Introduction
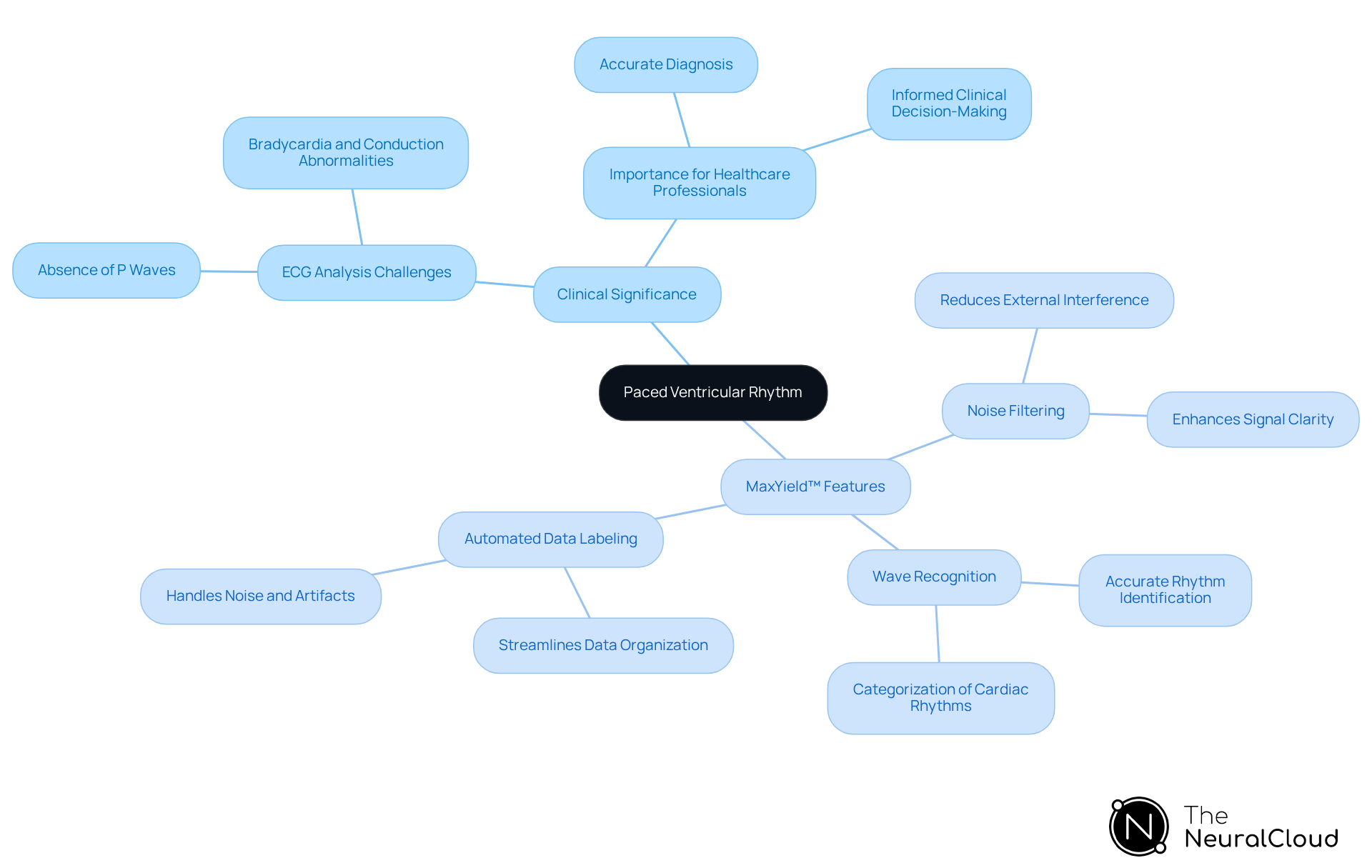
Understanding paced ventricular rhythm is crucial for healthcare professionals navigating the complexities of cardiac care, particularly as the prevalence of implanted cardiac devices continues to rise. This article delves into the significance of this unique cardiac pattern, highlighting the challenges faced in ECG analysis. It also examines the technological advancements that enhance ECG analysis and outlines essential features developers must consider to improve patient outcomes.
