Overview
This article provides key insights into the differences between anterior and posterior STEMI, emphasizing their importance for health tech developers. It outlines the challenges in ECG analysis, particularly the need for accurate diagnosis due to the distinct ECG patterns associated with each type. These differences can significantly influence treatment decisions and patient outcomes.
The MaxYield™ platform plays a crucial role in this context, enhancing ECG analysis and diagnostic precision through its advanced capabilities. By improving the accuracy of ECG readings, the MaxYield™ platform offers substantial benefits for healthcare professionals, ultimately leading to better patient care.
Introduction
Understanding the nuances between anterior and posterior ST-segment elevation myocardial infarction (STEMI) is vital for health tech developers aiming to enhance cardiac diagnostics. As advancements in technology reshape the landscape of ECG analysis, the MaxYield™ platform emerges as a game-changer. This platform offers automated solutions that significantly improve the accuracy and speed of ECG interpretation.
However, a critical challenge remains: how can developers ensure their tools effectively differentiate between these two types of STEMI to prevent misdiagnosis and optimize patient outcomes? Exploring these key insights can illuminate the path forward in cardiac care innovation.
Neural Cloud Solutions: MaxYield™ for Enhanced ECG Analysis
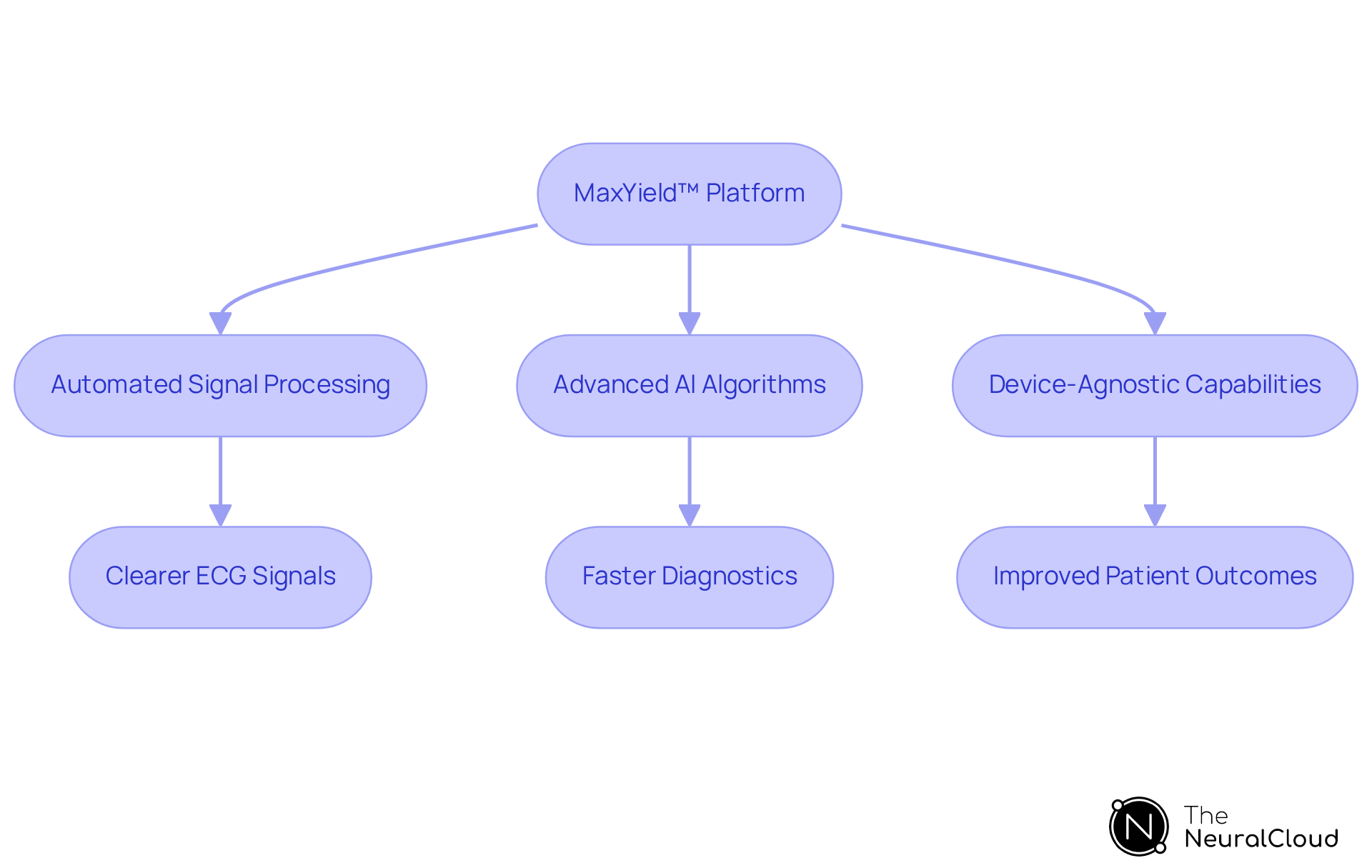
The MaxYield™ platform from Neural Cloud Solutions is leading a transformation in ECG analysis by automating cardiac signal processing. It addresses significant challenges in this field, such as noise and signal artifacts, which can obscure the clarity of ECG data. By utilizing advanced AI algorithms, MaxYield™ enhances the precision of ECG readings, facilitating the rapid and accurate identification of cardiac events. This capability is crucial for clinicians who depend on reliable data for informed decision-making.
