Introduction
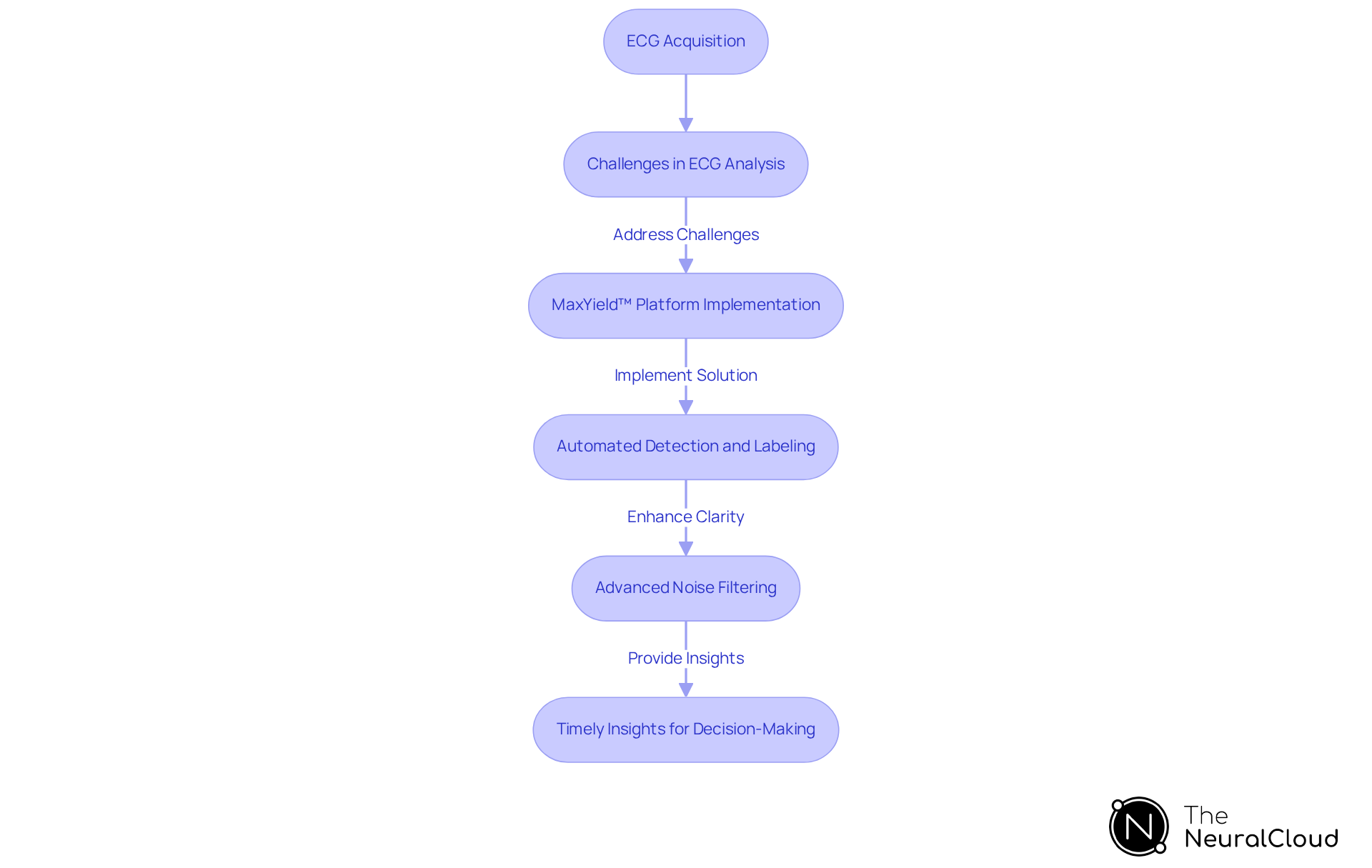
Understanding EKG rhythms is crucial for health tech developers, as these patterns form the foundation for diagnosing various cardiac conditions. However, ECG analysis presents challenges that can hinder timely and accurate diagnosis. With advancements in technology, platforms like Neural Cloud Solutions' MaxYield™ are transforming how ECG data is analyzed. This platform offers rapid and accurate insights that significantly enhance patient care.
MaxYield™ features advanced algorithms that streamline ECG data interpretation, allowing healthcare professionals to identify critical heart rhythms more efficiently. By automating the analysis process, the platform reduces the potential for human error and increases diagnostic accuracy. This not only saves time but also improves patient outcomes by ensuring that critical conditions are recognized and addressed promptly.