As health tech innovations evolve, they must effectively address the challenges posed by paced ventricular rhythm. Accurate diagnosis and management in clinical settings are paramount, and advancements in technology play a vital role in achieving this goal. By focusing on the features of these innovations, we can better understand their advantages and the direct benefits they offer to healthcare professionals.
Define Paced Ventricular Rhythm and Its Clinical Significance
Paced ventricular rhythm presents a unique challenge in ECG analysis, as it signifies a cardiac pattern where electrical impulses stem from a device rather than the heart's natural conduction system. This condition is characterized by the absence of intrinsic atrial activity, leading to a lack of P waves on the ECG. Understanding paced ventricular rhythm is crucial for healthcare professionals, especially when it arises due to bradycardia or other conduction abnormalities.
The MaxYield™ platform from Neural Cloud Solutions addresses these challenges by offering advanced features that enhance ECG analysis. Key features include:
- Noise Filtering: Reduces interference from external sources, allowing for clearer signal interpretation.
- Wave Recognition: Accurately identifies and categorizes various cardiac rhythms, including PVA.
- Automated Data Labeling: Streamlines the process of data organization, even in recordings with significant noise and artifacts.
These features translate into significant advantages for healthcare professionals. By improving the accuracy and efficiency of ECG analysis, MaxYield™ ensures that devices can reliably detect and interpret paced ventricular rhythm in individuals with implanted cardiac devices. This technological advancement not only enhances diagnostic yield but also supports confident clinical decision-making.
