Introduction
Understanding ECG patterns is essential for cardiologists, as accurately interpreting these signals can mean the difference between timely intervention and critical delays in patient care. The challenges in ECG analysis are significant, especially as cardiac conditions become more complex. However, advancements in technology, particularly through platforms like Neural Cloud Solutions' MaxYield™, provide healthcare professionals with sophisticated tools that streamline the recognition of essential ECG patterns.
MaxYield™ offers features that enhance ECG analysis, such as advanced algorithms that filter out noise and artifacts, allowing for clearer signal interpretation. This capability not only improves diagnostic accuracy but also empowers clinicians to make informed decisions swiftly. As a result, healthcare professionals can respond more effectively to patients' needs, ultimately leading to better outcomes.
In this article, we will explore ten essential ECG patterns that every cardiologist must recognize. By highlighting the innovative solutions provided by MaxYield™, we aim to illustrate how these tools can enhance diagnostic accuracy and improve patient care. With the right resources, clinicians can stay ahead in identifying vital indicators, ensuring that they are well-equipped to navigate the complexities of cardiac conditions.
Neural Cloud Solutions: MaxYield™ for Enhanced ECG Pattern Recognition
ECG analysis presents several challenges, including physiological variability and signal artifacts that can obscure critical data. Neural Cloud Solutions' MaxYield™ platform addresses these issues by automating the recognition of essential patterns through advanced noise filtering and AI-driven methodologies. This innovative approach embodies Gold Standard Methodologies that streamline workflow, making it easier for healthcare providers to effectively analyze ECG patterns.
MaxYield™ utilizes cutting-edge algorithms to process over 200,000 heartbeats in under five minutes. This capability allows for beat-by-beat analysis that isolates and labels key features such as P-waves, QRS complexes, and T-wave intervals. By accelerating the analysis process, the platform enhances the quality of ECG patterns, empowering healthcare professionals to identify cardiac events with greater confidence.
Moreover, MaxYield™ salvages previously obscured sections of lengthy Holter and patch monitor recordings, significantly improving diagnostic yield. Its continuous learning model ensures that accuracy and efficiency improve over time, adapting to the evolving needs of healthcare providers. The platform's seamless integration capabilities facilitate efficient workflow adjustments, making it an invaluable tool for cardiologists and healthcare technicians.
In summary, MaxYield™ not only enhances the analysis of ECG data but also supports clinical decision-making by providing reliable insights. With its advanced features and user-friendly design, it stands out as a critical asset in the pursuit of improved patient outcomes.

Anterior ST Segment Elevation MI: Key Characteristics and Recognition
Anterior ST segment elevation myocardial infarction (MI) presents a significant challenge in ECG analysis, characterized by ECG patterns of ST elevation in the precordial leads V1 to V4. A notable elevation of at least 1 mm in two contiguous leads indicates transmural ischemia, often accompanied by hyperacute T waves. Recognizing these ECG patterns is crucial, as they typically signal a critical blockage in the left anterior descending artery, which necessitates immediate medical intervention.
Recent studies underscore the importance of prompt diagnosis, revealing that only 17% of STEMI patients from non-PCI centers receive timely interventions. Current guidelines stress the need for healthcare professionals to be vigilant in identifying these ECG patterns, as early recognition can greatly enhance patient outcomes.
The MaxYield™ platform by Neural Cloud Solutions addresses these challenges by enhancing the accuracy of ECG analysis through advanced noise filtering and wave recognition. This technology reduces false-positive activations, thereby improving treatment efficiency. Cardiologists have observed that the MaxYield™ algorithm evolves with each use, continuously refining diagnostic accuracy and efficiency.
Notably, the Queen of Hearts™ model demonstrates a false-positive rate of just 7.9%, significantly lower than the 41.8% rate associated with standard triage methods. This highlights the potential of AI-ECG technology to improve diagnostic accuracy and treatment times, ultimately benefiting both healthcare professionals and patients.