The advantages of using MaxYield™ extend beyond just efficiency. Healthcare professionals benefit from enhanced decision-making capabilities, as the platform provides comprehensive data visualizations and real-time alerts. These features empower clinicians to make informed decisions quickly, ultimately leading to better patient management.
This article explores ten essential EKG rhythms that every health tech developer should master, highlighting their significance in clinical practice and the role of innovative technology in improving outcomes.
Neural Cloud Solutions MaxYield™: Advanced ECG Analysis for Healthcare Professionals
ECG analysis presents several challenges, including the time-consuming process of detecting and labeling essential heart features. The 'Neural Cloud Solutions' MaxYield™ platform addresses these issues by automating this process, significantly improving efficiency and accuracy.
MaxYield™ utilizes advanced AI algorithms to process over 200,000 heartbeats in under five minutes. This rapid analysis provides healthcare professionals with timely and reliable insights, allowing for quicker decision-making in clinical settings. The platform is compatible with various ECG devices, ensuring scalability and adaptability across different healthcare environments.
One of the standout features of MaxYield™ is its advanced noise filtering capabilities. These effectively eliminate noise categories that can obscure critical cardiac events, enhancing the clarity of ECG signals. This makes the platform an indispensable tool for cardiologists and health tech developers alike.
Case studies have shown that the AI-ECG group reduced the time from ECG acquisition to cath lab arrival to an average of 43.3 minutes, compared to 52.3 minutes for standard care. This improvement greatly enhances outcomes for patients. Furthermore, MaxYield™ transforms noisy recordings into detailed insights, supporting confident clinical decision-making.
As Dr. Chin-Sheng Lin noted, the ECG AI reader's ability to quickly interpret ECG data not only enhances diagnostic accuracy but also optimizes resource allocation. This ultimately leads to improved patient care and outcomes.
Sinus Rhythm: The Foundation of EKG Interpretation
Sinus rhythm is characterized by a regular heart rate of 60 to 100 beats per minute, initiated by the sinoatrial (SA) node. On an ECG, this rhythm features distinct P waves preceding each QRS complex, creating a consistent pattern. Identifying basic EKG rhythms is crucial for health tech developers, as it serves as the baseline for diagnosing arrhythmias and other heart conditions. Deviations from this rhythm can indicate underlying health issues that require further evaluation.
In 2025, the significance of maintaining normal sinus rhythm (NSR) is highlighted by its link to improved cardiac health outcomes. Research indicates that individuals spend an average of 38.2% of their days entirely in NSR, underscoring the rhythm's stability and its vital role in overall heart health. This statistic suggests that a substantial amount of time spent in NSR correlates with better health outcomes, reinforcing the need for effective monitoring technologies.
The sinoatrial node generates 100 to 110 action potentials per minute, reflecting the heart's natural pacing mechanism. This intrinsic activity is essential for sustaining a stable heart rhythm. Any dysfunction in the SA node can lead to abnormal rhythms, which are considered basic EKG rhythms, such as sinus bradycardia or tachycardia, and may necessitate clinical attention.
Real-world applications of sinus rhythm monitoring technology, such as wearable ECG devices integrated with advanced systems, have transformed patient care by enabling continuous monitoring and early detection of arrhythmias. Key features of these systems include:
- Mapping ECG signals through noise
- Isolating and labeling key features in every heartbeat
- Delivering beat-by-beat analysis of up to 200,000 heartbeats in less than 5 minutes
These features empower healthcare professionals to make timely interventions. As specialists emphasize, understanding and tracking sinus rhythm is essential for effective cardiac health management. Utilizing advanced systems can significantly enhance diagnostic precision and workflow efficiency.

