Introduction
Understanding supraventricular tachycardia (SVT) is essential for healthcare professionals working with cardiac arrhythmias. This tutorial provides a clear overview of the mechanisms, classifications, and diagnostic approaches necessary for mastering SVT strips. By breaking down these complexities, we aim to equip clinicians with the insights needed for effective management strategies.
However, various types of SVT present unique challenges. Clinicians must navigate these complexities to ensure accurate diagnosis and optimal treatment while minimizing risks to their patients. This article will explore how the MaxYield™ platform enhances ECG analysis, providing healthcare professionals with the tools they need to improve patient outcomes.
Define Supraventricular Tachycardia: Key Concepts and Mechanisms
Supraventricular tachycardia (SVT) includes various rapid heart rhythms that originate from above the ventricles, specifically within the atria or the atrioventricular (AV) node. The term 'supraventricular' indicates that the abnormal electrical impulses come from areas above the ventricles, leading to heart rates exceeding 100 beats per minute in adults, and ranging from 180 to 220 bpm in children. SVT can result from several factors, including reentrant circuits, ectopic foci, or enhanced automaticity. Understanding these mechanisms is essential for recognizing the clinical implications of the supraventricular tachycardia strip, which may present as symptoms like palpitations, dizziness, and potential hemodynamic instability.
Approximately 35 individuals per 100,000 experience SVT, with a notable prevalence among those aged 45 to 64 years. The clinical presentation can vary significantly; while many individuals remain asymptomatic, others may experience severe symptoms that necessitate urgent medical attention. For example, in cases of atrioventricular nodal reentrant tachycardia (AVNRT), the heart rate typically reaches around 180 to 220 bpm, which can be seen on a supraventricular tachycardia strip characterized by a narrow QRS complex on the ECG. This highlights the importance of accurate diagnosis and timely management, as untreated SVT can lead to complications such as syncope or even sudden cardiac death in rare instances.
Synchronized cardioversion is recommended for individuals with hemodynamic instability, emphasizing the need for prompt treatment. Real-world diagnostic approaches often involve Holter monitors or event recorders to capture infrequent episodes that may not be evident on a standard 12-lead ECG. By integrating advanced solutions like Neural Cloud Solutions' MaxYield™, healthcare professionals can significantly enhance their diagnostic capabilities.
