Introduction
Understanding EKG arrhythmias is crucial for healthcare professionals, particularly as technology reshapes cardiac care. The emergence of advanced platforms like Neural Cloud Solutions' MaxYield™ is transforming the landscape of ECG analysis. This platform offers remarkable accuracy and efficiency in detecting various arrhythmias, addressing the ongoing challenges in ECG interpretation.
However, a key question arises: how can developers and clinicians effectively leverage these innovations to improve patient outcomes while navigating the complexities of each arrhythmia's unique characteristics? This article explores ten essential EKG arrhythmias that every health tech developer should know, examining their clinical implications and the significant role of AI in diagnosis and management.
By understanding the features of MaxYield™, healthcare professionals can enhance their ECG analysis capabilities. The platform's advanced algorithms streamline the detection process, allowing for quicker and more accurate diagnoses. This not only improves clinical efficiency but also enhances patient care by enabling timely interventions.
In summary, as technology continues to evolve, embracing tools like MaxYield™ can empower healthcare professionals to navigate the complexities of EKG arrhythmias effectively.
Neural Cloud Solutions MaxYield™: Advanced ECG Analysis for Arrhythmia Detection
ECG analysis faces significant challenges, particularly in the accurate detection of EKG arrhythmia. Traditional methods often rely on manual interpretation, which can be time-consuming and prone to errors. To address these issues, 'Neural Cloud Solutions' has developed the MaxYield™ platform, which leverages sophisticated AI algorithms to automate EKG arrhythmia detection. This innovative technology can process over 200,000 heartbeats in under five minutes, providing healthcare professionals with swift and precise insights into cardiac health.
The MaxYield™ platform boasts advanced features that enhance ECG analysis. By effectively filtering out noise and isolating critical ECG features, it significantly improves diagnostic yield. This allows clinicians to focus on high-stakes decision-making rather than being overwhelmed by manual analysis. The platform's performance metrics highlight its capabilities, demonstrating high sensitivity and specificity across various diagnostic patterns. For example, the deep neural networks (DNNs) utilized in the system achieved impressive F1 scores of 0.957 for rhythm detection and 0.925 for acute coronary syndrome (ACS).
These results validate the effectiveness of the MaxYield™ platform in accurately interpreting ECGs, as evidenced by case studies that showcase its superiority over traditional computerized interpretation methods. Furthermore, the continuous learning model integrated into MaxYield™ enhances diagnostic accuracy over time, adapting to new data and improving performance. Cardiologists have noted the transformative impact of AI on ECG signal clarity, emphasizing that automated detection not only streamlines workflows but also enhances the reliability of diagnoses.
The integration of AI into ECG analysis represents a significant advancement, enabling clinicians to provide timely and informed care to patients with EKG arrhythmia. The ongoing pilot program with a Canadian cardiology clinic aims to validate these advancements in a real-world setting, showcasing the practical applications of this cutting-edge technology. With MaxYield™, healthcare professionals can expect improved efficiency and accuracy in their diagnostic processes.

Atrial Fibrillation: Key Characteristics and Clinical Implications
Atrial fibrillation (AF) presents significant challenges in EKG arrhythmia analysis due to its irregular and often rapid heart rate, which can impair blood flow. AF is identified on an ECG as an 'irregularly irregular' rhythm, which is a type of EKG arrhythmia that typically lacks discernible P waves. The clinical implications are serious, with AF linked to a fivefold increase in stroke risk, affecting over 40 million individuals worldwide. This increased risk arises from ineffective blood pumping, leading to pooling in the atria and a higher likelihood of clot formation, which can result in strokes, heart attacks, and heart failure.
To address these challenges, effective management strategies for AF include anticoagulation therapy to prevent thromboembolic events and rhythm control techniques aimed at restoring normal heart rhythm. Recent studies indicate that catheter ablation can reduce mortality by 70% and significantly decrease major cardiovascular events. Additionally, innovative AI models, powered by Neural Cloud Solutions' technology, are being developed to provide personalized treatment recommendations. These models allow clinicians to weigh the risks of stroke against potential bleeding complications, enhancing ECG analysis through advanced noise filtering and distinct wave recognition, which is crucial for accurately identifying EKG arrhythmia amidst physiological variability and signal artifacts.