Atrial Fibrillation: Key Characteristics and Management Strategies
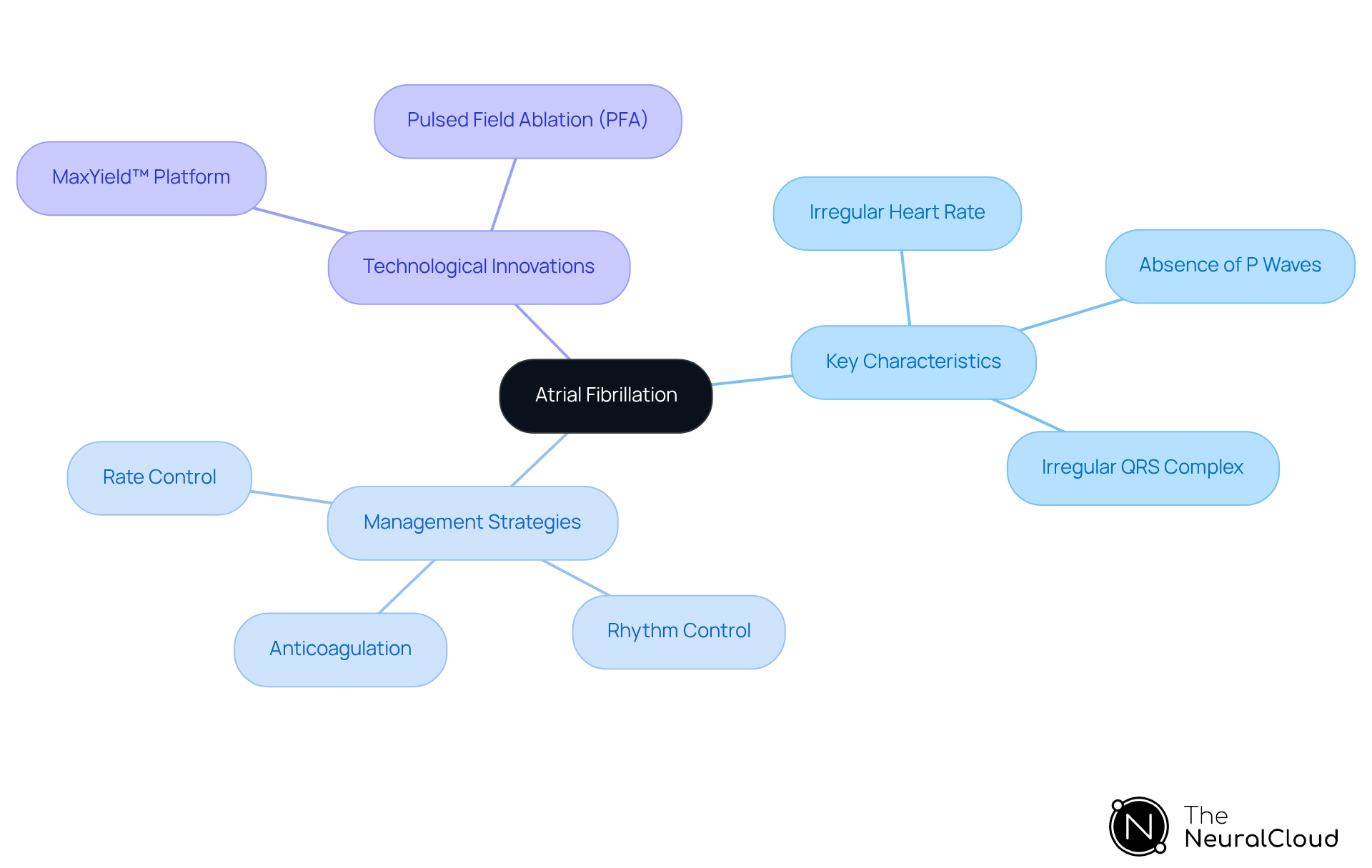
Atrial fibrillation (AF) presents significant challenges in ECG analysis due to its irregular and often rapid heart rate, which leads to ineffective atrial contractions. On an ECG, AF is characterized by the absence of distinct P waves and an irregularly irregular QRS complex. Effective management strategies include:
- Rate control
- Rhythm control
- Anticoagulation to reduce the risk of thromboembolic events
Recent studies show that focusing on heart rhythm treatment can lower the risk of stroke by 23% and decrease the risk of dying from cardiovascular disease by 32%.
For health tech developers, integrating advanced algorithms that accurately detect AF is essential for enhancing patient outcomes and improving ECG analysis platforms. The MaxYield™ platform exemplifies this innovation, featuring advanced noise reduction and artifact handling to ensure clarity in ECG readings, even under challenging conditions. Its capabilities include salvaging previously obscured sections of lengthy Holter, 1-Lead, and patch monitor recordings. Additionally, automated signal labeling and adaptive algorithms significantly enhance diagnostic yield, making it an invaluable tool for healthcare professionals.
Technologies like pulsed field ablation (PFA) further illustrate modern approaches to streamline AF treatment. PFA employs ultra-fast electrical pulses to target and destroy abnormal heart cells while minimizing damage to surrounding tissue, offering a safer and faster alternative to traditional methods. As the landscape of AF management evolves, the emphasis on precise ECG detection algorithms, such as those provided by MaxYield™, becomes increasingly vital for optimizing care.