Inferior ST Segment Elevation MI: Diagnostic Insights and ECG Features
Inferior ST segment rise myocardial infarction (MI) is characterized by ST elevation in leads II, III, and aVF. This often coincides with reciprocal ST segment depression in the lateral leads (I and aVL), indicating a potential right coronary artery occlusion. Recognizing these changes promptly is crucial for clinicians, as they can significantly influence patient outcomes.
A key diagnostic criterion is the presence of an ST increase of 1 mm or more in two adjacent inferior electrodes. This finding underscores the need for immediate intervention. Recent studies highlight the importance of these ECG patterns, revealing that terminal QRS distortion in inferior STEMI is linked to larger infarct sizes and a reduced left ventricular ejection fraction (LVEF).
Cardiologists stress that understanding these ECG patterns is essential for accurate diagnosis and timely treatment. Delays in recognizing these changes can adversely affect patient outcomes. As research in this area progresses, it continues to enhance our understanding of ST elevation in inferior electrodes, emphasizing the necessity for healthcare professionals to stay informed about the latest findings.

Posterior ST Segment Elevation MI: Identification and Clinical Relevance
Diagnosing posterior ST segment rise myocardial infarction (MI) poses significant challenges, mainly due to the lack of typical ST rise on standard 12-lead ECG patterns. To enhance detection, clinicians are encouraged to utilize additional electrodes, specifically V7, V8, and V9. These electrodes can reveal ST elevation of at least 0.5 mm, indicating substantial myocardial injury that necessitates immediate reperfusion therapy. A systematic approach that incorporates these elements has shown improved diagnostic accuracy, particularly in cases where traditional methods fall short.
Cardiologists emphasize the critical importance of recognizing these ECG patterns, as missed diagnoses can lead to severe complications, including cardiogenic shock and arrhythmias. Current best practices advocate for an adaptable interpretation of ECG patterns, ensuring healthcare professionals remain vigilant when evaluating patients with atypical presentations. The integration of synthesized leads has been validated in clinical settings, proving effective in identifying isolated posterior wall ST-elevation MI, which represents approximately 3.3% of acute myocardial infarctions.