MaxYield™ can process over 200,000 heartbeats in less than five minutes, showcasing its potential to revolutionize cardiac diagnostics. This efficiency makes it an essential tool for healthcare professionals and researchers alike. Additionally, the platform is device-agnostic, meaning it can effortlessly capture ECG recordings from any 1-lead or 3-lead device. As noted by Peter Kendall, President and Chief Commercial Officer of AIML, MaxYield™ effectively tackles core challenges in digital health by delivering clearer ECG signals, even in noisy, real-world conditions.
The advancements represented by MaxYield™ not only streamline clinical workflows but also enhance the overall quality of cardiac care. By providing clearer and more reliable ECG data, it empowers healthcare providers to make better-informed decisions, ultimately leading to improved patient outcomes. This innovative technology exemplifies the future of cardiac diagnostics, making it a vital asset in the field.
Anterior STEMI: Key ECG Patterns and Characteristics
The differences in ECG alterations between anterior vs posterior STEMI are particularly evident in the precordial electrodes (V1-V6). Key patterns include significant ST segment elevation, especially in V2 and V3, often accompanied by Q waves in these areas, indicating substantial myocardial injury. Recent studies reveal that hyperacute T waves frequently precede these changes, serving as early indicators of occlusive myocardial infarction. The presence of ST elevation exceeding 1 mm in two contiguous leads is a critical criterion for diagnosis, with specific thresholds for leads V2 and V3 based on patient demographics.
Health tech developers face challenges in accurately identifying these ECG patterns, making timely detection essential for improving patient outcomes in clinical settings. The occurrence of anterior myocardial infarction in emergency departments underscores the necessity for robust diagnostic instruments that enable swift intervention, ultimately enhancing the effectiveness of cardiac care. Neural Cloud Solutions' MaxYield™ platform addresses these challenges by leveraging gold standard methodologies, noise filtering, and automation, streamlining the workflow for ECG analysis.
The MaxYield™ platform provides several key features:
- It employs advanced algorithms for ECG interpretation.
- It enhances accuracy through noise reduction.
- It automates labeling processes.
These features offer significant advantages, including improved diagnostic precision, reduced analysis time, and cost-effectiveness for healthcare providers. By integrating wearable technology with MaxYield™, developers can further enhance automated labeling and reduce costs, improving the overall accuracy and efficiency of ECG analysis.
Moreover, the De Winter pattern, characterized by ST-depression at the J point and prominent positive T waves, suggests proximal left anterior descending artery blockage. This pattern should be acknowledged as part of the range of ECG alterations linked to anterior vs posterior STEMI. By focusing on these critical aspects, the MaxYield™ platform not only improves ECG analysis but also supports healthcare professionals in delivering timely and effective cardiac care.