Ventricular Tachycardia: Identification and Clinical Implications
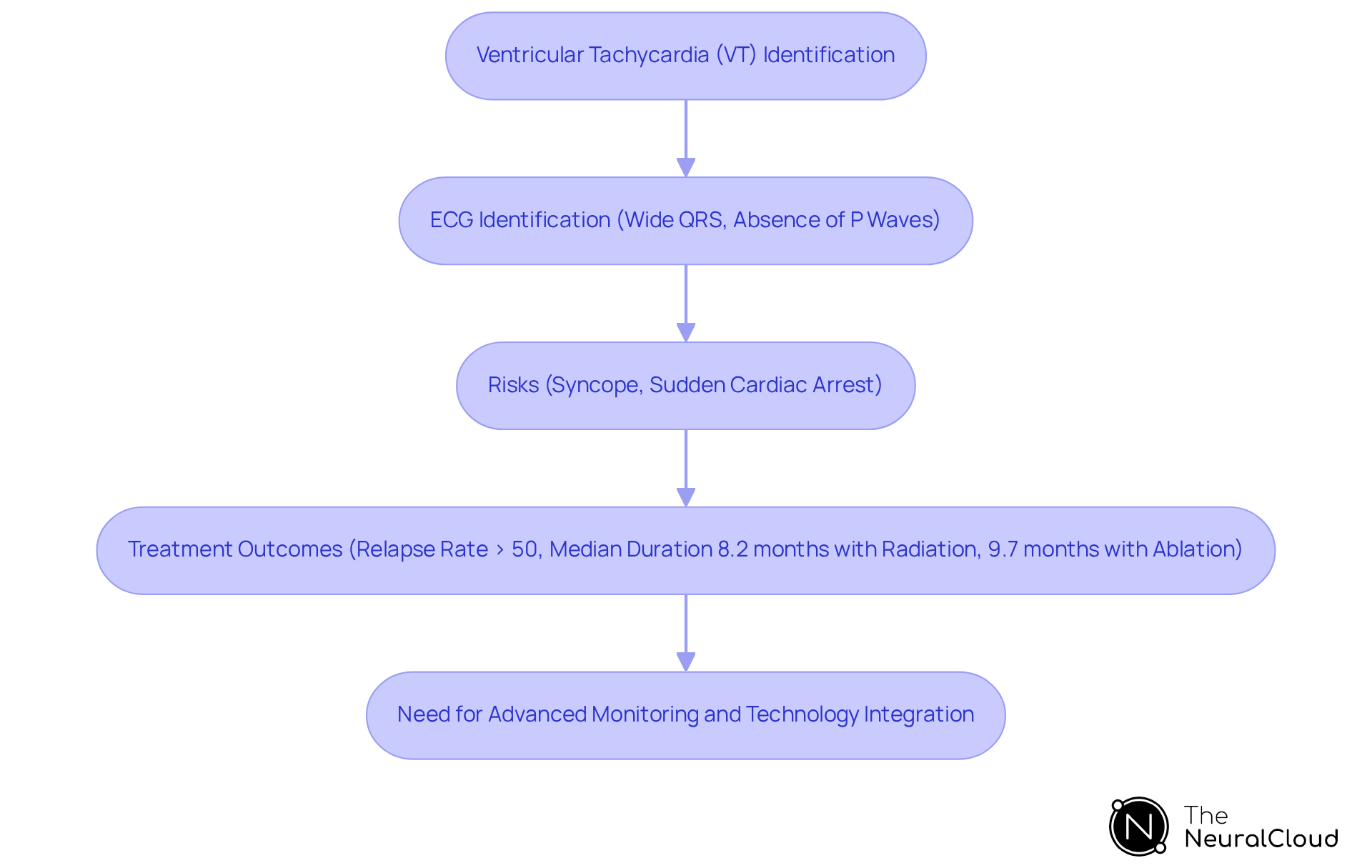
Ventricular tachycardia (VT) is defined by three or more consecutive ventricular beats at a rate exceeding 100 beats per minute. It can be identified on an ECG by wide QRS complexes and the absence of preceding P waves. This arrhythmia poses significant risks, including syncope and sudden cardiac arrest. Alarmingly, over 50% of individuals experience a relapse within a year after standard treatments like catheter ablation. The median duration before new persistent VT episodes occur is approximately 8.2 months with radiation therapy, compared to 9.7 months with ablation. This highlights the urgent need for effective monitoring and intervention strategies.