By adopting these strategies and leveraging the MaxYield™ platform, clinicians can significantly enhance patient outcomes through timely and accurate diagnosis. The platform not only streamlines ECG analysis but also empowers healthcare professionals with the tools needed to make informed decisions, ultimately improving patient care.

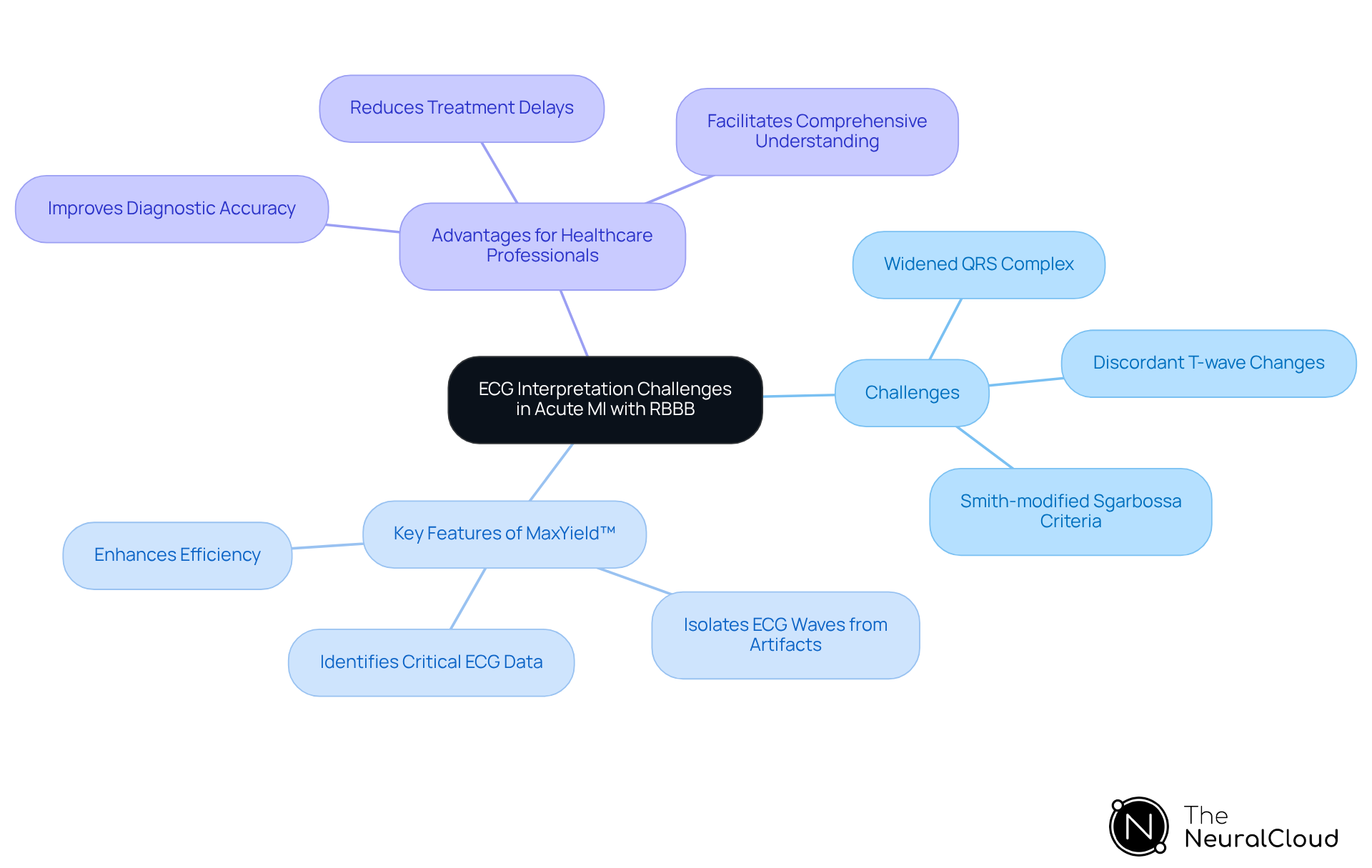
Acute MI with Right Bundle Branch Block: ECG Interpretation Challenges
Acute myocardial infarction (MI) accompanied by right bundle branch block (RBBB) presents notable challenges in the interpretation of ECG patterns. The widened QRS complex typical of RBBB can obscure the usual ST-segment changes associated with MI, complicating the diagnostic process of ECG patterns. Clinicians must recognize that while RBBB does not eliminate the possibility of STEMI, it complicates the interpretation of ST-segment elevation. Key features to monitor include discordant T-wave changes and the presence of Q waves, which may suggest certain ECG patterns indicative of an underlying acute coronary occlusion.
The Smith-modified Sgarbossa criteria highlight the importance of identifying concordant ST-segment elevation and depression in leads V1-V3, which can enhance diagnostic accuracy in patients with RBBB. Clinical examples show that many individuals with acute MI and RBBB may not meet traditional STEMI criteria, potentially leading to delays in treatment. In this context, Neural Cloud Solutions' MaxYield™ technology offers significant advantages by identifying and labeling critical ECG data, even in the presence of high noise and artifact levels.
MaxYield™ rapidly isolates ECG waves from recordings affected by baseline wander and muscle artifact, improving the efficiency of ECG analysis. This capability ensures that previously obscured sections of lengthy Holter and patch monitor recordings are salvaged. The advanced noise filtering and wave recognition features of MaxYield™ facilitate a more nuanced approach to ECG patterns interpretation, which is essential for the timely and effective management of these patients.