The MaxYield™ platform exemplifies advanced technology in AF oversight, enhancing clinical decision-making and improving patient outcomes. Key features of MaxYield™ include:
- Advanced noise filtering for clearer ECG readings.
- Distinct wave recognition to accurately identify AF.
- Personalized treatment recommendations based on AI analysis.
These features translate into significant advantages for healthcare professionals. For instance, AI-driven recommendations could reclassify nearly half of AF patients, reducing unnecessary anticoagulation treatment while maintaining safety. As our understanding of AF evolves, so do the strategies for its management, highlighting the importance of timely intervention and customized approaches in clinical practice.

Ventricular Tachycardia: Identification and Management Strategies
Ventricular tachycardia (VT) is marked by a series of rapid heartbeats that originate from the ventricles, typically appearing as wide QRS complexes on an ECG. Effective management strategies for VT include:
- Antiarrhythmic medications
- Synchronized cardioversion
- Catheter ablation
Early recognition and intervention are crucial, as untreated VT can lead to ventricular fibrillation and sudden cardiac arrest.
Statistics reveal a concerning trend: the age-adjusted mortality rate (AAMR) from VT has increased significantly, rising from 0.22 in 1999 to 0.32 in 2020. This underscores the growing public health issue associated with this condition. Notably, disparities in mortality rates exist, with Black adults facing a higher AAMR of 0.44 compared to 0.26 for White adults.
Case studies emphasize the need for tailored management approaches. For example, individuals with ischemic VT often benefit from dietary changes alongside pharmacological treatments. Those experiencing recurrent episodes may require referral to electrophysiologists for specialized care. In one study, an AI tool demonstrated an impressive sensitivity of 81.4% in detecting cells that cause EKG arrhythmia. This indicates that advanced technologies, such as Neural Cloud Solutions' platform, could enhance the accuracy of ablation procedures and improve patient outcomes. The system effectively transforms lengthy and noisy ECG recordings into clean signals, allowing for the rapid isolation of EKG arrhythmia waves even amidst high noise and artifact levels.
Recent advancements in management strategies highlight the role of implantable cardioverter-defibrillators (ICDs) for individuals with hemodynamically unstable VT. These devices significantly improve survival rates compared to antiarrhythmic medications alone. Furthermore, ongoing research into the genetic factors of familial VT is paving the way for more personalized treatment options.
In summary, a multifaceted approach to VT management-incorporating medication, lifestyle changes, and advanced technologies-is essential for improving outcomes and addressing the increasing burden of this serious cardiac condition.

Sinus Bradycardia: Interpretation and Clinical Relevance
Sinus bradycardia is defined by a heart rate of fewer than 60 beats per minute, typically appearing as a normal sinus rhythm on an ECG. While it is often seen as benign, it can indicate underlying health issues such as:
- Hypothyroidism
- Coronary artery disease
- Sick sinus syndrome
Clinicians need to assess the patient's symptoms, as bradycardia may be asymptomatic in many cases. However, when symptoms like dizziness, fatigue, or syncope arise, further investigation and potential intervention become necessary.
Recent studies show that sinus bradycardia is common among older adults and can be worsened by factors such as:
- Electrolyte imbalances
- Certain medications, including beta-blockers
The American College of Cardiology emphasizes the importance of accurate ECG interpretation in diagnosing bradycardia and any related EKG arrhythmia, as symptoms alone do not provide a definitive diagnosis. Advanced solutions like Neural Cloud Solutions' MaxYield™ enable healthcare professionals to utilize automated ECG analysis, improving the accuracy and efficiency of diagnosing bradycardia. An EKG arrhythmia is crucial for identifying the specific type of bradycardia, which may include:
- Sinus node dysfunction
- Atrioventricular (AV) block
Treatment options vary based on the severity of symptoms and underlying causes. For symptomatic individuals, pacing may be required to maintain adequate heart rates and prevent complications. Recent research highlights the role of leadless pacemakers as a minimally invasive option for those needing pacing, offering effective management of bradycardia while minimizing procedural risks.
Understanding the clinical significance of sinus bradycardia is essential for healthcare providers, as timely diagnosis and intervention can significantly impact patient outcomes. Regular monitoring and adherence to treatment protocols are vital for effectively managing this condition, especially in populations with high cardiovascular risk factors, such as individuals with diabetes or obesity. By integrating wearable technology with MaxYield™, healthcare professionals can enhance ECG analysis, reduce operational costs, and improve the quality of care.