For health tech developers, integrating advanced features that facilitate the rapid detection of VT is crucial for enhancing patient safety and improving clinical response times. Recent studies have shown that machine learning algorithms can effectively identify arrhythmia-causing cells, illustrating how technology can revolutionize VT management. As the landscape of heart care evolves, the implementation of innovative solutions will be vital in addressing the complexities associated with ventricular tachycardia. This ultimately leads to better outcomes for patients.
Premature Ventricular Contractions: Understanding Their Impact
Premature ventricular contractions (PVCs) present significant challenges in ECG analysis, as they are early heartbeats originating from the ventricles. These contractions often create a sensation of a skipped beat, which can be alarming for patients. On an ECG, PVCs are identified by wide and bizarre QRS complexes that occur without preceding P waves. While many PVCs are benign, frequent occurrences can lead to more serious arrhythmias, making vigilant monitoring essential.
Research highlights the risks associated with PVCs, particularly for patients with a moderate-to-high PVC burden (≥1000/day). These individuals face a significantly increased risk of developing new-onset atrial fibrillation (AF), with rates of 4.91% compared to 2.73% in those with a low burden. Furthermore, individuals exhibiting high-grade PVCs during recovery have a 70% to 80% increased risk of future cardiovascular death. This underscores the importance of distinguishing between benign PVCs and those that may signal underlying heart issues.
To address these challenges, health tech developers should focus on creating sophisticated algorithms capable of accurately differentiating between various PVC conditions. For instance, advancements in PVC detection algorithms can significantly enhance clinical decision-making. Studies have shown the effectiveness of Holter monitoring in identifying AF, demonstrating the need for improved detection methods.
The integration of an automated ECG analysis platform, such as that offered by Neural Cloud Solutions, can revolutionize the detection and analysis of PVCs. This system maps ECG signals through noise and provides beat-by-beat analysis, assisting clinicians in recognizing heart events with enhanced precision and effectiveness. As the medical community continues to investigate the effects of PVCs on heart health, the development of reliable detection tools will be crucial in improving outcomes for patients.

Atrial Flutter: Distinguishing Features and Treatment Options
Atrial flutter is marked by a rapid and regular atrial rate, usually around 300 beats per minute. This condition is identifiable by a distinctive 'sawtooth' pattern of flutter waves on the ECG, particularly visible in leads II, III, and aVF. Effective treatment options include:
- Rate control
- Rhythm control
- Catheter ablation
Recent advancements in management highlight the importance of timely intervention, with cardioversion emerging as a viable option.
For health tech developers, it's crucial to integrate features that accurately identify atrial flutter and distinguish it from atrial fibrillation. This differentiation is essential for enhancing diagnostic accuracy. Advanced platforms like Neural Cloud Solutions play a pivotal role in this process. They transform noisy recordings into detailed insights through sophisticated noise filtering and adaptive algorithms, significantly improving the identification of atrial flutter amidst challenging recordings.
Statistics show that the incidence rate of atrial flutter is reported as 88 per 100,000 person-years in the US. This underscores the critical need for precise ECG identification of basic EKG rhythms, as misdiagnosis can lead to inappropriate treatment strategies. Real-world examples illustrate how advanced ECG analysis, particularly through automated labeling and enhanced diagnostic yield provided by MaxYield™, can improve outcomes. By ensuring precise identification and management of atrial flutter, healthcare professionals can effectively reduce the burden of this common arrhythmia.

First Degree AV Block: Recognition and Clinical Significance
First-degree atrioventricular block (AVB) is characterized by a PR interval exceeding 200 milliseconds on the ECG, with each P wave followed by a QRS complex. While it is often asymptomatic and generally considered benign, it can indicate underlying conduction system issues. For health tech developers, grasping the clinical implications of first-degree AVB is essential for creating tools that effectively alert clinicians to potential conduction abnormalities that may require further assessment.
Statistics show that the prevalence of first-degree AVB is around 4%, with its incidence rising with age, particularly in males aged 80 years and older. Notably, a PR interval exceeding 350 milliseconds is associated with a significantly higher risk of needing permanent pacing. Research indicates that 7 out of 10 individuals with such intervals underwent pacemaker implantation, highlighting the importance of monitoring these intervals.
