Introduction
Atrial tachycardia and supraventricular tachycardia (SVT) are often mistaken for one another, yet they are distinct cardiac conditions with unique origins and implications. Understanding the differences between these two types of arrhythmias is essential for accurate diagnosis and effective treatment. Misinterpretations can lead to serious health consequences, making it crucial for healthcare professionals to differentiate between them.
What are the key characteristics that set atrial tachycardia apart from SVT? Recognizing these differences can significantly improve patient outcomes. This article explores the critical distinctions between these arrhythmias, examining their mechanisms, symptoms, triggers, and management strategies. By gaining a clearer understanding of these conditions, healthcare providers can enhance their ECG analysis and ultimately provide better care for their patients.
Origin and Mechanism of Atrial Tachycardia vs SVT
Atrial arrhythmia (AT) raises the question of whether atrial tachycardia is the same as SVT, as it is a specific type of supraventricular arrhythmia marked by rapid heart rates, usually exceeding 100 beats per minute, originating from ectopic foci within the atria. SVT is a broad term that encompasses various rapid heart rhythms that arise above the ventricles, and this leads to the question: is atrial tachycardia the same as SVT, including atrioventricular nodal reentrant rhythm (AVNRT) and atrioventricular reentrant rhythm (AVRT). Understanding the mechanisms behind these arrhythmias is essential for accurate diagnosis and tailored treatment strategies, as management approaches can differ significantly based on the underlying cause.
MaxYield™ from Neural Cloud Solutions offers advanced tools that enhance the analysis of these conditions. This platform automates ECG labeling and data extraction, enabling rapid identification of key features in every heartbeat, such as P-wave, QRS complex, and T-wave intervals. The automation streamlines the diagnostic process, reduces operational costs, and improves workflow efficiency, allowing healthcare professionals to concentrate on critical decision-making.
Key features of MaxYield™ include:
- Automated ECG labeling: Speeds up the identification of heart rhythm characteristics.
- Data extraction: Facilitates quick access to essential information.
- Beat-by-beat analysis: Processes up to 200,000 heartbeats in less than 5 minutes.
These features significantly boost productivity and accuracy in ECG analysis. By leveraging MaxYield™, healthcare professionals can enhance their diagnostic capabilities, ultimately leading to better patient outcomes.