Atrial Flutter: Recognition and Treatment Approaches
Atrial flutter is marked by a rapid, regular atrial rhythm, often recognizable on the ECG as a distinctive 'sawtooth' pattern, especially in the inferior leads. Effective management of atrial flutter typically requires a multifaceted approach. Rate control is usually achieved with beta-blockers, while anticoagulation plays a crucial role in reducing the risk of thromboembolic events. For those seeking definitive treatment, catheter ablation has proven to be a highly effective option. Studies indicate that the cumulative incidence of catheter ablation for atrial flutter is just 6.5% over ten years, highlighting its under-utilization despite significant benefits.
Recent advancements in treatment strategies have shown promise. For instance, the adoption of pulsed field ablation technology has been recognized for its safety and effectiveness in managing atrial flutter. Hospitals like Northwell Lenox Hill are incorporating this innovative approach to enhance outcomes for patients. The FieldForce Ablation System, utilized in clinical settings, has demonstrated an average ablation duration of 35 minutes, achieving a freedom rate from ventricular tachycardia of 78% in selected groups.
Moreover, the importance of early rhythm control is emphasized by findings that show a significant reduction in adverse cardiovascular events when implemented promptly. This aligns with the broader trend of improving long-term results for individuals with atrial flutter, as evidenced by survival rates of 91.2% at one year and 55.2% at ten years post-hospitalization.
In conclusion, understanding the recognition and management of atrial flutter is essential for health tech developers. This knowledge guides the creation of tools and technologies that can enhance cardiac care and improve outcomes for individuals.

Premature Ventricular Contractions: Causes and Clinical Significance
Premature ventricular contractions (PVCs) are extra heartbeats that disrupt the heart's normal rhythm, often felt as palpitations. While they are typically benign, frequent PVCs can indicate underlying heart conditions, which may require further evaluation. Clinicians should assess both the frequency of PVCs and any associated symptoms to determine the best management approach. Treatment options may include lifestyle modifications, such as reducing stress and avoiding stimulants, along with medications to control symptoms.
The clinical significance of PVCs is highlighted by their potential to signal more serious cardiac issues, including the risk of EKG arrhythmia. For instance, individuals with a PVC burden exceeding 24% face a significantly higher risk of developing PVC-induced cardiomyopathy, which can lead to heart failure. A case study of a 65-year-old man with complete atrioventricular block showed that implanting a dual-chamber pacemaker not only alleviated debilitating symptoms but also greatly improved his quality of life, underscoring the importance of timely intervention.
Recent insights into PVCs stress the necessity for continuous monitoring, particularly in individuals with a history of myocardial infarction. Frequent PVCs in these cases are linked to worse outcomes, including increased mortality, which may be attributed to EKG arrhythmia. Statistics indicate that the QRS complex duration in PVCs often exceeds 0.12 seconds, signaling a disruption in normal conduction pathways. While most individuals with occasional PVCs do not experience significant symptoms, those with underlying structural heart disease may encounter a more severe clinical course.
In summary, recognizing the clinical significance of PVCs is vital for effective management. By understanding the causes, symptoms, and potential complications associated with PVCs, healthcare professionals can make informed decisions that enhance patient outcomes.

