Introduction
Second-Degree Type 1 Heart Block, commonly referred to as Mobitz Type I, poses a distinct challenge in cardiac care due to its subtle yet significant implications for patient health. Understanding its characteristics and mechanisms is crucial for healthcare professionals, as it can often be benign but may occasionally lead to serious complications. Clinicians face the task of effectively navigating the complexities of diagnosis and management in a landscape where advanced technologies promise to enhance accuracy and patient outcomes.
This article explores the intricacies of this condition, focusing on its diagnosis and management strategies. It also highlights the role of innovative ECG analysis tools, such as the MaxYield™ platform, which aims to improve ECG interpretation. By examining the features of MaxYield™, healthcare professionals can gain insights into how this platform enhances ECG analysis, ultimately benefiting patient care.
Define Second-Degree Type 1 Heart Block: Key Characteristics and Mechanisms
Second-Degree Type 1 Heart Block, also referred to as Mobitz Type I or the Wenckebach phenomenon, is characterized by a progressive prolongation of the PR interval on the ECG until a P wave fails to conduct to the ventricles, resulting in a dropped beat. This occurs due to a temporary obstruction in the conduction system, primarily at the second degree type 1 heart block within the atrioventricular (AV) node. The underlying mechanism of second degree type 1 heart block involves a gradual increase in the time needed for electrical impulses to travel from the atria to the ventricles, ultimately leading to conduction failure.
Recent studies suggest that the second degree type 1 heart block is often benign, typically seen in individuals with high vagal tone or during sleep, and is usually asymptomatic. This underscores its generally favorable prognosis. Clinicians must recognize these characteristics to effectively differentiate the first type from more severe variations of heart obstruction, including second degree type 1 heart block and third-degree AV obstruction. For instance, the Wenckebach pattern typically exhibits a P:QRS ratio of 3:2 or 4:3, illustrating the cyclical nature of the interruption.
Understanding these nuances is crucial for accurate diagnosis and treatment, as the first variant is generally associated with a low risk of progressing to conditions like second degree type 1 heart block. The integration of Neural Cloud Solutions' MaxYield™ platform addresses the challenges in ECG analysis by enhancing the clarity of recordings affected by noise and artifacts.
Features of MaxYield™:
- Sophisticated noise filtering technology
- Advanced wave recognition capabilities
- Rapid isolation of critical data even in challenging conditions
Advantages for Healthcare Professionals:
- Enables precise diagnosis of heart rhythm disturbances
- Enhances patient care through improved ECG analysis
- Facilitates better management of cardiac conditions
This innovative platform ensures that clinicians can accurately diagnose and manage heart rhythm disturbances, ultimately leading to improved patient outcomes.

Identify Clinical Features and Diagnostic Criteria for Mobitz Type I
Individuals with second degree type 1 heart block can exhibit a variety of symptoms, ranging from being asymptomatic to experiencing fainting, dizziness, or heart fluttering. The diagnostic criteria primarily rely on ECG analysis, where the key feature is the progressive lengthening of the PR interval, ultimately leading to a non-conducted P wave. This occurrence, commonly known as the Wenckebach phenomenon, is crucial for differentiating Mobitz Type I from other types of heart block that may necessitate more intensive intervention.
Clinicians should evaluate the individual's clinical history, including medication use and any pre-existing cardiac conditions, as these factors can significantly influence the presentation and management of the condition. For asymptomatic individuals, regular monitoring is typically adequate; however, those exhibiting symptoms may require further diagnostic assessment and tailored management strategies. Notably, research indicates that over two-thirds of unmonitored individuals with second degree type 1 heart block experienced adverse outcomes within five years, underscoring the importance of diligent oversight and timely intervention.
Recognizing these clinical features is vital for effective diagnosis and treatment planning. By understanding the nuances of second degree type 1 heart block, healthcare professionals can enhance patient care and improve outcomes.