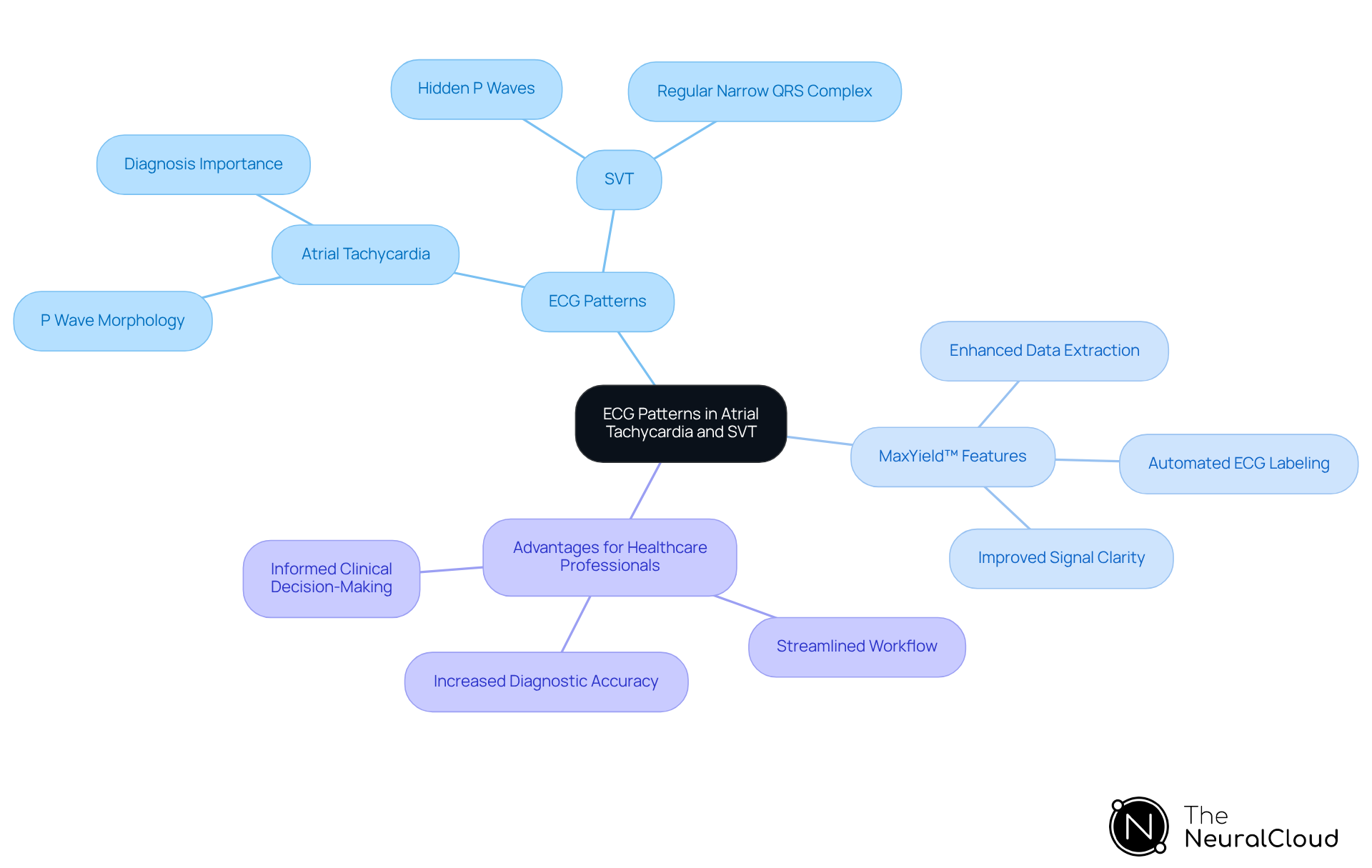
Electrocardiogram (ECG) Patterns in Atrial Tachycardia and SVT
Atrial arrhythmia is marked by distinct P waves preceding each QRS complex, often showing varying morphology due to their ectopic origin. This clear identification of P waves is crucial for accurate diagnosis. In contrast, when considering whether atrial tachycardia is the same as SVT, supraventricular arrhythmia (SVT) may present with hidden P waves or a regular narrow QRS complex, complicating the identification of the underlying rhythm.
Recent studies reveal that a rapid sinus heart rate is the most common ECG abnormality in acute pulmonary embolism, occurring in 31% of patients, while the S1Q3T3 pattern is noted in 15% of cases. Understanding whether atrial tachycardia is the same as SVT in these ECG patterns is vital for precise diagnosis and effective management of both rapid heart rhythms, as misinterpretation can lead to inappropriate treatment approaches. Current guidelines stress the importance of meticulous ECG analysis to differentiate between these conditions, particularly addressing the question of whether atrial tachycardia is the same as SVT, underscoring the need to recognize the unique characteristics of each rhythm.
The MaxYield™ platform from Neural Cloud Solutions offers advanced features that significantly enhance ECG analysis. By automating ECG labeling and data extraction, it reduces noise and improves signal clarity. This AI-powered method optimizes workflow, enabling healthcare practitioners to make informed clinical decisions based on accurate ECG analyses, particularly when evaluating if atrial tachycardia is the same as SVT.
Key Features of MaxYield™:
- Automated ECG labeling
- Enhanced data extraction
- Improved signal clarity
Advantages for Healthcare Professionals:
- Streamlined workflow
- Increased diagnostic accuracy
- Informed clinical decision-making
In summary, utilizing the MaxYield™ platform not only simplifies the ECG analysis process but also empowers healthcare professionals to deliver better patient care through precise and reliable diagnostics.
Clinical Presentation and Symptoms of Atrial Tachycardia vs SVT
Patients with atrial arrhythmia (AT) often report symptoms like palpitations, dizziness, and fatigue. While these symptoms can be concerning, they tend to be less severe than those experienced during episodes of supraventricular tachycardia (SVT). In contrast, SVT typically presents with more intense symptoms, such as chest pain, syncope, and increased anxiety due to the rapid heart rate.
Research shows that the prevalence of symptoms in individuals with SVT can significantly affect their quality of life, with many noting a decline in daily functioning. Understanding these differences in clinical presentation is vital for timely and appropriate interventions. If left untreated, SVT can lead to serious complications, including heart failure and thromboembolic events.
Recent studies highlight that effective management of SVT can improve outcomes for patients and enhance their overall quality of life. This underscores the importance of accurate diagnosis and tailored treatment strategies.