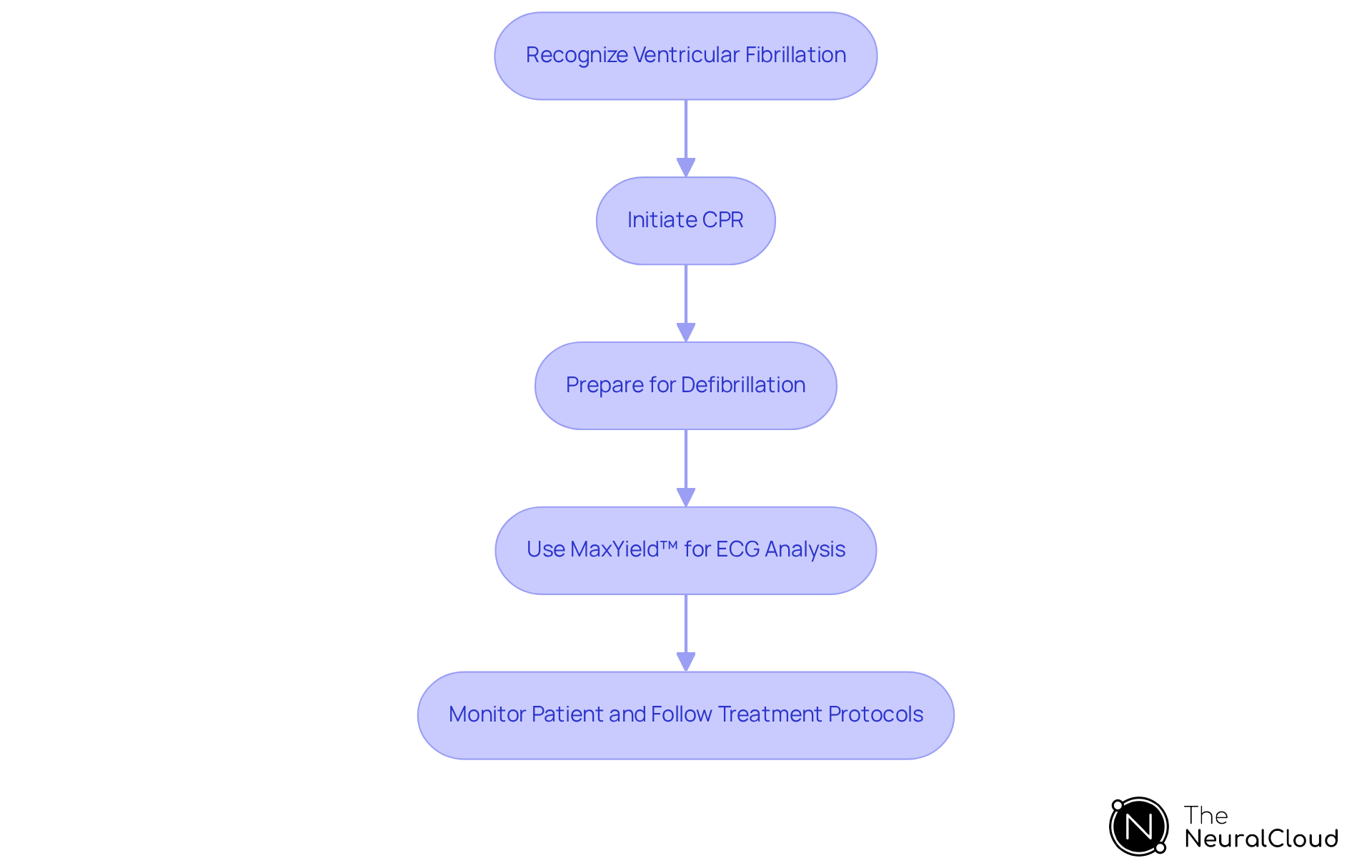
Ventricular Fibrillation: Urgent Recognition and Response
Ventricular fibrillation (VF) is a critical arrhythmia characterized by disorganized electrical activity in the heart's ventricles. This condition leads to ineffective contractions and poses a significant risk of sudden cardiac arrest. Immediate recognition of VF is essential, as timely intervention can prevent fatal outcomes. The first response to VF includes cardiopulmonary resuscitation (CPR) and defibrillation, both crucial for restoring a normal heart rhythm.
Recent advancements in ECG analysis, particularly through the MaxYield™ platform, underscore the importance of rapid intervention. This innovative system transforms lengthy and noisy ECG recordings into clean, crisp signals, utilizing cutting-edge AI technology for enhanced clarity and speed in ambulatory ECG waveform analysis. Such capabilities are vital in clinical trials, emphasizing the necessity for prompt medical intervention in life-threatening EKG arrhythmias, such as VF. The effectiveness of timely reactions in EKG arrhythmia treatment is clearly demonstrated.
Treatment protocols for VF highlight the urgency of addressing EKG arrhythmia with immediate action. An implantable cardioverter defibrillator (ICD) can automatically detect VF and deliver life-saving shocks to restore normal rhythm. Additionally, CPR should be initiated without delay to maintain blood flow to vital organs until defibrillation can be performed.
The latest treatment guidelines advocate for a structured approach to managing VF, incorporating advanced technologies like pulsed field ablation (PFA), recognized for its efficacy in treating EKG arrhythmia, including VF. Innovations such as MaxYield™ not only enhance the clarity of ECG signals but also streamline processes, reduce operational costs, and improve productivity in healthcare settings. Continuous education and training for healthcare professionals are essential to ensure they are prepared to respond effectively to VF cases.
