automated labeling and data extraction. This significantly reduces operational costs while improving diagnostic accuracy. The MaxYield™ platform also offers advanced AI-driven solutions and signal mapping, which further streamline the analysis process, allowing for quicker and more accurate assessments.
Advantages for Healthcare Professionals
Certain symptoms warrant immediate medical attention, including severe chest pain, sudden shortness of breath, loss of consciousness, and rapid or irregular heartbeat. Recent research underscores that dizziness and syncope are prevalent in individuals with conduction disorders of the cardiovascular system, stressing the significance of comprehensive assessment in symptomatic persons. For example, the frequency of syncope in individuals with dual fascicle impairment can be as high as 17% annually in symptomatic instances, highlighting the necessity for careful observation and prompt action. Furthermore, the rate of advancement of a specific heart condition to total heart failure can reach 17% annually in symptomatic individuals, emphasizing the importance of identifying these signs.
Diagnose Bifascicular Block: Methods and Techniques
The diagnosis of bifascicular block relies on several key methods:
-
Electrocardiogram (ECG): This remains the cornerstone of diagnosis, where specific patterns such as Right Bundle Branch Block (RBBB) in conjunction with either Left Anterior Fascicular Block (LAFB) or Left Posterior Fascicular Block (LPFB) are identified. For instance, a case study highlighted RBBB with LAFB in an individual presenting with chest pain, revealing a RSR pattern in V1-3 and slurred S waves in lateral leads, which indicated a 99% proximal LAD occlusion. The MaxYield™ platform enhances ECG analysis through advanced noise filtering and distinct wave recognition, allowing for rapid isolation of critical data even in recordings with high levels of noise and artifact. Moreover, the MaxYield™ platform evolves with each use, continuously improving its accuracy and efficiency over time.
-
Clinical Evaluation: A thorough medical history and physical examination are essential for evaluating symptoms and recognizing risk factors linked to dual fascicle disruption. This step ensures that clinicians can tailor their approach based on individual patient profiles. Notably, this type of conduction disturbance is linked with structural cardiovascular disease in 50-80% of instances, highlighting the necessity of comprehensive clinical assessment.
-
Additional Testing: Blood tests are often performed to exclude underlying conditions such as electrolyte imbalances or thyroid dysfunction, which can contribute to conduction abnormalities. This is especially significant since structural cardiac disease is linked to dual fascicular conduction issues in 50-80% of instances.