Triggers and Risk Factors for Atrial Tachycardia and SVT
Understanding the triggers for rapid heart rate is crucial for effective management. Common factors include:
- Excessive caffeine intake
- Alcohol consumption
- Emotional stress
These elements can lead to increased heart rates, impacting overall health.
In contrast, the question of whether atrial tachycardia is the same as SVT may also arise as these same factors can trigger both conditions. However, it can additionally be linked to structural heart abnormalities or electrolyte imbalances. Recognizing these triggers allows individuals to take proactive steps in managing their conditions.
By comprehending the underlying causes, patients can work towards reducing the frequency of episodes. This knowledge empowers them to make informed lifestyle choices, ultimately leading to better health outcomes.

Treatment Options for Atrial Tachycardia vs SVT
Management of rapid heartbeats involves a comprehensive strategy that includes antiarrhythmic drugs, catheter ablation, and lifestyle modifications to minimize triggers. In contrast, when considering the acute management of supraventricular tachycardia (SVT), one may wonder, is atrial tachycardia the same as SVT, as it typically utilizes vagal maneuvers or medications such as adenosine to restore normal heart rhythm? For those experiencing recurrent SVT, long-term management may incorporate beta-blockers or catheter ablation. This procedure has shown an initial success rate of approximately:
- 60% for tachycardia
- 80% for fibrillation
- 89.7% for typical flutter
Recent studies indicate that nearly 70% of individuals remain free from arrhythmia recurrence five years after undergoing multiple ablation procedures, while about 50.6% achieve this outcome following a single ablation. However, it is crucial to consider the long-term risks associated with catheter ablation, which include:
- 6.0% incidence of death
- 2.4% risk of stroke
- 1.2% chance of major bleeding within five years
Understanding these treatment pathways and their associated risks is vital for healthcare professionals aiming to enhance patient outcomes and effectively manage arrhythmias.

Acute Management Strategies for Atrial Tachycardia and SVT
Managing rapid heart rhythm effectively requires a clear understanding of acute interventions. Vagal maneuvers, such as the Valsalva maneuver, are often the first line of action for hemodynamically stable individuals, as they can successfully terminate episodes. In cases of supraventricular arrhythmia (SVT), the immediate administration of adenosine is crucial. This first-line treatment boasts a success rate of approximately 80.1% in restoring normal rhythm within seconds, which is vital for preventing hemodynamic instability and reducing the risk of complications.
Current guidelines, including those from the European Resuscitation Council, underscore the importance of these interventions as essential components of emergency protocols. Healthcare professionals must act swiftly to manage these arrhythmias effectively. However, it is critical to note that adenosine is contraindicated in patients with Wolff-Parkinson-White (WPW) syndrome and heart fibrillation due to the potential risk of dangerous ventricular arrhythmias.
Research indicates that adenosine remains a preferred choice in emergency settings, especially when compared to electrical cardioversion (ECV), which has a slightly higher success rate of 83.9%. Understanding these treatment options and their implications is essential for healthcare providers to ensure optimal patient outcomes.