Key Features of MaxYield™:
- Identifies and labels critical ECG data amidst noise.
- Rapidly isolates ECG waves from artifacts.
- Enhances efficiency in ECG analysis.
Advantages for Healthcare Professionals:
- Improves diagnostic accuracy in challenging cases.
- Reduces delays in treatment for patients with acute MI and RBBB.
- Facilitates a more comprehensive understanding of ECG recordings.
New Left Bundle Branch Block: Distinguishing Features and Implications
New left bundle branch block (LBBB) is defined by a QRS duration of 120 ms or greater and often occurs alongside acute myocardial infarction (AMI). In cases of chest pain, it's essential for clinicians to treat new LBBB as an ST-segment elevation equivalent, which may require immediate reperfusion therapy. Key characteristics of these ECG patterns include:
- A broad, notched R wave in leads V5 and V6
- A deep S wave in leads V1 and V2
Recognizing these features is vital, as it can significantly impact management and outcomes for patients.
Current guidelines emphasize the importance of early identification and intervention for individuals presenting with new LBBB, especially in emergency settings. The MaxYield™ platform from Neural Cloud Solutions offers advanced noise filtering and wave recognition capabilities that enhance the accuracy of ECG analysis. This technology enables healthcare professionals to quickly isolate ECG waves from recordings affected by baseline wander, movement, and muscle artifacts, ultimately improving diagnostic yield.
The benefits of using MaxYield™ are clear: it allows for more accurate ECG interpretations, which can lead to timely and effective treatment decisions. Clinical examples show that prompt action can improve prognoses, highlighting the necessity for healthcare professionals to be vigilant in recognizing these critical ECG patterns. As noted by leading cardiologists, understanding the implications of new LBBB in the context of chest pain is essential for optimizing treatment strategies and enhancing patient care.

Anterior MI Pattern-Tombstoning: Visual Cues for Recognition
The tombstoning pattern in anterior myocardial infarction (MI) presents significant ST segment elevation that resembles a tombstone, typically seen in leads V1-V6. This distinctive pattern signals extensive myocardial damage and is often linked to critical occlusion of the left anterior descending artery. Recognizing this visual cue is crucial for clinicians, as early identification of tombstoning can lead to prompt intervention, ultimately improving patient outcomes. Current research highlights the importance of this pattern, associating it with higher mortality rates and adverse clinical events.
Understanding these visual signals is essential for accurate interpretation of ECG patterns and effective management of patients exhibiting ST segment elevation. The integration of wearable technology with Neural Cloud Solutions' MaxYield™ platform addresses the challenges faced in ECG analysis. The platform features automated labeling and advanced noise filtering capabilities, which tackle issues like physiological variability and signal artifacts. This ensures that critical data is accurately identified and analyzed, enhancing the overall efficiency of ECG interpretation.
The benefits of the MaxYield™ platform are significant for healthcare professionals. By streamlining the ECG interpretation process, it supports clinicians in making timely and informed decisions. The platform not only improves the accuracy of ECG analysis but also enhances the ability to respond to critical situations effectively. With these advancements, healthcare providers can better manage patient care and improve clinical outcomes.

Anterior MI Pattern-Typical ST Segment Elevation: Key Features
In anterior myocardial infarction (MI), the characteristic ST segment pattern typically shows a rise of at least 1 mm in two or more adjacent recordings, particularly in leads V2 to V4. This elevation is crucial for identifying transmural ischemia, which indicates acute coronary occlusion. Clinicians should also be vigilant for reciprocal ST segment depression in the inferior electrodes (II, III, aVF), as this can further confirm the diagnosis. Misinterpretation of these ST segment rise measurements can lead to incorrect diagnoses and delayed treatment, highlighting the importance of accurate analysis of ECG patterns.