MaxYield™ Features:
- Automates ECG analysis
- Maps signals through noise to isolate and label key features in every heartbeat
- Rapidly analyzes 200,000 heartbeats in less than 5 minutes
These features allow clinicians to transform noisy recordings into detailed insights. Utilizing MaxYield™ enables healthcare professionals to identify cardiac events more effectively, directly addressing the clinical needs associated with SVT and supporting confident clinical decisions. As noted by the Arrhythmia Alliance, 'A supraventricular tachycardia strip is characterized by a narrow QRS complex of less than 120 ms and an elevated heart rate.' This underscores the critical nature of recognizing and managing SVT effectively.

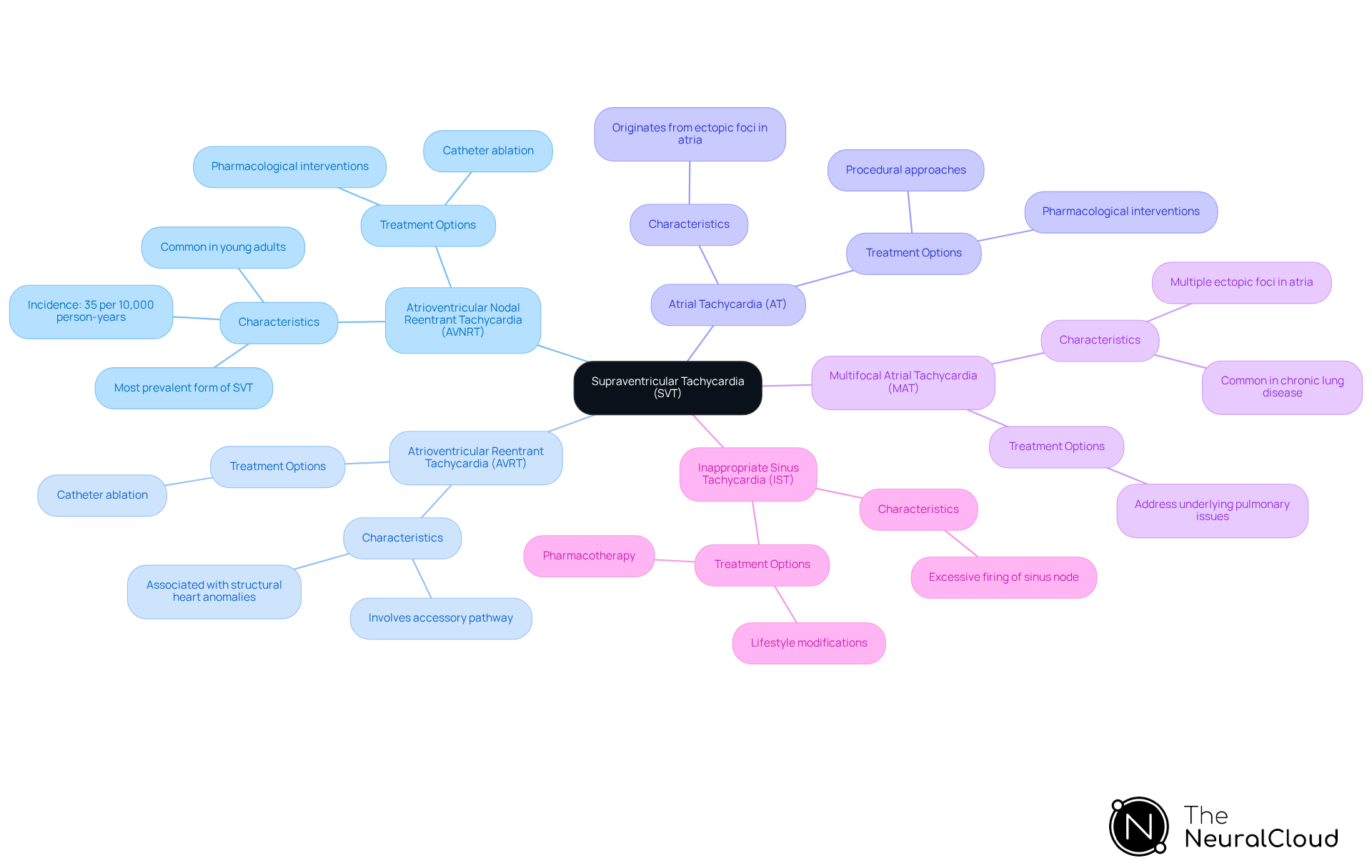
Classify Types of Supraventricular Tachycardia: A Detailed Overview
Supraventricular tachycardia (SVT) includes several distinct types, each with unique characteristics and implications for treatment. Understanding these classifications is crucial for healthcare professionals to devise appropriate diagnostic and therapeutic strategies.
Atrioventricular Nodal Reentrant Tachycardia (AVNRT) is the most prevalent form of SVT. It features a reentrant circuit within the AV node, with an incidence of approximately 35 per 10,000 person-years, translating to 2.29 cases per 1,000 individuals. This type is particularly common among young adults.
Atrioventricular Reentrant Tachycardia (AVRT) involves an accessory pathway that creates a circuit between the atria and ventricles, leading to rapid heart rates. Often associated with structural heart anomalies, AVRT can be effectively treated through catheter ablation, which has shown promising outcomes in clinical settings.
Atrial Tachycardia (AT) originates from ectopic foci in the atria, resulting in rapid atrial depolarization. Management may require a combination of pharmacological interventions and procedural approaches, depending on the individual's stability and underlying conditions.
Multifocal Atrial Tachycardia (MAT) is characterized by multiple ectopic foci in the atria and is frequently observed in individuals with chronic lung disease. Treatment often focuses on addressing the underlying pulmonary issues to mitigate episodes.
Inappropriate Sinus Tachycardia (IST) occurs when the sinus node fires excessively without a clear cause, leading to persistent tachycardia. Management strategies may include lifestyle modifications and, in some cases, pharmacotherapy.
Differentiating between these subtypes allows for tailored treatment plans that enhance outcomes and optimize resource allocation in clinical practice. As noted by experts in cardiology, this understanding is essential for improving patient care.