Long-Term Monitoring for Atrial Tachycardia vs SVT
Long-term monitoring of atrial arrhythmia often relies on Holter monitors or event recorders, which are crucial for capturing episodes and analyzing their frequency. For patients with supraventricular tachycardia (SVT), continuous monitoring is vital to evaluate treatment efficacy and adjust management strategies. However, recent studies indicate that short-term Holter monitoring frequently fails to identify actionable arrhythmias. In fact, 64% of individuals experiencing daily symptoms encounter undetected actionable arrhythmias within the first 48 hours. This highlights the necessity for extended monitoring solutions, such as the Zio long-term continuous monitoring (LTCM) system, which allows for uninterrupted data collection for up to 14 days.
Advancements in monitoring technology not only enhance diagnostic accuracy but also play a pivotal role in optimizing patient care and significantly improving quality of life. One such advancement is Neural Cloud Solutions' MaxYield™ platform, which offers automated ECG analysis with advanced noise reduction and artifact handling. This capability enables clearer signal interpretation, even in challenging conditions.
Features of MaxYield™:
- Automated ECG analysis
- Advanced noise reduction
- Artifact handling
- Beat-by-beat analysis
- Ability to salvage obscured sections of recordings
These features ensure comprehensive patient assessment, allowing healthcare providers to make informed decisions. By integrating long-term monitoring solutions like Zio LTCM and MaxYield™ into their practice, healthcare professionals can significantly enhance their ECG analysis capabilities, ultimately leading to better patient outcomes.

Quality of Life Impact of Atrial Tachycardia and SVT
Patients experiencing rapid heartbeats often face significant anxiety and a diminished quality of life due to the unpredictable nature of their episodes. Research indicates that individuals with supraventricular tachycardia (SVT) similarly report high levels of distress, which can severely limit their daily activities. For instance, studies show that the frequency and duration of SVT episodes correlate negatively with health-related quality of life (hrQoL) scores, highlighting the emotional burden these conditions impose.
Approximately 27% of individuals with SVT have reported ceasing driving due to fears of episodes, further illustrating the profound impact on their lifestyle. Addressing these quality of life concerns is crucial for healthcare providers. Integrating mental health support into treatment plans can significantly enhance individual outcomes and overall well-being. Recent findings emphasize the importance of ongoing observation and customized interventions to improve the quality of life for individuals managing these arrhythmias.

Lifestyle Modifications for Managing Atrial Tachycardia and SVT
Lifestyle changes are crucial for managing heart rhythm disorders, especially when considering if atrial tachycardia is the same as SVT. Key strategies include:
- Reducing caffeine and alcohol intake, as these substances can worsen arrhythmias.
- Stress management techniques, such as relaxation exercises and mindfulness practices, significantly alleviate symptoms.
- A balanced diet rich in whole grains and lean proteins, while avoiding high-cholesterol foods, supports overall heart health.
- Regular exercise, tailored to individual capabilities, strengthens the heart and enhances its function.
Research indicates that these lifestyle changes not only reduce triggers but also empower individuals to take control of their conditions, leading to improved outcomes and quality of life. For example, studies show that adopting healthier sleep habits and effectively managing weight can reduce the frequency and severity of arrhythmias. Dr. William Sauer, a cardiac electrophysiologist, emphasizes the importance of these changes: "Certain lifestyle changes, such as improved sleep habits, limiting caffeine and alcohol, and maintaining a healthy body weight have all been shown to reduce arrhythmia burden."
By implementing these changes, individuals can significantly enhance their heart health and more effectively manage rapid heartbeats, particularly when considering if atrial tachycardia is the same as SVT.