The integration of Neural Cloud Solutions' MaxYield™ platform addresses these challenges by leveraging advancements in AI technology for ECG interpretation. MaxYield™ enhances diagnostic accuracy and reduces false activations, even in recordings affected by high levels of noise and artifact. It rapidly isolates ECG waves from challenging conditions, providing valuable support in emergency settings. Recognizing these ECG patterns promptly is vital for initiating urgent treatment, which can significantly improve patient outcomes.
As noted by experts, understanding these ECG patterns is essential for effective clinical decision-making in emergency situations. The MaxYield™ platform not only streamlines the analysis process but also empowers healthcare professionals with the tools needed to make informed decisions quickly. By improving the accuracy of ECG interpretations, MaxYield™ ultimately contributes to better patient care and outcomes.

Anterior MI Example-Isolated J Point Elevation: Clinical Significance
Isolated J point rise can occur in anterior myocardial infarction (MI) and may be mistaken for benign early repolarization (BER). Clinicians should recognize that this finding, defined by a J point rise of ≥1 mm in the precordial electrodes, can signify underlying ischemia. Recent studies suggest that J point rise is present in approximately 12.3% of subjects, underscoring its clinical relevance. It's crucial to differentiate this from benign conditions, as misinterpretation can lead to missed diagnoses and inadequate management, particularly in acute coronary syndromes.
For instance, when isolated J point increase is observed without notable ST segment changes, additional examination is necessary to exclude ischemic events. As K. Thygesen observes, 'Unfortunately, roughly half of high-risk individuals with occlusion myocardial infarction do not satisfy STEMI criteria, leading to delays in cath laboratory activation.' Identifying isolated J point elevation can enhance diagnostic accuracy in acute settings, ultimately improving outcomes for individuals.
The MaxYield™ platform from Neural Cloud Solutions addresses these challenges by automating ECG labeling and employing advanced noise filtering techniques to enhance the analysis of ECG patterns. This integration allows for more efficient analysis, helping clinicians isolate critical data even in recordings with high levels of noise and artifact. The features of MaxYield™ include:
- Automated ECG labeling for quicker assessments.
- Advanced noise filtering to enhance signal clarity.
- Efficient data isolation to support accurate diagnoses.
These advantages lead to improved diagnostic yield, enabling healthcare professionals to analyze ECG patterns and make timely and informed decisions in critical situations.

Integrating Technology in ECG Analysis: The Role of Advanced Solutions
ECG analysis faces several challenges, including the complexity of interpreting signals and the potential for human error. The MaxYield™ platform from Neural Cloud Solutions addresses these issues by integrating advanced technology into cardiac diagnostics. This innovative platform leverages sophisticated AI algorithms to enhance the clarity and accuracy of ECG patterns, enabling healthcare professionals to identify critical cardiac signals with precision.
MaxYield™ offers several key features that set it apart in the field of ECG analysis. It transforms lengthy and noisy ECG recordings into clean, crisp signals, rapidly isolating ECG waves even amidst baseline wander, movement, and muscle artifact. This capability not only streamlines workflows for healthcare providers but also significantly reduces the risk of misinterpretation. As Raghavee Neupane highlights, "AI technologies have the capacity to enhance diagnostic accuracy, enable earlier detection of subtle abnormalities, and alleviate the workload of healthcare providers."
The advantages of using MaxYield™ are substantial. A review of 800 studies indicates that AI-assisted interpretation of ECG patterns can enhance diagnostic accuracy and facilitate earlier detection of cardiac conditions. This underscores the importance of these advancements in modern healthcare. Furthermore, testimonials from leading cardiologists emphasize how AI is transforming ECG analysis, showcasing its potential to enhance clinical workflows and patient management strategies.
The adaptive algorithm of MaxYield™ continuously evolves, improving its diagnostic yield over time. This ongoing enhancement is crucial for effective clinical integration, ensuring that healthcare professionals can rely on the platform for accurate and timely cardiac diagnostics. By adopting MaxYield™, healthcare providers can not only improve patient outcomes but also optimize their operational efficiency.