In summary, the urgent handling of ventricular fibrillation requires swift recognition and a well-coordinated response. By integrating both traditional methods and emerging technologies like MaxYield™, healthcare professionals can significantly enhance patient outcomes.
Atrioventricular Blocks: Types and Clinical Management
Atrioventricular (AV) blocks are categorized into first, second, and third degrees, each presenting unique ECG characteristics and clinical implications, including the potential for EKG arrhythmia. First-degree AV block, characterized by a prolonged PR interval, is generally considered benign but can indicate a higher risk of developing atrial fibrillation. Recent studies indicate that around 85% of people over age 50 have atherosclerotic coronary disease, which can complicate the treatment of AV blocks.
Second-degree AV blocks can be further divided into Mobitz Type I (Wenckebach) and Mobitz Type II, both of which may require careful monitoring. Mobitz Type II is particularly concerning as it can progress to third-degree AV block and asystole, necessitating immediate intervention. Clinical oversight often involves rhythm monitoring and, in instances of symptomatic bradycardia, the initiation of temporary pacing or pharmacological support.
Third-degree AV block, or complete heart block, is a critical condition that typically requires pacemaker insertion. This intervention is essential to prevent life-threatening EKG arrhythmia and symptomatic bradycardia. A study highlighted that new onset AV blocks in COVID-19 patients occurred at a rate of 5.5 cases per 100 patients, underscoring the need for vigilant monitoring in this population.
The clinical implications of AV blocks extend beyond immediate handling; they also involve understanding the underlying risk factors. For instance, independent risk factors for first-degree AV block include:
- Male sex
- Older age
- Elevated systolic blood pressure
Lifestyle modifications, such as regular exercise, have shown a significant negative association with the prevalence of first-degree AV block, suggesting that proactive health management can mitigate risks.
With the integration of Neural Cloud Solutions' platform, healthcare professionals can enhance their analysis of these conditions. MaxYield™ employs advanced noise filtering and distinct wave recognition, allowing for the rapid isolation of ECG waves even in recordings affected by baseline wander, movement, and muscle artifacts. This ability enhances the precision of recognizing atrioventricular blocks and tackles typical issues in ECG analysis, such as physiological variability and signal artifacts, ultimately resulting in more efficient care.
In summary, effective clinical oversight of AV blocks and EKG arrhythmia requires a nuanced understanding of their types, associated risks, and the implementation of appropriate monitoring and intervention strategies. This knowledge is essential for healthcare professionals aiming to enhance outcomes in the context of arrhythmias.

Sinus Tachycardia: Causes and Clinical Implications
Sinus tachycardia is marked by an increased heart rate, often resulting from heightened sympathetic activity due to stress, fever, or exercise. While it is generally benign, persistent sinus tachycardia can signal underlying cardiac or systemic issues. Therefore, clinicians must assess the patient's history and symptoms to determine suitable management strategies.
Advanced tools like Neural Cloud Solutions' platform can significantly improve ECG analysis in these scenarios. This platform automates ECG analysis, providing beat-by-beat insights that include a thorough examination of P-wave, QRS complex, and T-wave onsets and offsets. Additionally, it effectively filters out noise to isolate critical waveforms, enhancing the clarity of the data.
By integrating this technology, health tech developers can boost workflow efficiency. The platform ensures that even subtle EKG arrhythmias, such as sinus tachycardia, are detected and analyzed with greater precision. This not only aids healthcare professionals in making informed decisions but also enhances patient care through timely and accurate diagnostics.