Diagnose Supraventricular Tachycardia: ECG Interpretation and Testing Protocols
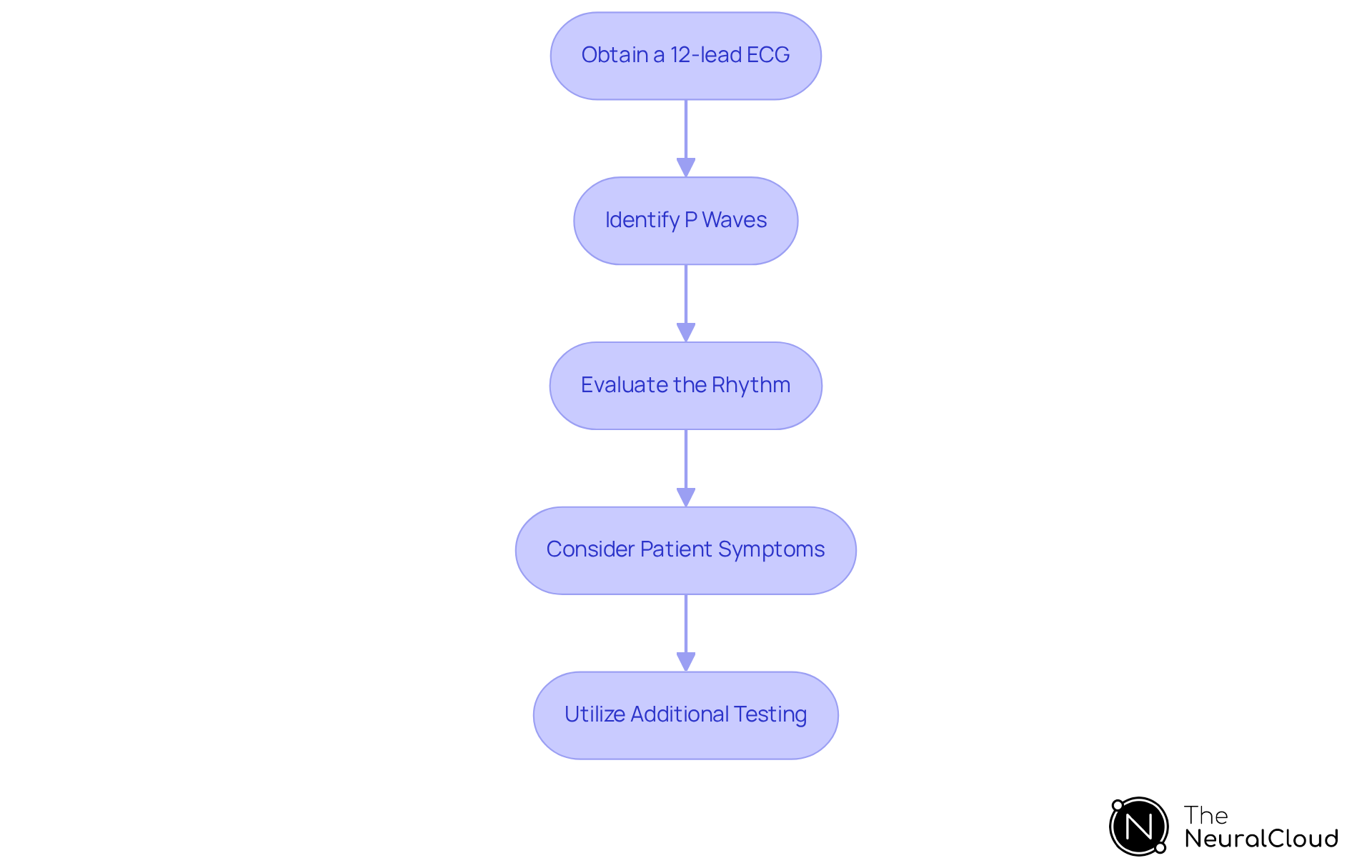
Diagnosing a supraventricular tachycardia strip requires a systematic approach to ECG interpretation, focusing on key features that guide clinical decision-making. The following steps outline the current best practices:
- Obtain a 12-lead ECG: This remains the gold standard for diagnosing SVT. Look for a narrow QRS complex (less than 120 ms) and a heart rate typically ranging from 150 to 250 beats per minute, as these findings are indicative of a supraventricular tachycardia strip.
- Identify P Waves: Assess the visibility and morphology of P waves. In atrioventricular nodal reentrant tachycardia (AVNRT), P waves may be obscured within the QRS complex, while in atrial tachycardia, they may appear distinctly before or after the QRS complex.
- Evaluate the Rhythm: Determine whether the rhythm is regular or irregular. Regular rhythms often suggest the presence of a supraventricular tachycardia strip, while irregular rhythms may indicate other underlying conditions.
- Consider Patient Symptoms: Correlate ECG findings with patient-reported symptoms such as palpitations, dizziness, or syncope. This correlation is crucial for a comprehensive evaluation of the individual's condition as shown in the supraventricular tachycardia strip.
- Utilize Additional Testing: If necessary, employ Holter monitoring or electrophysiological studies to confirm the diagnosis and evaluate the frequency of episodes. These tests can provide valuable insights into the individual's arrhythmia patterns and guide treatment options.