Moreover, the continuous learning model integrated into MaxYield™ allows the platform to evolve over time, addressing traditional limitations in ECG interpretation. As a result, healthcare professionals can rely on this innovative solution to provide better patient care and outcomes.
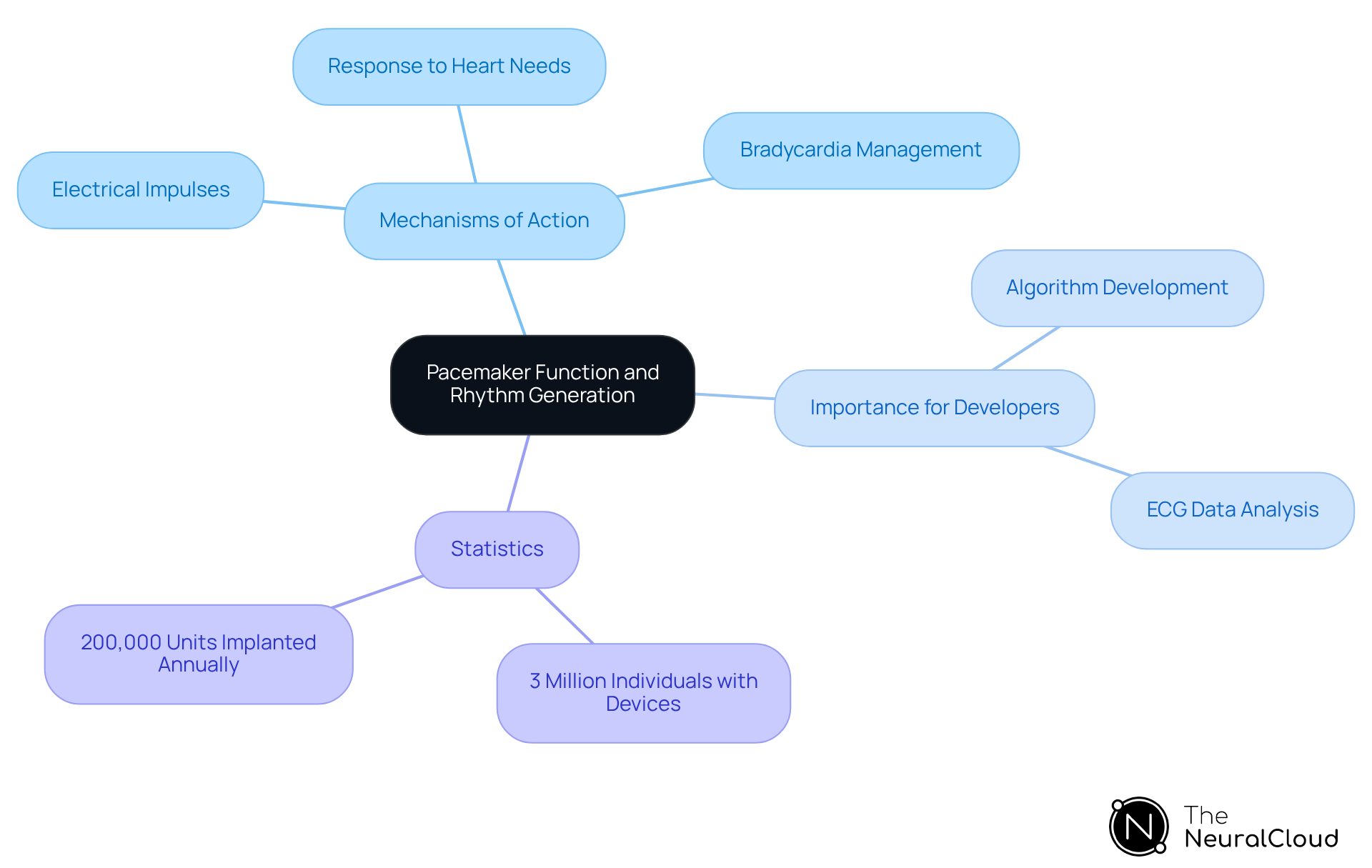
Explain Mechanisms of Pacemaker Function and Rhythm Generation
Pacemakers function by delivering electrical impulses to the heart muscle, stimulating contractions that maintain an adequate heart rate. These advanced devices can be programmed to respond to the heart's physiological needs, adjusting the pacing rate as required. The primary mechanism involves sensing the heart's intrinsic electrical activity and providing stimulation when natural impulses fall short. This capability is crucial for individuals with bradycardia or other conduction disorders, ensuring stable cardiac output.
For health technology developers, grasping these mechanisms is essential for creating algorithms that accurately analyze ECG data from patients with heart devices. This knowledge not only boosts diagnostic reliability but also enhances monitoring, ultimately leading to improved healthcare outcomes. Recent advancements in cardiac rhythm management technology, such as the FDA-approved dual-chamber leadless device, showcase the ongoing evolution in this field, prioritizing patient safety and comfort.
Statistics reveal that around 3 million individuals in the U.S. currently live with a cardiac device, with approximately 200,000 units implanted each year for conditions like bradycardia. As the demand for cardiac pacing rises, driven by an aging population, the development of innovative algorithms for ECG interpretation becomes increasingly essential.
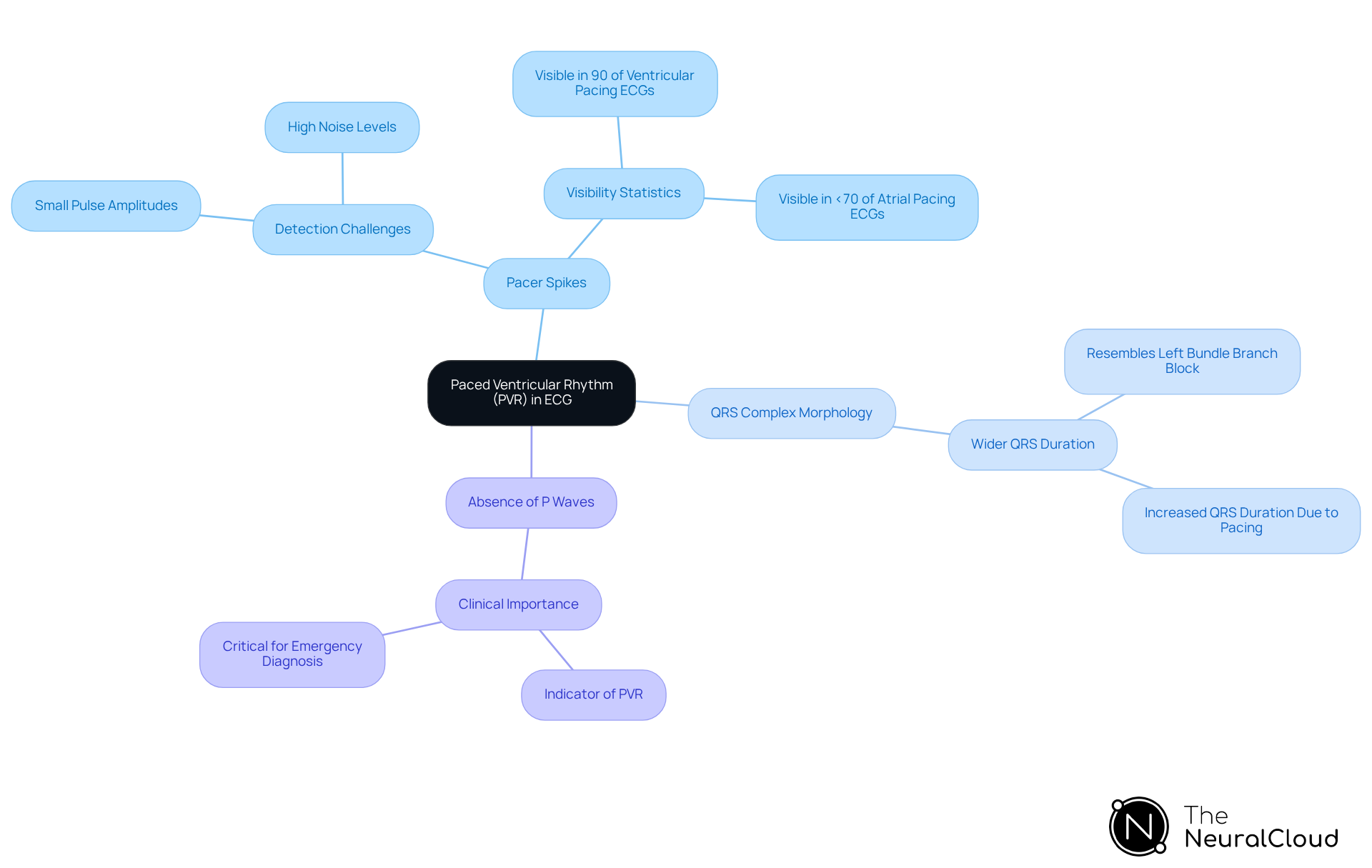
Identify Paced Ventricular Rhythm in ECG Readings: Key Features and Interpretation