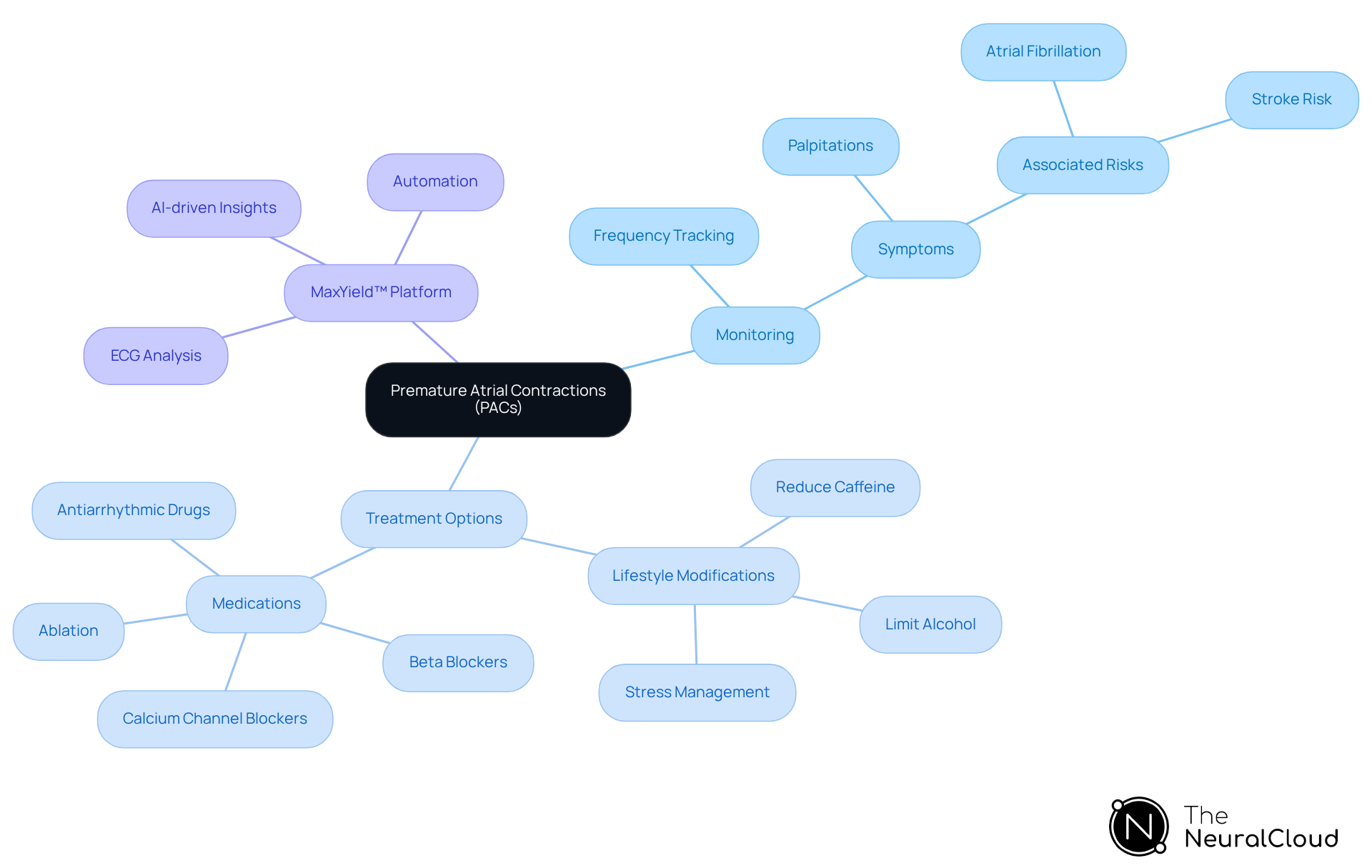
Premature Atrial Contractions: Monitoring and Clinical Considerations
Premature atrial contractions (PACs) are extra beats that originate in the atria, often experienced as palpitations. While they are typically benign, frequent PACs can elevate the risk of developing atrial fibrillation. Therefore, monitoring the frequency of PACs and any associated symptoms is essential for determining whether further evaluation or treatment for EKG arrhythmia is necessary. This treatment may involve lifestyle modifications or medications.
The MaxYield™ platform addresses the challenges in ECG analysis by offering advanced features that enhance efficiency. It automates the labeling and data extraction processes, which streamlines the monitoring of PACs. This integration not only simplifies the workflow but also reduces operational costs, allowing healthcare professionals to track PACs and their implications, including EKG arrhythmia, more accurately.
By leveraging AI-driven insights, MaxYield™ supports healthcare providers in delivering timely and effective care. The benefits of this platform include improved patient outcomes through better monitoring and analysis of PACs, which can help in detecting EKG arrhythmia. With its user-friendly interface and robust capabilities, MaxYield™ empowers healthcare professionals to make informed decisions, ultimately enhancing the quality of care.