Conclusion
Recognizing essential ECG patterns is crucial for cardiologists, particularly when diagnosing and managing acute myocardial infarctions. However, ECG analysis often presents challenges, such as noise and signal artifacts, which can hinder accurate interpretation. This is where Neural Cloud Solutions' MaxYield™ platform comes into play, offering advanced technology that enhances diagnostic capabilities.
MaxYield™ features a streamlined ECG analysis process that significantly improves the accuracy and efficiency of identifying critical cardiac events. By integrating AI-driven methodologies, the platform effectively addresses common issues in ECG interpretation. For instance, it rapidly processes and analyzes ECG data, reducing false positives and facilitating timely medical interventions. This capability is a game-changer for healthcare professionals, allowing them to respond more effectively to cardiac events.
The advantages of using MaxYield™ extend beyond just improved analysis. By enhancing ECG pattern recognition, this innovative tool supports clinical decision-making, ultimately leading to better patient outcomes. As the landscape of cardiac diagnostics evolves, embracing technologies like MaxYield™ becomes essential for healthcare providers. Staying informed about these advancements ensures that cardiologists are equipped to handle the complexities of cardiac events with confidence.
In summary, the integration of MaxYield™ into clinical practice not only streamlines ECG analysis but also empowers healthcare professionals to deliver superior patient care. By understanding and utilizing this platform, cardiologists can enhance their diagnostic accuracy and improve overall patient outcomes.
Frequently Asked Questions
What challenges does ECG analysis face?
ECG analysis faces challenges such as physiological variability and signal artifacts that can obscure critical data.
How does the MaxYield™ platform improve ECG analysis?
MaxYield™ automates the recognition of essential ECG patterns through advanced noise filtering and AI-driven methodologies, streamlining the workflow for healthcare providers.
What is the processing capability of MaxYield™?
MaxYield™ can process over 200,000 heartbeats in under five minutes, allowing for beat-by-beat analysis that isolates and labels key features such as P-waves, QRS complexes, and T-wave intervals.
How does MaxYield™ enhance diagnostic yield?
MaxYield™ salvages previously obscured sections of lengthy Holter and patch monitor recordings, significantly improving the diagnostic yield.
What is the continuous learning model of MaxYield™?
The continuous learning model of MaxYield™ ensures that its accuracy and efficiency improve over time, adapting to the evolving needs of healthcare providers.
What is the significance of recognizing Anterior ST Segment Elevation MI?
Recognizing Anterior ST segment elevation myocardial infarction (MI) is crucial as it indicates a critical blockage in the left anterior descending artery that requires immediate medical intervention.
What are the key ECG characteristics of Anterior ST Segment Elevation MI?
Key characteristics include ST elevation of at least 1 mm in two contiguous leads V1 to V4, often accompanied by hyperacute T waves.
How does MaxYield™ assist in recognizing Anterior ST Segment Elevation MI?
MaxYield™ enhances the accuracy of ECG analysis through advanced noise filtering and wave recognition, reducing false-positive activations and improving treatment efficiency.
What is the false-positive rate of the MaxYield™ algorithm compared to standard methods?
The MaxYield™ algorithm has a false-positive rate of just 7.9%, significantly lower than the 41.8% rate associated with standard triage methods.
What are the key characteristics of Inferior ST Segment Elevation MI?
Inferior ST segment elevation myocardial infarction (MI) is characterized by ST elevation in leads II, III, and aVF, often with reciprocal ST segment depression in lateral leads (I and aVL).
Why is prompt recognition of Inferior ST Segment Elevation MI important?
Prompt recognition is crucial as it can significantly influence patient outcomes, and delays can adversely affect treatment effectiveness.
What are the diagnostic criteria for Inferior ST Segment Elevation MI?
A key diagnostic criterion is an ST increase of 1 mm or more in two adjacent inferior electrodes, indicating the need for immediate intervention.