Paced ventricular rhythm presents unique challenges in ECG analysis, particularly with the advent of modern bipolar pacemakers. Identifying the paced ventricular rhythm (PVR) on an ECG requires careful attention to several key features, especially when leveraging advanced technologies like Neural Cloud Solutions' MaxYield™ platform.
-
Pacer Spikes: One of the primary indicators of PVR is the presence of pacer spikes, which are vertical lines appearing before each QRS complex. These spikes signify the timing of the pacemaker's electrical impulses. However, detecting these spikes has become increasingly difficult due to the small pulse amplitudes produced by contemporary bipolar pacemakers. MaxYield™ excels in identifying these subtle signals, even amidst high levels of noise and artifact. Research shows that visible atrial stimulation artifacts are present in less than 70% of ECGs, while ventricular stimulation generates visible pace spikes in about 90% of ECGs. This highlights the critical need for accurate detection of these changes.
-
In paced ventricular rhythm, the QRS complexes are typically wider than normal, often resembling left bundle branch block morphology. This widening occurs because pacing alters the conduction pathway, resulting in an increased QRS duration. MaxYield™'s advanced noise filtering capabilities ensure that these essential features are accurately detected, even in challenging recording conditions.
-
Absence of P Waves: Another significant characteristic of PVR is the absence of P waves, as the atria are not activated by intrinsic impulses. This absence serves as a crucial indicator for clinicians interpreting ECGs, particularly in emergency situations where timely diagnosis of paced ventricular rhythm is vital. The adaptive algorithms of MaxYield™ continuously learn and improve, enhancing the precision of P wave detection and overall pattern interpretation.