Conclusion
The exploration of EKG arrhythmias underscores the critical role of advanced technologies in enhancing cardiac care. Understanding various types of arrhythmias, such as atrial fibrillation, ventricular tachycardia, and sinus bradycardia, allows healthcare professionals to utilize tools like Neural Cloud Solutions' MaxYield™ platform. This platform improves diagnostic accuracy and efficiency through AI-driven analysis, streamlining workflows and empowering clinicians to make informed decisions that enhance patient outcomes.
Key insights regarding the management and clinical implications of specific arrhythmias have been shared throughout the article. The MaxYield™ platform offers rapid detection capabilities and tailored treatment strategies for conditions like atrial flutter and premature ventricular contractions. These advancements in ECG analysis are reshaping cardiac health, emphasizing the significance of timely intervention and personalized care. Such insights highlight the potential for improved health outcomes through innovative technological solutions.
Given the ongoing challenges posed by EKG arrhythmias, health tech developers are called to action: prioritize the integration of advanced analytical tools in clinical practice. Embracing technologies that enhance ECG interpretation and facilitate effective management strategies can significantly reduce the risks associated with arrhythmias. The future of cardiac care lies in the synergy between technology and clinical expertise, paving the way for a healthier tomorrow.
Features of the MaxYield™ Platform:
- AI-driven analysis for improved diagnostic accuracy
- Streamlined workflows for healthcare professionals
- Rapid detection capabilities for timely intervention
Advantages for Healthcare Professionals:
- Enhanced decision-making through accurate data
- Personalized treatment strategies for patients
- Improved patient outcomes through innovative technology
In conclusion, the integration of advanced analytical tools like the MaxYield™ platform is essential for addressing the challenges of EKG arrhythmias. By leveraging these technologies, the healthcare community can enhance ECG analysis and ultimately improve cardiac care.
Frequently Asked Questions
What is the MaxYield™ platform developed by Neural Cloud Solutions?
The MaxYield™ platform is an advanced ECG analysis tool that utilizes AI algorithms to automate the detection of EKG arrhythmias, processing over 200,000 heartbeats in under five minutes for swift and precise cardiac health insights.
How does MaxYield™ improve ECG analysis?
MaxYield™ enhances ECG analysis by effectively filtering out noise and isolating critical ECG features, which improves diagnostic yield and allows clinicians to focus on high-stakes decision-making without being overwhelmed by manual analysis.
What performance metrics does MaxYield™ achieve?
The platform demonstrates high sensitivity and specificity, with F1 scores of 0.957 for rhythm detection and 0.925 for acute coronary syndrome (ACS), validating its effectiveness in interpreting ECGs.
How does MaxYield™ adapt and improve over time?
The platform incorporates a continuous learning model that enhances diagnostic accuracy by adapting to new data, thereby improving its performance over time.
What is atrial fibrillation (AF) and why is it significant?
Atrial fibrillation (AF) is an irregular and often rapid heart rhythm identified on an ECG as 'irregularly irregular,' which significantly increases the risk of stroke and affects over 40 million individuals worldwide.
What management strategies are effective for atrial fibrillation?
Effective management strategies for AF include anticoagulation therapy to prevent thromboembolic events and rhythm control techniques, such as catheter ablation, which can reduce mortality and major cardiovascular events.
How does MaxYield™ assist in managing atrial fibrillation?
MaxYield™ enhances AF oversight by providing advanced noise filtering, distinct wave recognition for accurate identification of AF, and personalized treatment recommendations based on AI analysis.
What is ventricular tachycardia (VT) and how is it characterized?
Ventricular tachycardia (VT) is characterized by a series of rapid heartbeats originating from the ventricles, typically appearing as wide QRS complexes on an ECG.
What are the management strategies for ventricular tachycardia?
Management strategies for VT include antiarrhythmic medications, synchronized cardioversion, and catheter ablation, with early recognition and intervention being crucial to prevent severe complications.
What role do implantable cardioverter-defibrillators (ICDs) play in VT management?
ICDs significantly improve survival rates in individuals with hemodynamically unstable VT compared to antiarrhythmic medications alone.
How does the AI technology in Neural Cloud Solutions enhance the management of EKG arrhythmias?
The AI technology improves the accuracy of detecting EKG arrhythmias, transforming noisy ECG recordings into clean signals, which facilitates rapid isolation of arrhythmia waves even in challenging conditions.