Explore Management and Treatment Approaches for Second-Degree Type 1 Heart Block
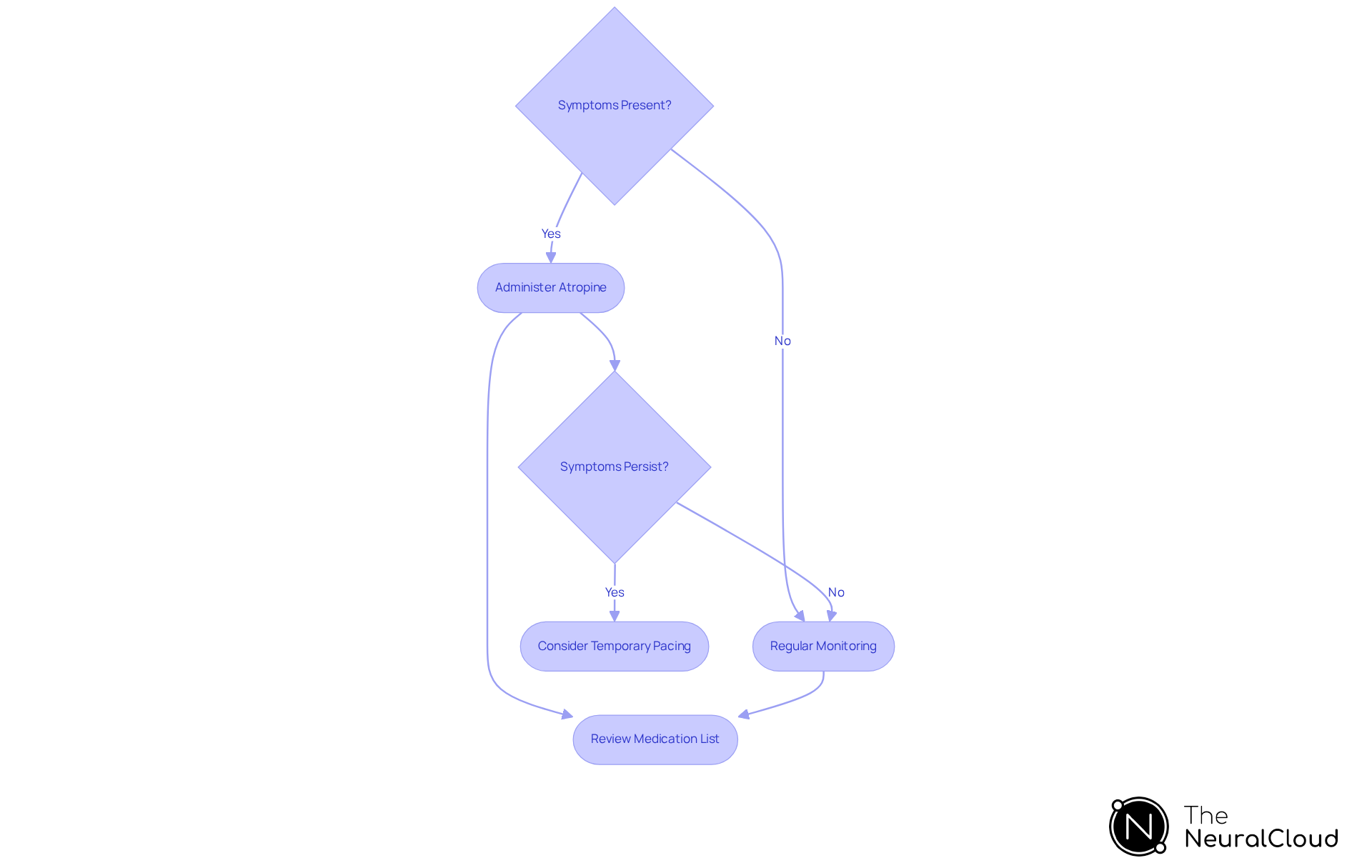
Management of Mobitz Type I primarily involves careful monitoring and addressing any reversible causes of the heart block. Asymptomatic individuals generally do not require specific treatment; however, regular follow-up is essential to ensure stability. For those exhibiting symptoms, atropine is often the first-line intervention, effectively increasing heart rate and enhancing conduction. In cases where symptoms persist or escalate, temporary pacing may be warranted to stabilize the individual.
A thorough review of the individual's medication list is crucial, as certain drugs, including beta-blockers and digoxin, can exacerbate the condition. Adapting the management strategy to the specific clinical situation of each individual is vital, ensuring that the risks and benefits of any intervention are thoughtfully balanced. Real-world examples demonstrate that symptomatic patients typically respond well to atropine, with many experiencing significant improvement in their condition.
Importantly, second degree type 1 heart block is unlikely to require treatment unless symptoms are evident, as indicated by specialists. Additionally, it is essential to recognize that while Mobitz type I is often benign, there is a chance of progression to second degree type 1 heart block and more serious types of AV block, underscoring the need for vigilant monitoring. Regular follow-up for asymptomatic individuals remains crucial to address any potential reversible causes.
Utilize Advanced ECG Analysis Technologies for Enhanced Diagnosis and Management
ECG analysis often faces significant challenges, particularly in accurately diagnosing conditions such as second degree type 1 heart block. Traditional methods can be hindered by noise and signal artifacts, which obscure true cardiac signals and complicate interpretation. This is where advanced technologies, such as Neural Cloud Solutions' MaxYield™ platform, come into play.