Experts stress the need for vigilance regarding prolonged PR intervals, as they correlate with increased risks of atrial fibrillation, heart failure, and all-cause mortality. For instance, one study found that first-degree AVB was independently linked to a 5-year cumulative incidence of atrial fibrillation of 6.8% in individuals with prolonged PR intervals, compared to just 2.1% in those without.
Incorporating these insights into health tech solutions can significantly enhance clinicians' ability to detect and manage potential heart issues early, ultimately leading to improved patient outcomes. By understanding the implications of first-degree AVB, developers can create more effective tools that support timely interventions.

Ventricular Fibrillation: Urgent Recognition and Response
Ventricular fibrillation (VF) presents significant challenges in cardiac care, characterized by chaotic electrical activity in the ventricles. This leads to ineffective contractions and a marked loss of cardiac output. On an ECG, basic EKG rhythms like VF manifest as a rapid, erratic waveform, lacking identifiable QRS complexes. The urgency for immediate recognition and defibrillation is critical, as survival rates depend heavily on swift intervention. Studies show that timely defibrillation can result in survival rates as high as 50% when administered promptly after VF onset.
For health tech developers, prioritizing features that enable rapid detection of VF is essential. The MaxYield™ platform exemplifies this approach, integrating advanced algorithms that identify VF in real-time. This capability allows healthcare professionals to act swiftly in critical situations. With automated ECG analysis, MaxYield™ effectively maps basic EKG rhythms through noise, isolating key features in every heartbeat. It delivers beat-by-beat analysis of 200,000 heartbeats in under 5 minutes, enhancing the clarity and efficiency of ECG interpretation, which is crucial for recognizing basic EKG rhythms, including VF.
The occurrence of VF during cardiac arrest incidents is substantial, with approximately 70% of individuals experiencing this deadly rhythm. Real-world examples underscore the importance of a swift response. Recent case studies reveal that three-quarters of individuals treated with double sequential defibrillation left the hospital with positive neurological outcomes, highlighting the impact of prompt intervention.
As we approach 2025, the emphasis on rapid recognition of VF will intensify, driven by technological advancements and a deeper understanding of cardiac emergencies. The integration of AI-powered monitoring systems, such as MaxYield™, can significantly enhance early detection and automate noise reduction, ultimately improving outcomes in critical situations.

Sinus Bradycardia: Clinical Considerations and Management
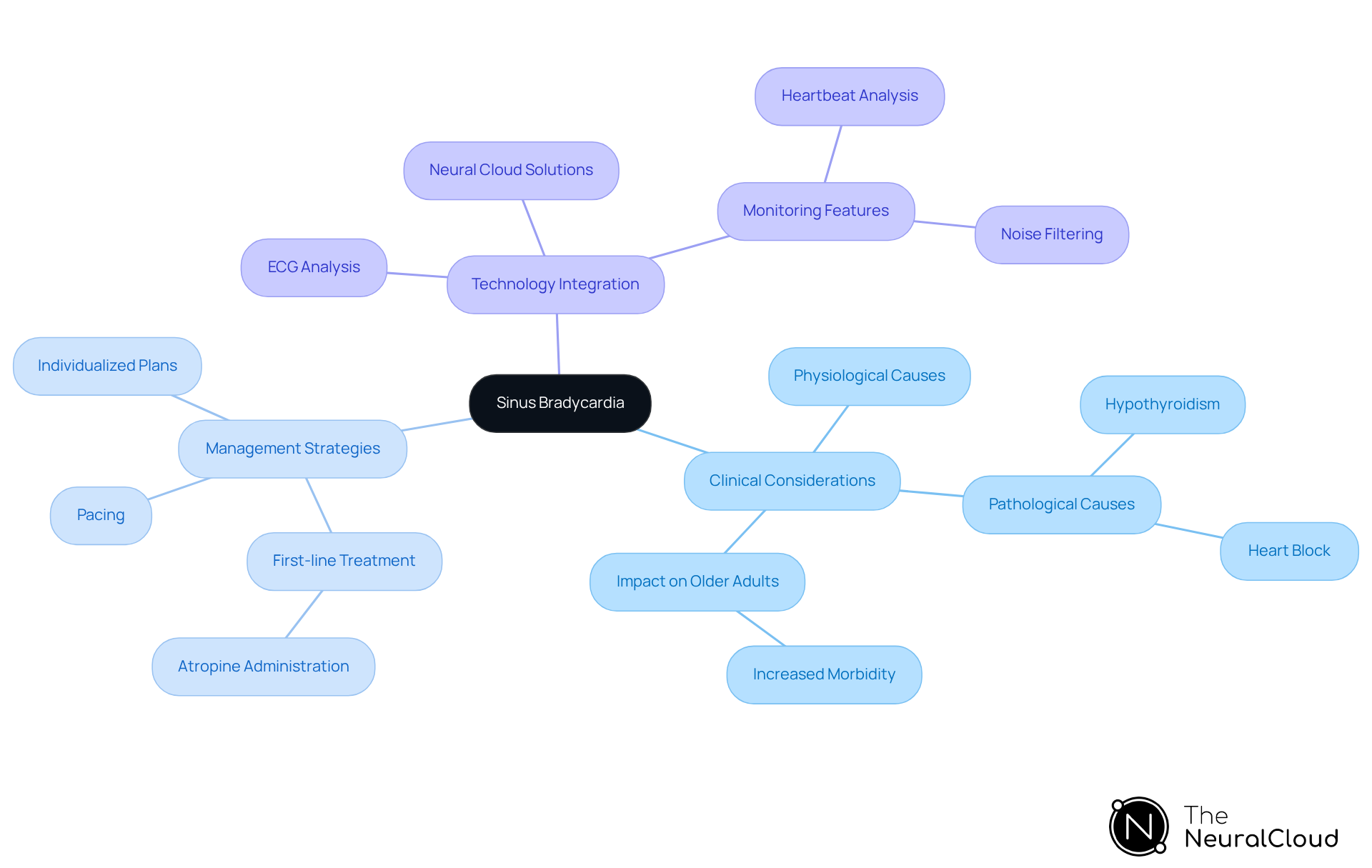