Posterior STEMI: Unique ECG Features and Indicators
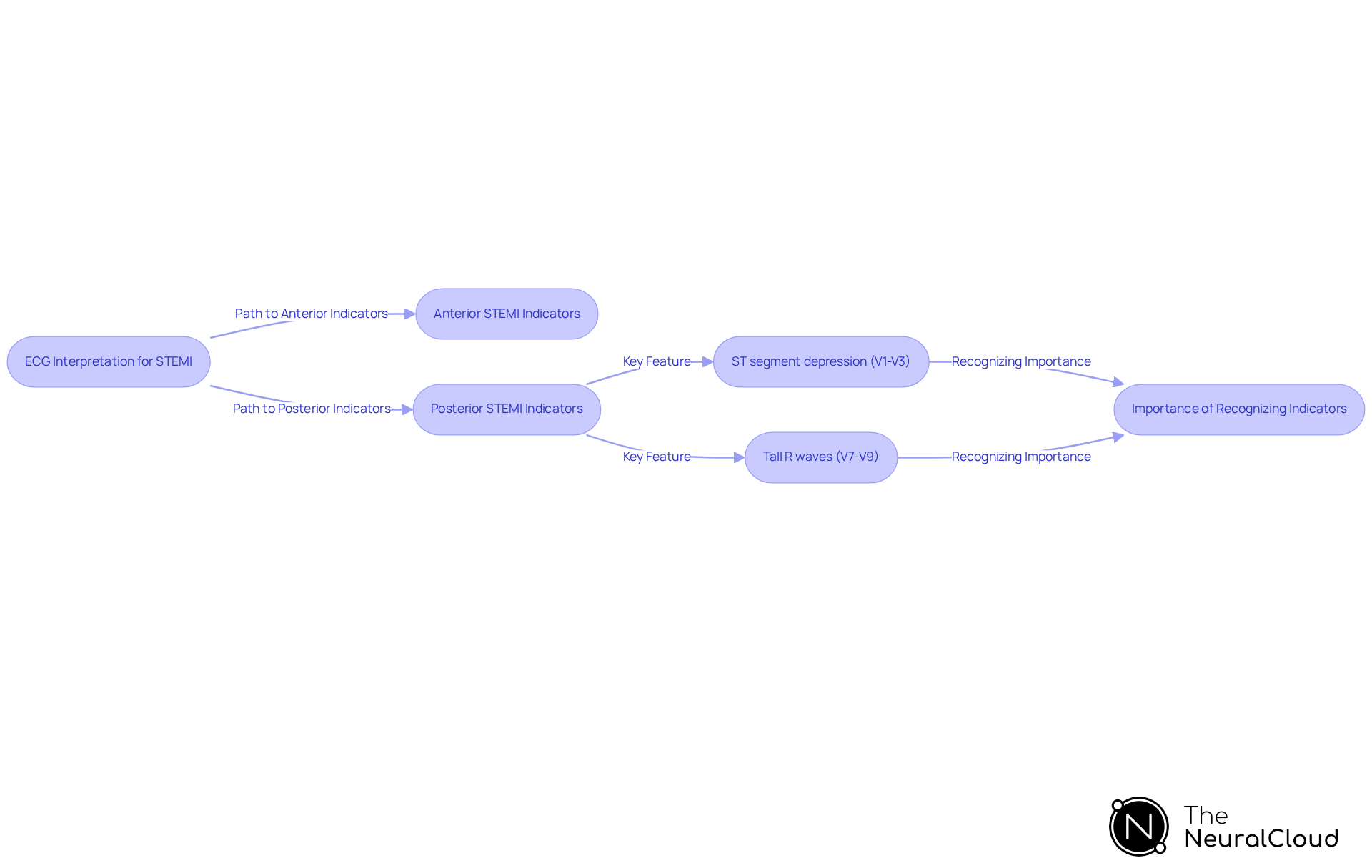
The distinction between anterior vs posterior STEMI is important, as posterior STEMI often presents with subtle ECG changes that can be easily overlooked, making accurate diagnosis critical. Key indicators include:
- ST segment depression in the context of anterior vs posterior STEMI positions (V1-V3)
- Tall R waves in positions V7-V9, located on the back
These characteristics can be difficult to recognize, particularly when back myocardial infarction occurs alone or as a continuation of inferior or lateral MIs, which account for up to 20% of acute MIs. Recognizing these indicators is essential, as misinterpretation can delay treatment and increase the risk of complications.