Incorporating advanced solutions like Neural Cloud Solutions' MaxYield™ platform can significantly enhance this process.
Features of MaxYield™:
- Noise Filtering: MaxYield™ excels in filtering out noise, ensuring clearer ECG readings.
- Distinct Wave Recognition: It allows healthcare professionals to identify previously obscured sections of lengthy Holter recordings.
Advantages for Healthcare Professionals: By utilizing MaxYield™, healthcare professionals can overcome the limitations of traditional ECG interpretation technology, which often struggles with high levels of noise and artifact. This adaptability and automation in ECG analysis address common challenges such as physiological variability and signal artifacts. Ultimately, this leads to more accurate diagnoses and effective management strategies when analyzing the supraventricular tachycardia strip.
Manage Supraventricular Tachycardia: Treatment Approaches and Clinical Guidelines
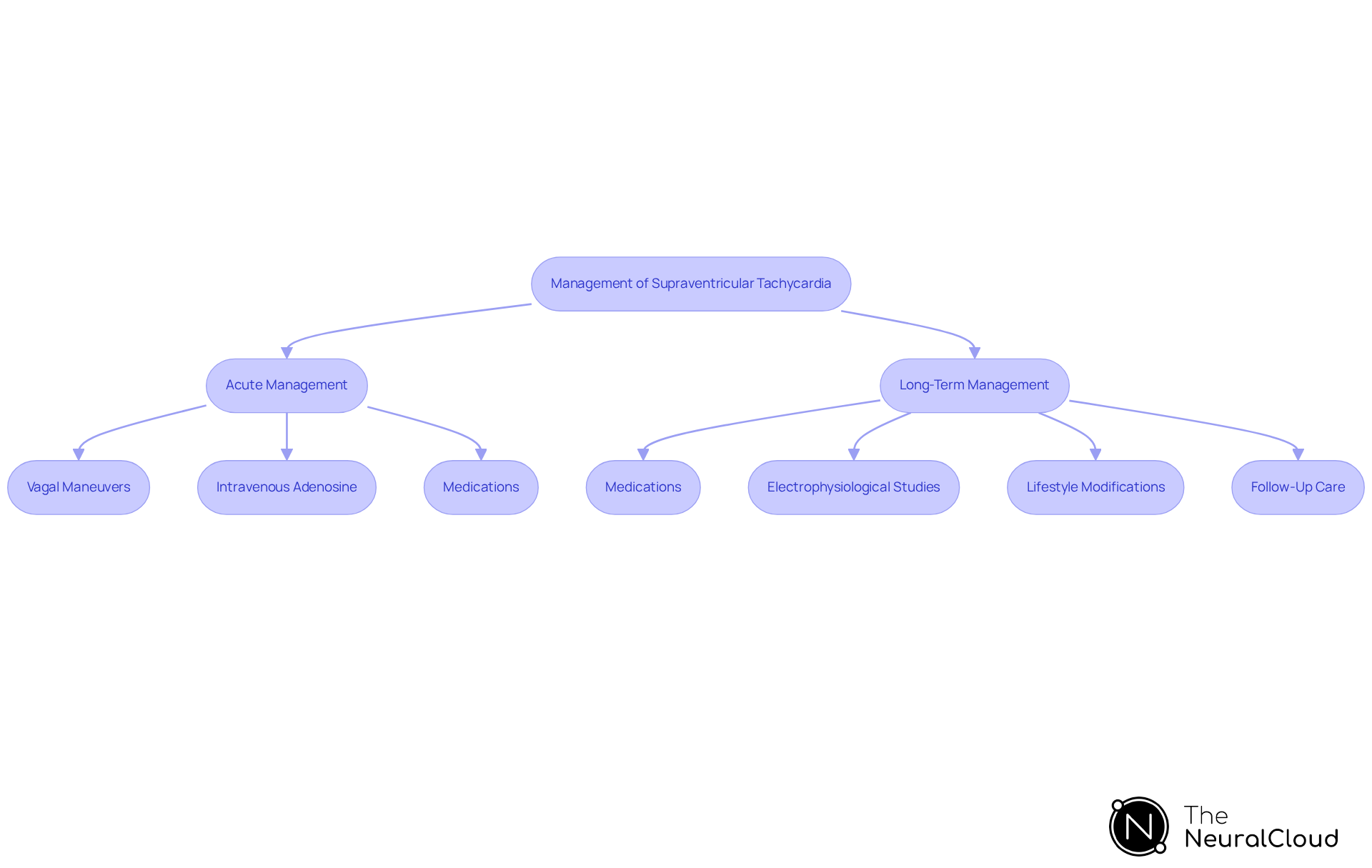
Management of a supraventricular tachycardia strip involves both acute and long-term strategies that are essential for effective treatment.