The MaxYield™ platform utilizes sophisticated AI algorithms to automate ECG data analysis. This technology enables rapid and precise identification of critical features, including PR interval prolongation and dropped beats. With the ability to process over 200,000 heartbeats in under five minutes, clinicians gain swift access to reliable cardiac insights, facilitating informed decision-making.
Key features of the MaxYield™ platform include:
- Automated ECG Data Analysis: Reduces the time spent on manual interpretation.
- Rapid Processing: Analyzes over 200,000 heartbeats quickly, providing timely insights.
- Noise and Artifact Reduction: Enhances signal clarity for more accurate diagnoses.
These features translate into significant advantages for healthcare professionals. By streamlining the analysis process, clinicians can focus on high-level decision-making rather than labor-intensive manual tasks. This shift not only improves efficiency but also leads to better patient outcomes. Feedback from cardiologists highlights the platform's potential to revolutionize ECG interpretation, enhancing clinical workflows and diagnostic accuracy.

Conclusion
Second-Degree Type 1 Heart Block, also known as Mobitz Type I or the Wenckebach phenomenon, is a significant aspect of cardiac health that necessitates careful understanding and management. This condition is marked by a progressive lengthening of the PR interval, which can lead to occasional dropped beats. It often presents benignly, particularly in individuals with high vagal tone. Recognizing its unique features is crucial for healthcare professionals to distinguish it from more severe forms of heart block and to provide appropriate care.
In the context of ECG analysis, challenges often arise in accurately diagnosing heart conditions. The MaxYield™ platform from Neural Cloud Solutions addresses these challenges by enhancing diagnostic accuracy through advanced technology. Key features of the MaxYield™ platform include:
- Real-time data analysis
- User-friendly interfaces
- Integration with existing healthcare systems
These features not only streamline the diagnostic process but also empower healthcare professionals to make informed decisions quickly.
The advantages of utilizing the MaxYield™ platform are substantial. By improving ECG analysis, healthcare providers can deliver precise and timely care, ultimately leading to better patient outcomes. For asymptomatic individuals, minimal intervention may be required, while those exhibiting symptoms can benefit from targeted treatments such as atropine or temporary pacing. Regular monitoring remains essential, especially given the potential for progression to more serious heart conditions.
Ultimately, the effective diagnosis and management of Second-Degree Type 1 Heart Block depend on a combination of clinical expertise and innovative technology. As advancements in ECG analysis continue to emerge, healthcare professionals are better equipped to navigate the complexities of cardiac health. Emphasizing the importance of ongoing education and adaptation to new technologies will ensure that clinicians remain at the forefront of managing this condition effectively.
Frequently Asked Questions
What is Second-Degree Type 1 Heart Block?
Second-Degree Type 1 Heart Block, also known as Mobitz Type I or the Wenckebach phenomenon, is characterized by a progressive prolongation of the PR interval on the ECG until a P wave fails to conduct to the ventricles, resulting in a dropped beat.
What causes Second-Degree Type 1 Heart Block?
It occurs due to a temporary obstruction in the conduction system, primarily at the atrioventricular (AV) node, leading to a gradual increase in the time needed for electrical impulses to travel from the atria to the ventricles, ultimately causing conduction failure.
Is Second-Degree Type 1 Heart Block serious?
Recent studies suggest that Second-Degree Type 1 Heart Block is often benign, typically seen in individuals with high vagal tone or during sleep, and is usually asymptomatic, indicating a generally favorable prognosis.
How can clinicians differentiate Second-Degree Type 1 Heart Block from other heart block types?
Clinicians must recognize the characteristics of Second-Degree Type 1 Heart Block, such as the P:QRS ratio of 3:2 or 4:3, which illustrates the cyclical nature of the interruption, to effectively differentiate it from more severe variations like third-degree AV obstruction.
What is the role of the MaxYield™ platform in ECG analysis?
The MaxYield™ platform addresses challenges in ECG analysis by enhancing the clarity of recordings affected by noise and artifacts, enabling precise diagnosis of heart rhythm disturbances.
What features does the MaxYield™ platform offer?
MaxYield™ features sophisticated noise filtering technology, advanced wave recognition capabilities, and rapid isolation of critical data even in challenging conditions.
How does MaxYield™ benefit healthcare professionals?
It enhances patient care through improved ECG analysis, facilitates better management of cardiac conditions, and enables precise diagnosis of heart rhythm disturbances, ultimately leading to improved patient outcomes.