MaxYield™ transforms lengthy and noisy ECG recordings into clean, crisp signals, leveraging cutting-edge AI technology for clarity and speed in ambulatory ECG waveform analysis. Real-world examples illustrate the role of advanced algorithms in enhancing the visibility of these indicators in ECG readings. For instance, the PMcardio AI model has demonstrated a significant improvement in diagnostic accuracy, achieving approximately 89% accuracy in ECG interpretation compared to 65% for physicians. This underscores the capability of AI, such as MaxYield™, to assist healthcare practitioners in real-time clinical decision-making, particularly in recognizing back wall myocardial infarction.
Cardiologists emphasize the challenges in identifying back wall myocardial infarction, noting that the conventional 12-lead ECG may not adequately capture the subtleties of rear wall ischemia. As one specialist stated, 'Clinical suspicion for an anterior vs posterior STEMI should remain elevated with any level of ST segment depression in the anterior electrodes.' This highlights the necessity for health tech developers to innovate and create algorithms that can effectively analyze ECG data, ensuring timely and accurate diagnosis of heart attacks. Testimonials from users of MaxYield™ further validate its effectiveness, demonstrating how it has transformed their ECG analysis processes. For practical guidance on utilizing MaxYield™, please refer to the user manuals available on our website.
Clinical Implications: Risks of Misdiagnosing Anterior vs Posterior STEMI
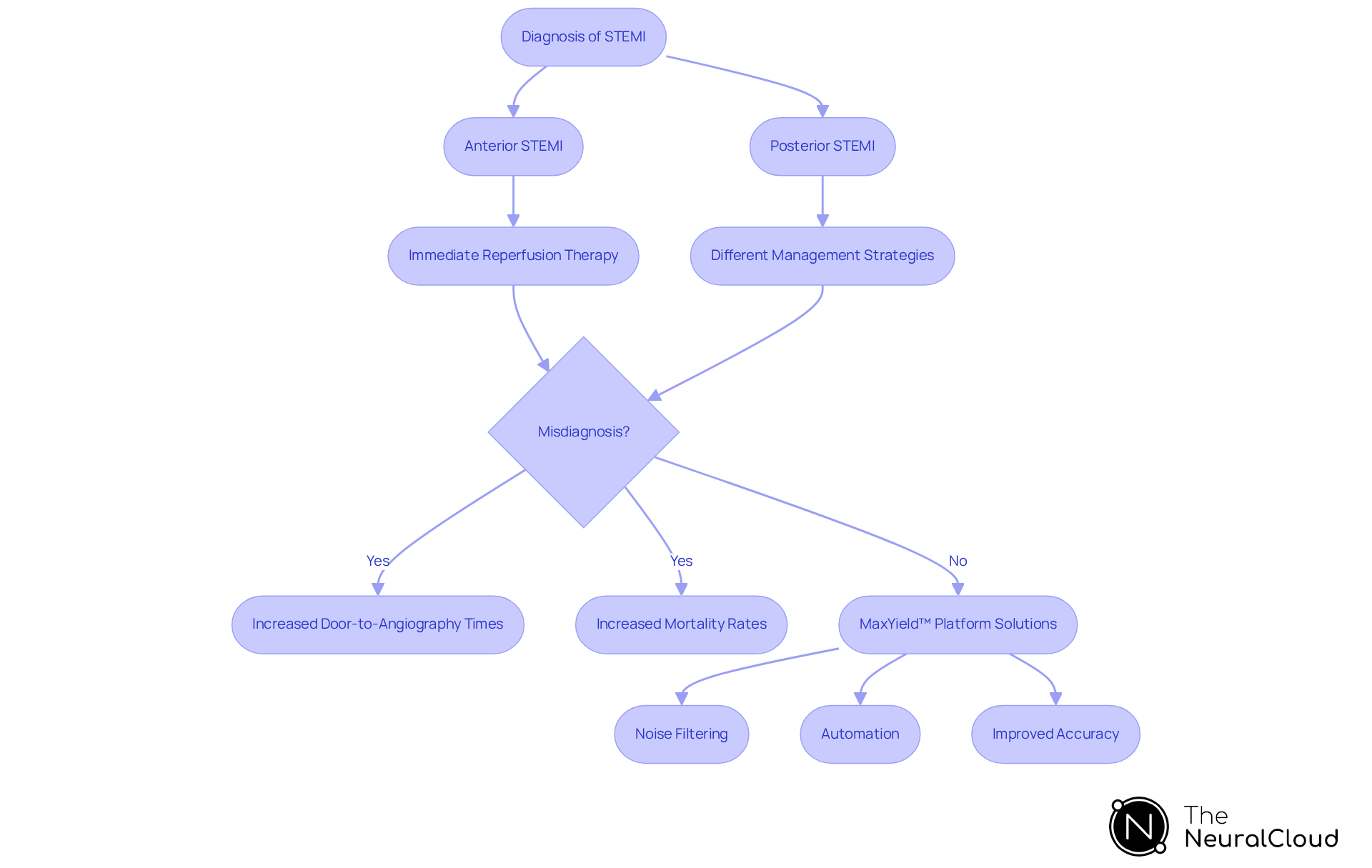