Sinus bradycardia is defined by a heart rate of fewer than 60 beats per minute, originating from the sinoatrial (SA) node. This condition can be physiological, often observed in athletes, or pathological, indicating potential underlying issues such as hypothyroidism or heart block. Recent studies emphasize that bradycardia can significantly affect clinical outcomes, particularly in older adults, where it may correlate with increased morbidity. The American College of Cardiology highlights the necessity of prompt treatment for individuals with symptomatic bradycardia, especially those experiencing dizziness or fainting.
Management strategies for sinus bradycardia typically focus on addressing the underlying cause. In symptomatic cases, atropine is often the first-line treatment, administered intravenously to increase heart rate. Additionally, pacing may be necessary for individuals with severe bradycardia or those who do not respond to medication. The Heart Rhythm Society's latest guidelines stress the importance of individualized treatment plans, considering factors such as symptom severity and patient preferences.
For health tech developers, understanding the nuances of sinus bradycardia is crucial for ensuring accurate heart rate monitoring and facilitating appropriate clinical responses. The integration of advanced technologies like Neural Cloud Solutions' platform can significantly enhance this process. This system automates ECG analysis, offering detailed insights and noise filtering features that enable the swift detection of critical cardiac events.
Key Features of Neural Cloud Solutions' Platform:
- Automates ECG analysis for efficiency.
- Provides detailed insights into cardiac events.
- Offers noise filtering for clearer data interpretation.
With the ability to analyze 200,000 heartbeats in less than 5 minutes and identify P-wave, QRS complex, and T-wave onsets, leveraging such advanced monitoring technologies becomes essential as the prevalence of bradycardia increases, particularly among the aging population. This ensures timely interventions and enhances patient outcomes, aligning with ongoing efforts to optimize cardiovascular care.
T-Wave Changes: Interpreting Their Clinical Relevance
T-wave changes on an ECG can indicate various conditions, including ischemia, electrolyte imbalances, and structural heart disease. Abnormal T waves may present as inversions, peaks, or flattening, each suggesting different underlying issues. Recent studies highlight that T wave inversion (TWI) is a common finding, documented in 2% of a cohort of 5,360 young, apparently healthy individuals, with 13% of those diagnosed with cardiomyopathy. This underscores the importance of accurately interpreting T-wave changes, as deeper T waves (>0.183 mV) significantly increase the likelihood of cardiomyopathy diagnosis by 18 times.
For health tech developers, integrating algorithms capable of detecting and interpreting T-wave changes is crucial for enhancing diagnostic accuracy and supporting clinical decision-making. The MaxYield™ platform exemplifies this integration, offering automated ECG analysis that maps ECG signals through noise, isolating and labeling key features in every heartbeat. With its capability to provide beat-by-beat analysis and handle 200,000 heartbeats in under 5 minutes, this system ensures that T-wave abnormalities are precisely identified and examined, even in recordings with elevated levels of noise and artifacts.