For health tech developers, integrating algorithms capable of detecting these features is essential for accurate rhythm interpretation. Algorithms like those in MaxYield™ enhance the reliability of data provided to clinicians, ultimately improving evaluations and patient outcomes. The sensitivity of manual ECG interpretation for ventricular pacing has been reported as moderate, with Reader 1 at 0.88 and Reader 2 at 0.93. This underscores the necessity for advanced detection methods to support clinical decision-making. As noted by Joel T Levis, applying Sgarbossa criteria is vital for timely diagnosis in individuals with VPRs and acute myocardial infarction (AMI).
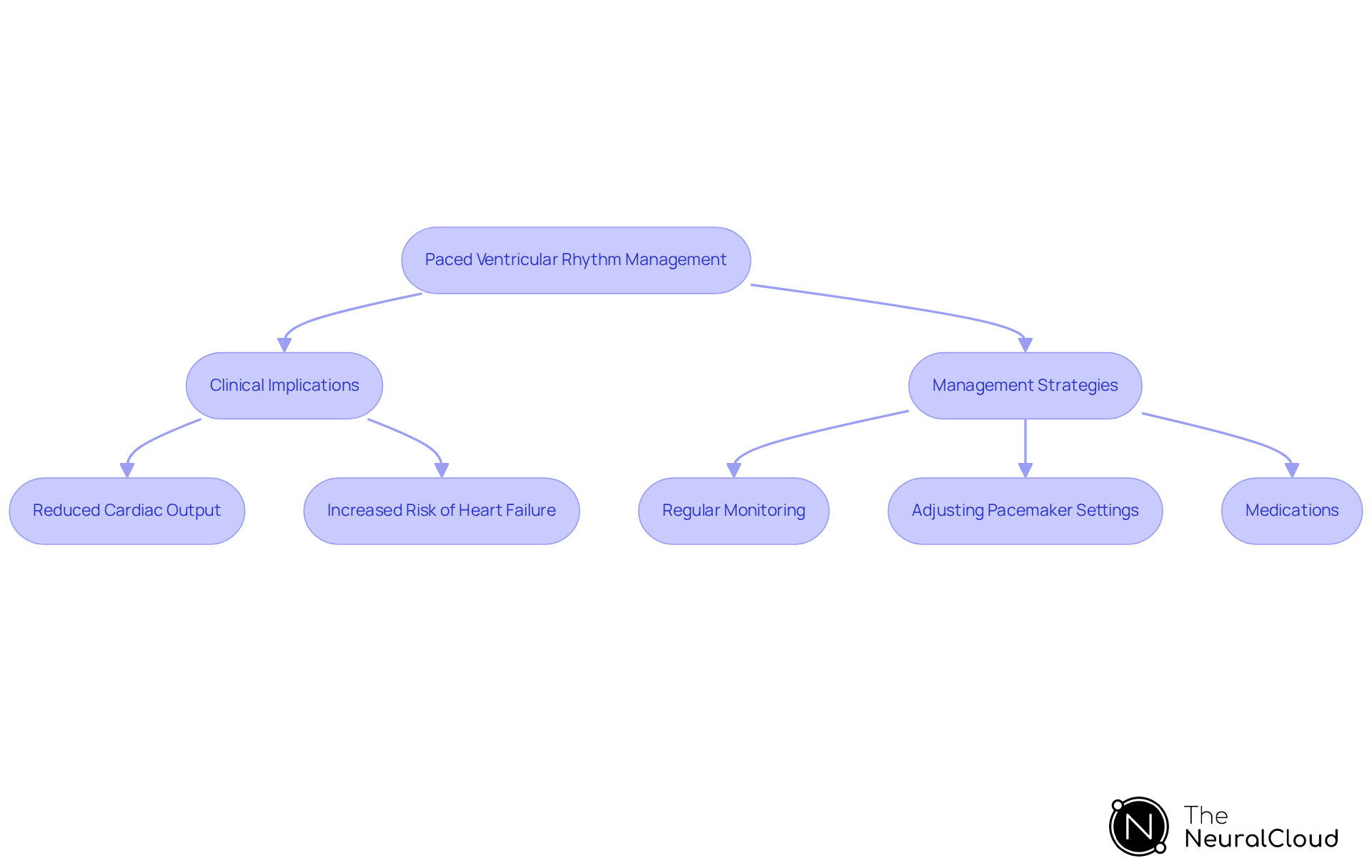
Discuss Clinical Implications and Management Strategies for Paced Ventricular Rhythm
The clinical implications of paced ventricular rhythm are significant. Patients experiencing paced ventricular rhythm (PVR) may face various complications, such as reduced cardiac output and an increased risk of heart failure. Effective management strategies typically involve:
- Regular monitoring of the rhythm function
- Adjusting pacemaker settings as necessary
Additionally, clinicians might consider medications to optimize heart function and prevent complications associated with chronic stimulation.