Misdiagnosing anterior vs posterior STEMI can lead to serious clinical outcomes, including delayed treatment and increased mortality rates. The distinction between anterior vs posterior STEMI highlights that anterior myocardial infarction typically necessitates immediate reperfusion therapy, while posterior myocardial infarction may require different management strategies. Studies indicate that misdiagnosis can result in a five-fold increase in door-to-angiography times, directly impacting patient outcomes. For instance, patients incorrectly diagnosed with a heart attack experienced a median door-to-angiography time of 220 minutes, compared to just 43 minutes for those diagnosed accurately. This delay can exacerbate the risk of irreversible heart damage, emphasizing the urgency of accurate diagnosis.
Health tech developers must prioritize precision in their diagnostic tools to mitigate these risks, ensuring healthcare professionals can rely on accurate ECG interpretations for swift decision-making. The need for enhanced diagnostic precision is further underscored by the fact that nearly 10% of heart attack patients do not present with typical chest pain, complicating prompt diagnosis. As Dr. Chris Gale observes, shifting perceptions about heart attack symptoms is essential, as heart attacks impact a wider demographic than traditionally assumed. Improving the precision of heart attack diagnosis is vital not only for better treatment outcomes but also for optimizing resource allocation in healthcare settings.
Neural Cloud Solutions' MaxYield™ platform addresses these challenges by enhancing ECG workflow efficiency through gold standard noise filtering and automation. The platform effectively manages physiological variability and signal artifacts, which are common obstacles in ECG analysis. This leads to improved diagnostic accuracy, enabling healthcare professionals to make informed decisions quickly. By focusing on the features of MaxYield™, such as advanced noise reduction and automated processes, the platform provides significant advantages. These include reduced door-to-angiography times and improved patient outcomes, ultimately benefiting both patients and healthcare providers.
ECG Leads: Diagnostic Tools for Anterior and Posterior STEMI
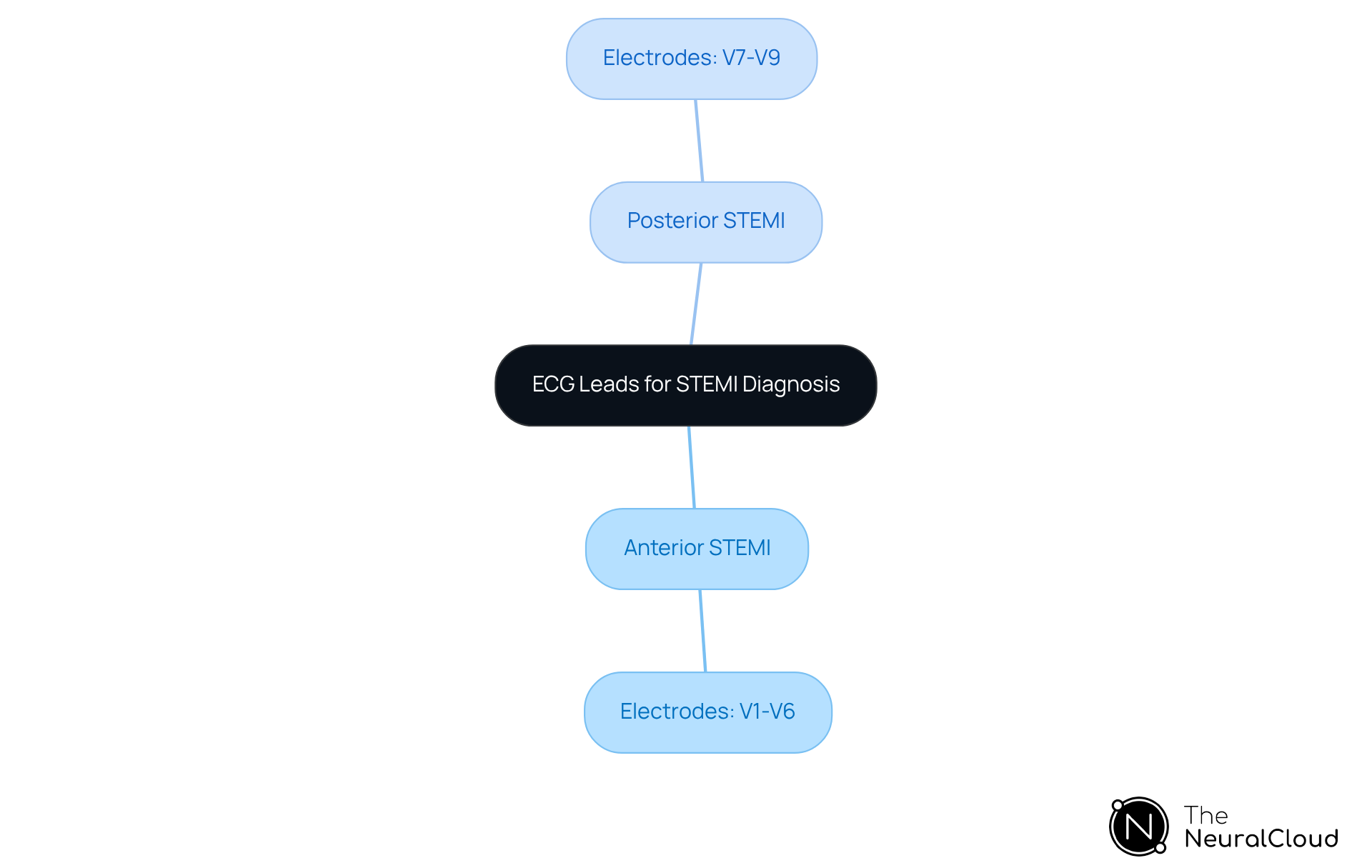
The choice of ECG electrodes is essential for accurately diagnosing anterior vs posterior STEMI. In the context of anterior vs posterior STEMI, standard electrodes V1-V6 are used for anterior myocardial infarction, effectively capturing the heart's anterior wall's electrical activity. Conversely, diagnosing posterior STEMI requires additional electrodes on the rear, specifically V7-V9, to detect changes indicative of inferior wall involvement when considering anterior vs posterior STEMI.
Recent studies highlight that employing these posterior electrodes can significantly improve the detection of myocardial infarctions that might otherwise remain undetected with standard placements. Developers of ECG analysis tools should prioritize these electrode configurations, ensuring their systems deliver clear visualizations and interpretations to aid clinicians in making accurate diagnoses.
By incorporating advanced algorithms that consider the intricacies of lead placement, developers can improve diagnostic accuracy and overall effectiveness in ECG solutions, ultimately enhancing patient outcomes in acute myocardial infarction cases.