The prognostic value of T-wave abnormalities has been emphasized in recent research, which indicates that these changes are stronger predictors of cardiovascular mortality than ST segment depression. For instance, a study involving 46,950 ECGs found that T-wave abnormalities significantly correlated with increased cardiovascular death rates, reinforcing the need for focused clinical attention on these markers.
Dr. Gherardo Finocchiaro observed that the capability to distinguish between benign and harmful T wave abnormalities is crucial for effective management of individuals, especially since T-wave abnormalities impacting multiple regions of the heart were discovered to be seven times more likely to signify underlying disease. This highlights the clinical relevance of developing advanced algorithms, such as those found in MaxYield™, that can assist healthcare professionals in making informed decisions based on precise ECG interpretations. Real-world applications of this technology can lead to improved patient outcomes, particularly in identifying those at risk for serious cardiac events.

Conclusion
Mastering basic EKG rhythms is essential for health tech developers, as these rhythms form the foundation for diagnosing various cardiac conditions. However, ECG analysis can be challenging due to the complexity of heart rhythms and the need for timely intervention. This is where advanced tools like Neural Cloud Solutions' MaxYield™ platform come into play.
The MaxYield™ platform streamlines ECG analysis by integrating cutting-edge technology that enhances the accuracy and speed of identifying critical heart rhythms. Key features include:
- Automated rhythm detection
- Real-time monitoring
- Comprehensive reporting capabilities
These features not only simplify the analysis process but also empower healthcare professionals to make informed decisions quickly.
The advantages of using the MaxYield™ platform are significant. By improving the efficiency of ECG analysis, healthcare providers can ensure timely detection and intervention, particularly in life-threatening situations like ventricular fibrillation. This ultimately leads to better patient outcomes and improved cardiac health management.
As the healthcare landscape evolves, understanding and accurately interpreting EKG rhythms remains crucial. Health tech developers are encouraged to prioritize the integration of advanced ECG analysis tools like MaxYield™. By doing so, they can enhance monitoring capabilities and facilitate prompt clinical decision-making, contributing to improved patient care and potentially saving lives through timely interventions.
Frequently Asked Questions
What is the MaxYield™ platform and what challenges does it address in ECG analysis?
The MaxYield™ platform by Neural Cloud Solutions automates the detection and labeling of essential heart features, significantly improving efficiency and accuracy in ECG analysis.
How quickly can MaxYield™ process ECG data?
MaxYield™ can process over 200,000 heartbeats in under five minutes, providing timely and reliable insights for healthcare professionals.
What are the key features of the MaxYield™ platform?
Key features include advanced noise filtering capabilities that enhance ECG signal clarity, compatibility with various ECG devices, and the ability to transform noisy recordings into detailed insights.
How does MaxYield™ improve patient outcomes in clinical settings?
Case studies show that the AI-ECG group using MaxYield™ reduced the time from ECG acquisition to cath lab arrival to an average of 43.3 minutes, compared to 52.3 minutes for standard care, leading to improved patient outcomes.
What is sinus rhythm and why is it important in EKG interpretation?
Sinus rhythm is characterized by a regular heart rate of 60 to 100 beats per minute, initiated by the sinoatrial (SA) node. It serves as the baseline for diagnosing arrhythmias and other heart conditions, making it crucial for health tech developers.
What is the significance of maintaining normal sinus rhythm (NSR)?
Maintaining NSR is linked to improved cardiac health outcomes, with research indicating that individuals spend an average of 38.2% of their days entirely in NSR, correlating with better health outcomes.
What are the challenges associated with atrial fibrillation (AF) in ECG analysis?
AF presents challenges due to its irregular and often rapid heart rate, leading to ineffective atrial contractions and the absence of distinct P waves on an ECG.
What management strategies are effective for atrial fibrillation?
Effective management strategies for AF include rate control, rhythm control, and anticoagulation to reduce the risk of thromboembolic events.
How does the MaxYield™ platform enhance the detection and management of atrial fibrillation?
MaxYield™ features advanced noise reduction and artifact handling, enabling accurate detection of AF and salvaging obscured sections of ECG recordings, thereby enhancing diagnostic yield.
What modern technologies are being used for atrial fibrillation treatment?
Technologies like pulsed field ablation (PFA) are being used, which employ ultra-fast electrical pulses to target and destroy abnormal heart cells while minimizing damage to surrounding tissue.