Diagnosis Accuracy and Complications of Atrial Tachycardia vs SVT
Accurate diagnosis of conditions relies on understanding if atrial tachycardia is atrial tachycardia the same as SVT. Misdiagnosis can lead to inappropriate treatment and increased risks of complications, such as heart failure and stroke. A study involving 119 individuals found that documented SVT was induced in 55% of subjects during electrophysiological studies, highlighting the need for precise identification.
To improve diagnostic accuracy, healthcare providers can utilize advanced diagnostic tools like electrocardiograms (ECGs) and continuous monitoring systems. One such tool is Neural Cloud Solutions' MaxYield™ platform, which offers automated ECG analysis. This platform effectively maps ECG signals through noise, isolating and labeling key features in every heartbeat.
Features of MaxYield™:
- Automated ECG analysis
- Noise filtering to isolate key features
- Beat-by-beat analysis of heartbeats
- Insights from 200,000 heartbeats in under 5 minutes
The advantages of using MaxYield™ are significant. Its continuous learning model ensures that accuracy and efficiency improve over time, reducing the likelihood of misdiagnosis. By integrating MaxYield™ into clinical practice, healthcare providers can enhance clarity and efficiency in ECG interpretation. This ultimately leads to improved patient outcomes and minimizes the risks associated with untreated arrhythmias.

Conclusion
Atrial tachycardia and supraventricular tachycardia (SVT) may exhibit rapid heart rates, yet they are distinct conditions with unique origins, mechanisms, and clinical implications. Understanding these differences is vital for accurate diagnosis and effective management. Misinterpretation can lead to inappropriate treatment strategies, potentially impacting patient outcomes negatively.
Key points highlighted throughout the article include:
- The distinct ECG patterns associated with each condition
- Their varying clinical presentations and symptoms
- The triggers and risk factors that can exacerbate episodes
Treatment options differ significantly, with management strategies tailored to the unique characteristics of atrial tachycardia and SVT. Long-term monitoring and lifestyle modifications also play crucial roles in enhancing patient quality of life and reducing the frequency of arrhythmia episodes.
Recognizing the differences between atrial tachycardia and SVT is essential for healthcare professionals and patients alike. By fostering an understanding of these conditions, individuals can take proactive steps toward better heart health, informed lifestyle choices, and timely medical interventions. Emphasizing accurate diagnosis and tailored treatment plans will not only enhance patient outcomes but also empower individuals to manage their conditions effectively, leading to improved overall well-being.
Frequently Asked Questions
What is the difference between atrial tachycardia and supraventricular tachycardia (SVT)?
Atrial tachycardia is a specific type of supraventricular arrhythmia characterized by rapid heart rates, usually exceeding 100 beats per minute, originating from ectopic foci within the atria. SVT is a broader term that includes various rapid heart rhythms originating above the ventricles, including atrioventricular nodal reentrant rhythm (AVNRT) and atrioventricular reentrant rhythm (AVRT).
Why is it important to understand the mechanisms behind atrial tachycardia and SVT?
Understanding the mechanisms is essential for accurate diagnosis and tailored treatment strategies, as management approaches can differ significantly based on the underlying cause of the arrhythmias.
What tools does MaxYield™ from Neural Cloud Solutions provide for analyzing atrial tachycardia and SVT?
MaxYield™ offers advanced tools for automated ECG labeling and data extraction, enabling rapid identification of key features in every heartbeat and streamlining the diagnostic process.
What are the key features of the MaxYield™ platform?
Key features include automated ECG labeling, data extraction for quick access to essential information, and beat-by-beat analysis of up to 200,000 heartbeats in less than 5 minutes.
How do ECG patterns differ between atrial tachycardia and SVT?
Atrial tachycardia typically shows distinct P waves preceding each QRS complex, which may have varying morphology due to their ectopic origin. In contrast, SVT may present with hidden P waves or a regular narrow QRS complex, making it more challenging to identify the underlying rhythm.
What symptoms do patients experience with atrial tachycardia compared to SVT?
Patients with atrial tachycardia often report symptoms like palpitations, dizziness, and fatigue, which tend to be less severe than the more intense symptoms experienced during episodes of SVT, such as chest pain, syncope, and increased anxiety.
How does SVT affect a patient's quality of life?
The prevalence of symptoms in individuals with SVT can significantly affect their quality of life, leading to a decline in daily functioning. Untreated SVT can result in serious complications, including heart failure and thromboembolic events.
What is the importance of accurate diagnosis in managing atrial tachycardia and SVT?
Accurate diagnosis is vital for timely and appropriate interventions, as effective management of SVT can improve patient outcomes and enhance their overall quality of life.