For health tech developers, integrating features that allow for real-time monitoring and alerts regarding pacing function can greatly enhance safety and improve clinical outcomes. Such capabilities not only provide immediate feedback but also empower healthcare providers to respond swiftly to any issues that arise. Furthermore, including educational resources within the technology can equip healthcare professionals with the knowledge needed to make informed decisions about patient management.
In summary, addressing the challenges associated with paced ventricular rhythm through innovative technology and comprehensive management strategies can lead to better patient outcomes. By focusing on both the clinical implications and the potential for technological advancements, we can ensure that healthcare providers are well-prepared to navigate the complexities of patient care.
Conclusion
Understanding paced ventricular rhythm is crucial for healthcare professionals and health tech developers, as it signifies a notable shift from the heart's natural conduction system. This condition, characterized by the lack of intrinsic atrial activity and the presence of pacer spikes, presents distinct challenges in ECG interpretation. The MaxYield™ platform addresses these challenges by offering innovative solutions that enhance the accuracy and reliability of ECG analysis, ultimately leading to improved patient care.
Key insights emphasize the significance of recognizing pacemaker function mechanisms and the specific ECG features linked to paced ventricular rhythm. The MaxYield™ platform integrates advanced algorithms and continuous learning models, significantly boosting diagnostic capabilities. This ensures that healthcare providers can make informed decisions swiftly, which is increasingly vital given the rising prevalence of cardiac devices. The need for sophisticated tools to interpret ECG data has never been more pressing.
Reflecting on the broader implications, the intersection of clinical knowledge and technological innovation is essential for tackling the complexities of paced ventricular rhythm. By prioritizing advancements in health tech, developers can empower clinicians to enhance patient outcomes and streamline management strategies. Ongoing education and real-time monitoring are crucial for further improving the safety and efficacy of care for individuals living with paced ventricular rhythm.
Frequently Asked Questions
What is paced ventricular rhythm?
Paced ventricular rhythm is a cardiac pattern where electrical impulses originate from a device rather than the heart's natural conduction system, characterized by the absence of intrinsic atrial activity and a lack of P waves on the ECG.
Why is understanding paced ventricular rhythm important for healthcare professionals?
Understanding paced ventricular rhythm is crucial for healthcare professionals, particularly when it occurs due to bradycardia or other conduction abnormalities, as it presents unique challenges in ECG analysis.
What challenges does paced ventricular rhythm present in ECG analysis?
The main challenge is the absence of P waves, which complicates the interpretation of the ECG and can lead to difficulties in diagnosing underlying cardiac conditions.
What is the MaxYield™ platform and how does it help with ECG analysis?
The MaxYield™ platform from Neural Cloud Solutions offers advanced features that enhance ECG analysis, including noise filtering, wave recognition, and automated data labeling, which improve the accuracy and efficiency of detecting paced ventricular rhythm.
What are the key features of the MaxYield™ platform?
Key features include: - Noise Filtering: Reduces interference from external sources for clearer signal interpretation. - Wave Recognition: Accurately identifies and categorizes various cardiac rhythms. - Automated Data Labeling: Streamlines data organization, even in recordings with noise and artifacts.
How do the features of MaxYield™ benefit healthcare professionals?
These features enhance the accuracy and efficiency of ECG analysis, enabling reliable detection and interpretation of paced ventricular rhythm, which supports confident clinical decision-making and improves diagnostic yield.
How does the continuous learning model of MaxYield™ benefit ECG interpretation?
The continuous learning model allows the platform to evolve over time, addressing traditional limitations in ECG interpretation, thereby improving patient care and outcomes.