Acute Management: For stable individuals experiencing an episode, vagal maneuvers, such as the Valsalva maneuver, can be attempted to terminate the episode. If these maneuvers are ineffective, intravenous adenosine is often administered to restore normal rhythm.
Medications: Beta-blockers and calcium channel blockers are commonly prescribed for rate control and rhythm management. In cases where episodes occur frequently, antiarrhythmic medications may be indicated to help manage the condition more effectively.
Electrophysiological Studies: For individuals with recurrent SVT, the supraventricular tachycardia strip may suggest that catheter ablation is a curative option, particularly for types like AV nodal reentrant tachycardia (AVNRT) and atrioventricular reentrant tachycardia (AVRT).
Lifestyle Modifications: Patients should be advised on lifestyle changes that can help manage their condition. This includes reducing caffeine intake, managing stress, and avoiding known triggers that may precipitate episodes.
Follow-Up Care: Regular follow-up appointments are essential to monitor the effectiveness of treatment and make necessary adjustments to the management plan.
Adhering to clinical guidelines ensures that patients receive optimal care tailored to their specific needs.
Conclusion
Understanding and mastering supraventricular tachycardia (SVT) is crucial for healthcare professionals, as it encompasses a variety of rapid heart rhythms originating above the ventricles. This article provided a comprehensive tutorial on SVT, detailing its definitions, mechanisms, types, diagnostic protocols, and management strategies. By thoroughly grasping these elements, practitioners can enhance their ability to recognize and effectively treat this condition, ultimately improving patient outcomes.
Key insights discussed include the various types of SVT, such as:
- Atrioventricular nodal reentrant tachycardia (AVNRT)
- Atrial tachycardia
Each requiring specific diagnostic and treatment approaches. The importance of accurate ECG interpretation and the role of advanced diagnostic tools like Neural Cloud Solutions' MaxYield™ were emphasized, showcasing how technology can aid in isolating and analyzing critical cardiac signals. Additionally, the article highlighted the significance of tailored management plans that incorporate both acute interventions and long-term lifestyle modifications.
The knowledge gained from this tutorial is not just academic; it has real-world implications for patient care. By applying these insights and utilizing effective diagnostic tools, healthcare professionals can significantly improve their diagnostic accuracy and treatment efficacy for patients experiencing SVT. Engaging with this material not only enhances clinical skills but also underscores the importance of continuous learning in the ever-evolving field of cardiology.
Frequently Asked Questions
What is supraventricular tachycardia (SVT)?
Supraventricular tachycardia (SVT) refers to various rapid heart rhythms that originate from above the ventricles, specifically within the atria or the atrioventricular (AV) node, leading to heart rates exceeding 100 beats per minute in adults.
What heart rates are typically associated with SVT in children?
In children, SVT heart rates can range from 180 to 220 beats per minute.
What are the common causes of SVT?
SVT can result from several factors, including reentrant circuits, ectopic foci, or enhanced automaticity.
What symptoms might indicate the presence of SVT?
Symptoms of SVT may include palpitations, dizziness, and potential hemodynamic instability.
How prevalent is SVT in the population?
Approximately 35 individuals per 100,000 experience SVT, with a notable prevalence among those aged 45 to 64 years.
Can individuals with SVT be asymptomatic?
Yes, many individuals with SVT remain asymptomatic, while others may experience severe symptoms that require urgent medical attention.
What is the heart rate typically seen in atrioventricular nodal reentrant tachycardia (AVNRT)?
In cases of AVNRT, the heart rate typically reaches around 180 to 220 beats per minute.
How is SVT diagnosed?
Diagnostic approaches for SVT often involve Holter monitors or event recorders to capture infrequent episodes that may not be evident on a standard 12-lead ECG.
What is the recommended treatment for individuals with hemodynamic instability due to SVT?
Synchronized cardioversion is recommended for individuals with hemodynamic instability.
What features does Neural Cloud Solutions' MaxYield™ offer for diagnosing SVT?
MaxYield™ automates ECG analysis, maps signals through noise to isolate and label key features in every heartbeat, and rapidly analyzes 200,000 heartbeats in less than 5 minutes.
What characterizes a supraventricular tachycardia strip on an ECG?
A supraventricular tachycardia strip is characterized by a narrow QRS complex of less than 120 ms and an elevated heart rate.