-
Holter Monitoring: Continuous ECG monitoring is beneficial for detecting intermittent conduction abnormalities that may not be evident during a standard ECG. This method can provide insights into the frequency and nature of arrhythmias, aiding in the overall assessment of cardiac health. The MaxYield™ platform enhances this process by automating the labeling of ECG data, thus improving efficiency and reducing costs associated with manual analysis.
These diagnostic methods are crucial for verifying conduction delay in two fascicles and guiding subsequent treatment plans. As specialists in the field point out, precise diagnosis is essential, particularly considering the possibility of progression to total cardiac failure, which involves a 1-4% yearly risk.

Explore Treatment Options for Bifascicular Block: Strategies and Protocols
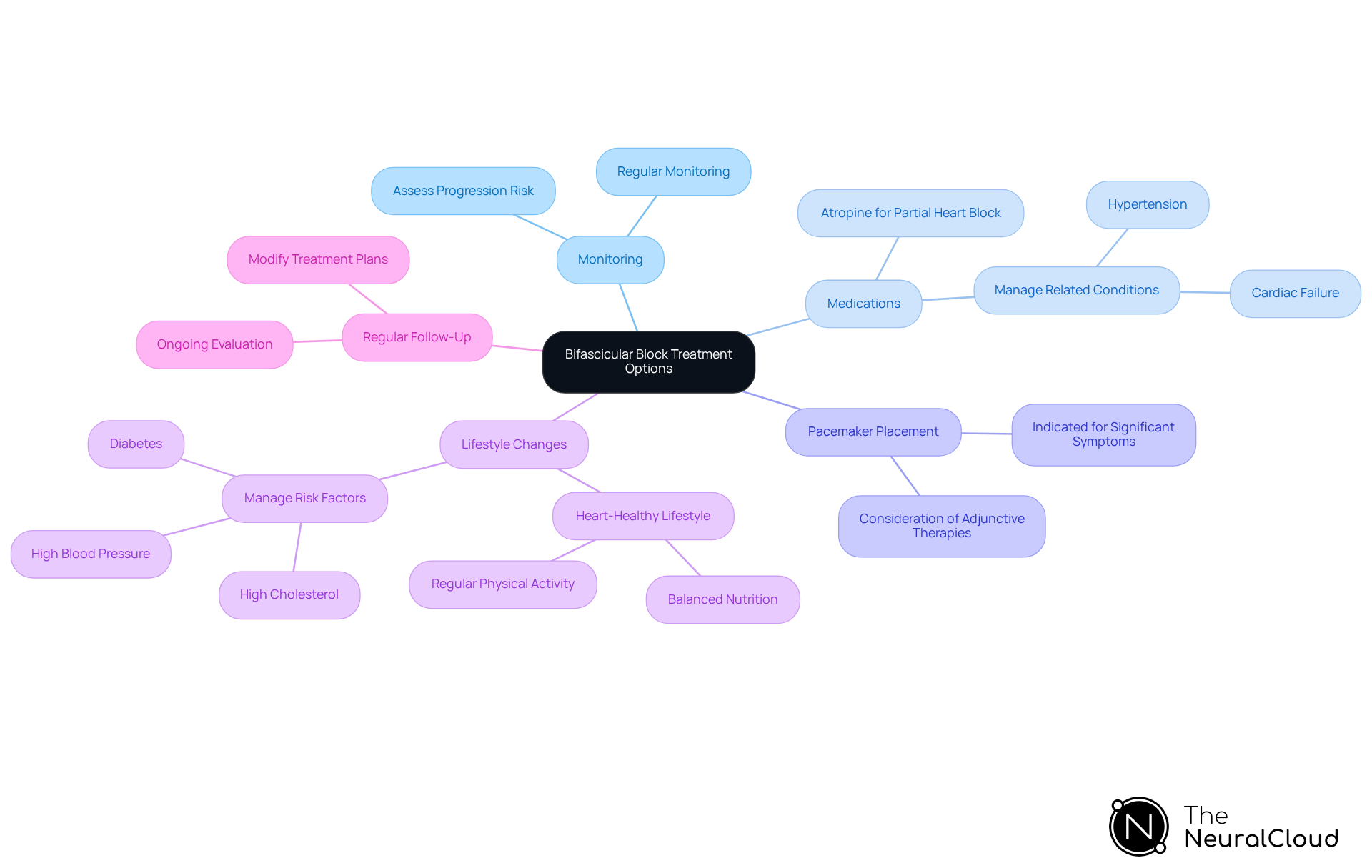
Treatment for bifascicular block varies based on the patient's symptoms and underlying conditions:
-
Monitoring: Asymptomatic patients typically do not require immediate intervention but should undergo regular monitoring to detect any progression of the condition. Research indicates that the likelihood of developing total cardiac obstruction in these patients is low, allowing for a cautious approach.
-
Medications: For symptomatic individuals, bifascicular block treatment may include prescribing medications to manage related conditions such as hypertension or cardiac failure. For example, atropine can effectively alleviate partial heart block when vagal activity is a contributing factor.
-
Bifascicular block treatment: In cases where individuals experience syncope or significant symptoms, the placement of a permanent pacemaker is often indicated as a part of the bifascicular block treatment. Recent findings suggest that while direct pacemaker insertion may be the most efficient strategy, it does not entirely prevent the recurrence of syncope. Therefore, careful selection of individuals and consideration of adjunctive therapies are crucial.
-
Lifestyle Changes: Encouraging a heart-healthy lifestyle, which includes balanced nutrition and regular physical activity, is essential for managing risk factors associated with heart conditions. Effectively managing conditions like high blood pressure, diabetes, and high cholesterol is particularly important.
-
Regular Follow-Up: Ongoing evaluation and follow-up are vital to modify treatment plans as needed, ensuring that any changes in the individual's condition are promptly addressed.
These comprehensive strategies aim to reduce symptoms and lessen complications associated with fascicular impairment, ultimately improving outcomes for individuals with bifascicular block treatment.
Implement Follow-Up Care: Monitoring and Long-Term Management
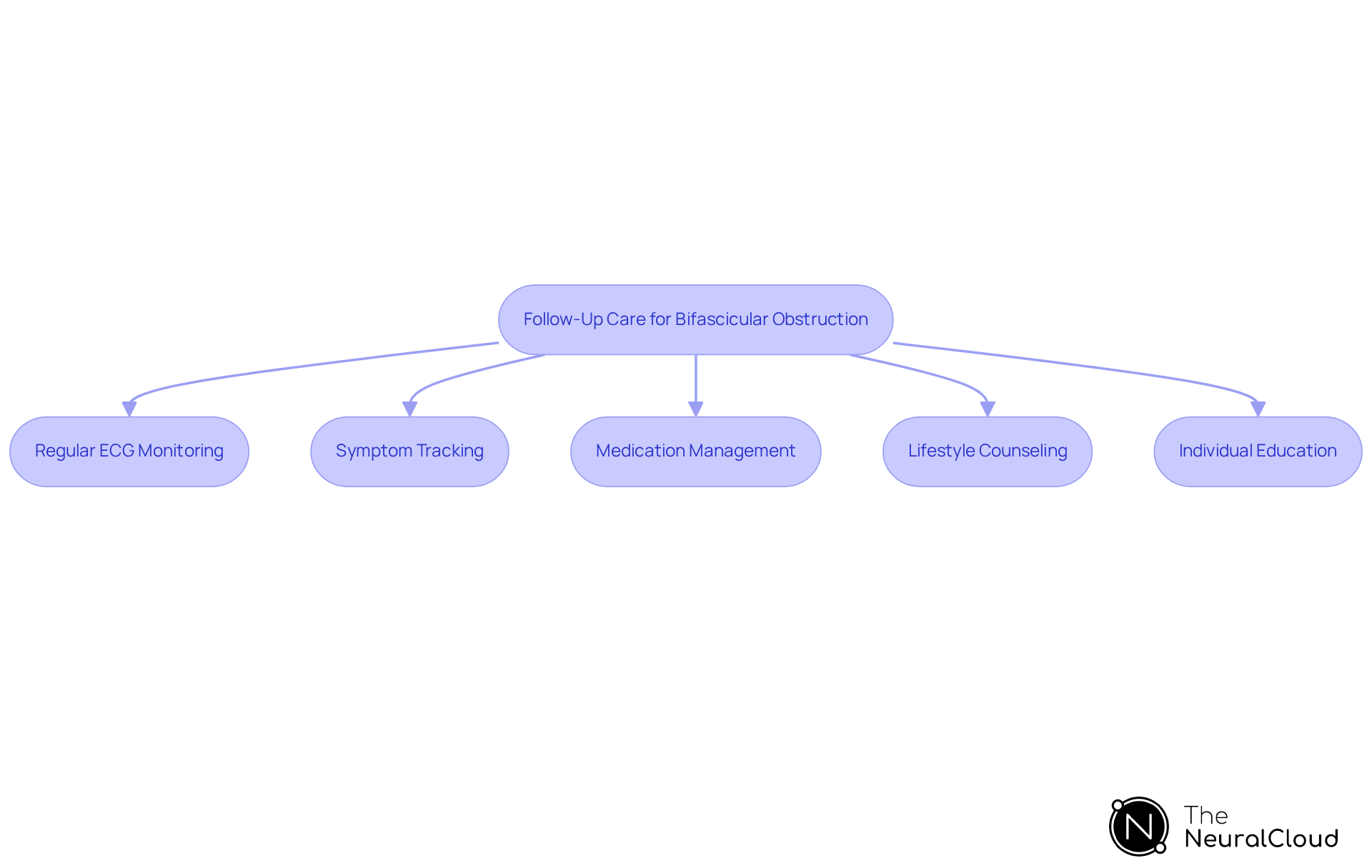
Introducing follow-up care for individuals with bifascicular obstruction is crucial for the bifascicular block treatment to avert complications like complete cardiac failure and to guarantee optimal management. Key strategies include:
- Regular ECG Monitoring: Continuous assessment of conduction patterns is vital. Regular ECGs assist in identifying any changes that may suggest advancement to a more serious heart condition, enabling prompt intervention.
- Symptom Tracking: Patients should be encouraged to actively monitor and report any new or worsening symptoms, such as syncope or palpitations, which can signal deteriorating cardiac function.
- Medication Management: A thorough review of medications is necessary to optimize the treatment of underlying conditions and to adjust therapies as needed, particularly in light of emerging evidence regarding pacing strategies.
- Lifestyle Counseling: Providing ongoing support for lifestyle modifications such as diet, exercise, and smoking cessation can significantly enhance cardiovascular health and overall well-being.
- Individual Education: Instructing individuals about their condition, possible symptoms, and the significance of seeking medical attention swiftly is essential for proactive management.
These follow-up strategies are not only vital for maintaining patient health but also play a significant role in the bifascicular block treatment by mitigating the associated risks. Recent studies show improved outcomes with regular monitoring and timely interventions, underscoring the importance of these practices.
Conclusion
Bifascicular block is a significant cardiac conduction disorder that can lead to serious complications if not properly managed. Understanding this condition - from its definition and causes to its symptoms and treatment options - is crucial for healthcare professionals aiming to improve patient outcomes. Accurate diagnosis and timely intervention are vital in preventing progression to more severe cardiac issues.
Key insights regarding the multifaceted nature of bifascicular block have emerged. The leading causes include ischemic heart disease and structural cardiac abnormalities, with critical symptoms that warrant immediate medical attention. Diagnostic methods such as ECG and continuous monitoring are essential tools for recognizing and managing this condition effectively. Treatment strategies range from lifestyle modifications to the implementation of pacemakers, underscoring the need for personalized care based on individual patient profiles.
Proactive management of bifascicular block is imperative for reducing associated risks. By adopting comprehensive treatment protocols and ensuring regular follow-up care, healthcare providers can significantly enhance the quality of life for patients. The integration of advanced technologies, such as the MaxYield™ platform, supports clinical efforts by improving diagnostic accuracy and patient outcomes.
Features of the MaxYield™ Platform:
- Enhanced ECG Analysis: Provides clearer insights into cardiac conduction disorders.
- Real-Time Monitoring: Allows for immediate detection of changes in patient status.
- User-Friendly Interface: Simplifies the process for healthcare professionals.
Advantages for Healthcare Professionals:
- Improved Diagnostic Accuracy: Reduces the likelihood of misdiagnosis.
- Increased Efficiency: Saves time in patient assessment and management.
- Better Patient Outcomes: Leads to more effective treatment strategies.
Ultimately, a commitment to understanding and addressing bifascicular block will lead to better management strategies and a healthier future for those affected by this cardiac conduction disorder.
Frequently Asked Questions
What is bifascicular block?
Bifascicular block is a cardiac conduction disorder characterized by the impairment of electrical impulses in two of the three primary fascicles in the heart's conduction system. It typically involves a combination of right bundle branch obstruction (RBBB) and either left anterior fascicular obstruction (LAFB) or left posterior fascicular obstruction (LPFB).
How common is bifascicular block in the adult population?
Bifascicular block occurs in 1-2% of the adult population and is often associated with structural cardiac disease in 50-80% of cases, as well as ischemic cardiac disease in 40-60% of instances.
What are the potential complications of bifascicular block?
Complications include a significant risk of progression to total cardiac interruption, which ranges from 1% annually in asymptomatic individuals to as high as 17% in symptomatic individuals, such as those experiencing syncope.
What factors can lead to bifascicular block?
Key factors include ischemic heart disease, structural cardiac disease, hypertension, age, and congenital heart defects. Ischemic heart disease is the leading cause, accounting for 40-60% of cases.
How does ischemic heart disease contribute to bifascicular block?
Ischemic heart disease can damage the heart's electrical conduction pathways, often associated with coronary artery disease or previous cardiac events, leading to bifascicular block.
What role does hypertension play in bifascicular block?
Chronic high blood pressure is a significant risk factor for developing conduction abnormalities, including bifascicular block, as it increases the likelihood of encountering specific heart conduction issues.
Why is age a risk factor for bifascicular block?
The risk of bifascicular block increases with age due to degenerative changes in the heart's conduction system, making older adults more susceptible to cardiovascular risk factors.
How can advanced technologies assist in diagnosing bifascicular block?
Technologies like Neural Cloud Solutions' MaxYield™ platform enhance ECG analysis by identifying and labeling critical data amidst noise and artifacts, improving diagnostic accuracy for patients with bifascicular block.
What is the importance of monitoring patients with bifascicular block?
Regular monitoring is essential, especially for individuals with a history of heart disease or symptoms such as dizziness, fatigue, or palpitations, to implement appropriate treatment and management strategies.