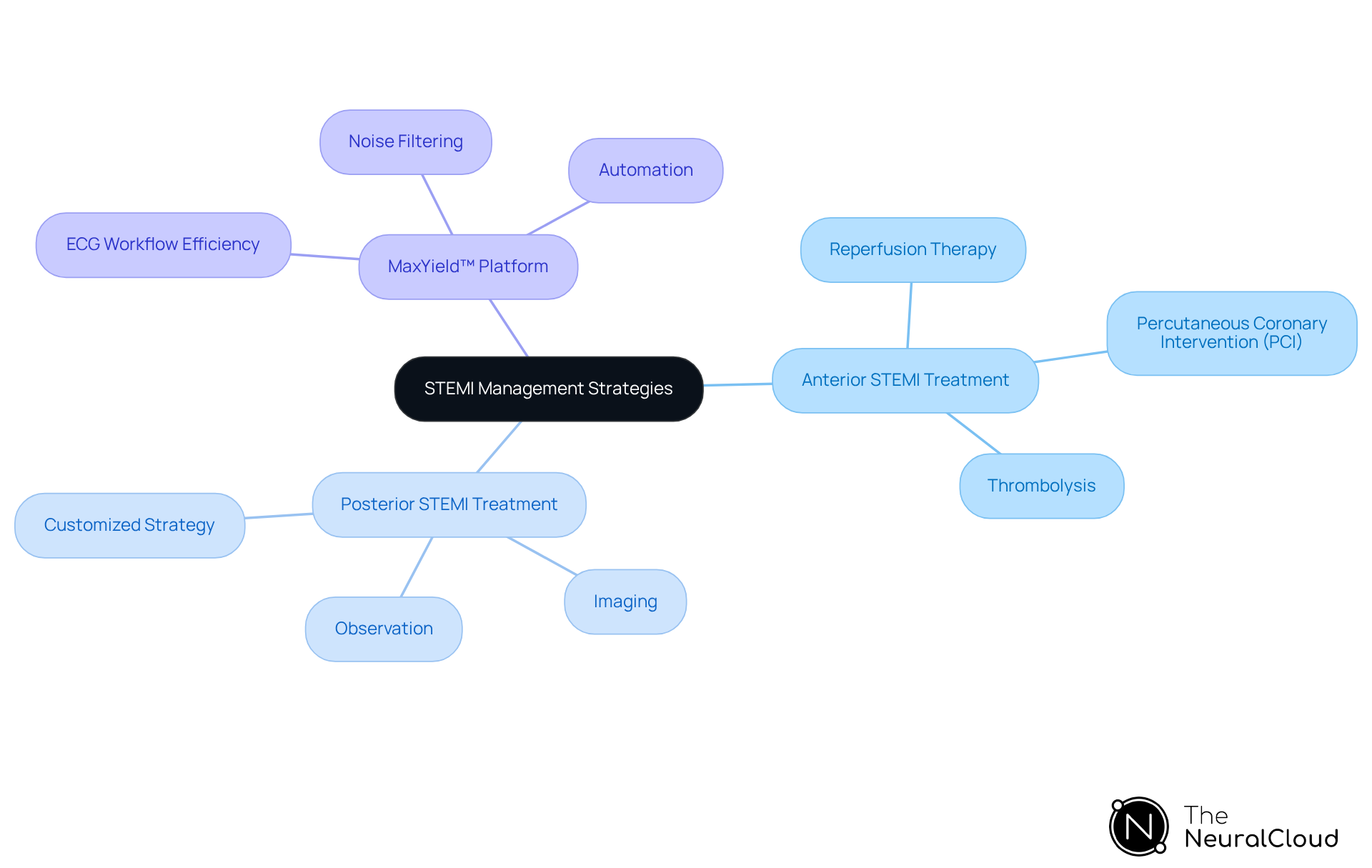
Treatment Strategies: Anterior vs Posterior STEMI Management
Treatment approaches for myocardial infarction differ significantly when considering anterior vs posterior STEMI. In the context of anterior vs posterior STEMI, anterior myocardial infarction typically requires immediate reperfusion therapy, such as percutaneous coronary intervention (PCI) or thrombolysis. In contrast, managing anterior vs posterior STEMI often necessitates a more customized strategy, which may involve further imaging or observation. Health tech developers should consider these treatment pathways when designing their diagnostic tools, ensuring they provide actionable insights that align with clinical protocols.
Integrating Neural Cloud Solutions' MaxYield™ platform can significantly enhance ECG workflow efficiency. This platform features gold standard noise filtering and automation, addressing challenges such as physiological variability and signal artifacts. By simplifying the analysis process, MaxYield™ facilitates prompt and precise decision-making in heart attack management. The benefits for healthcare professionals include improved accuracy in ECG interpretation and reduced time spent on analysis, ultimately leading to better patient outcomes.
In conclusion, the MaxYield™ platform not only streamlines ECG analysis but also empowers healthcare providers with the tools necessary for effective heart attack management. By focusing on these essential features and their advantages, developers can create diagnostic tools that truly meet the needs of clinical practice.
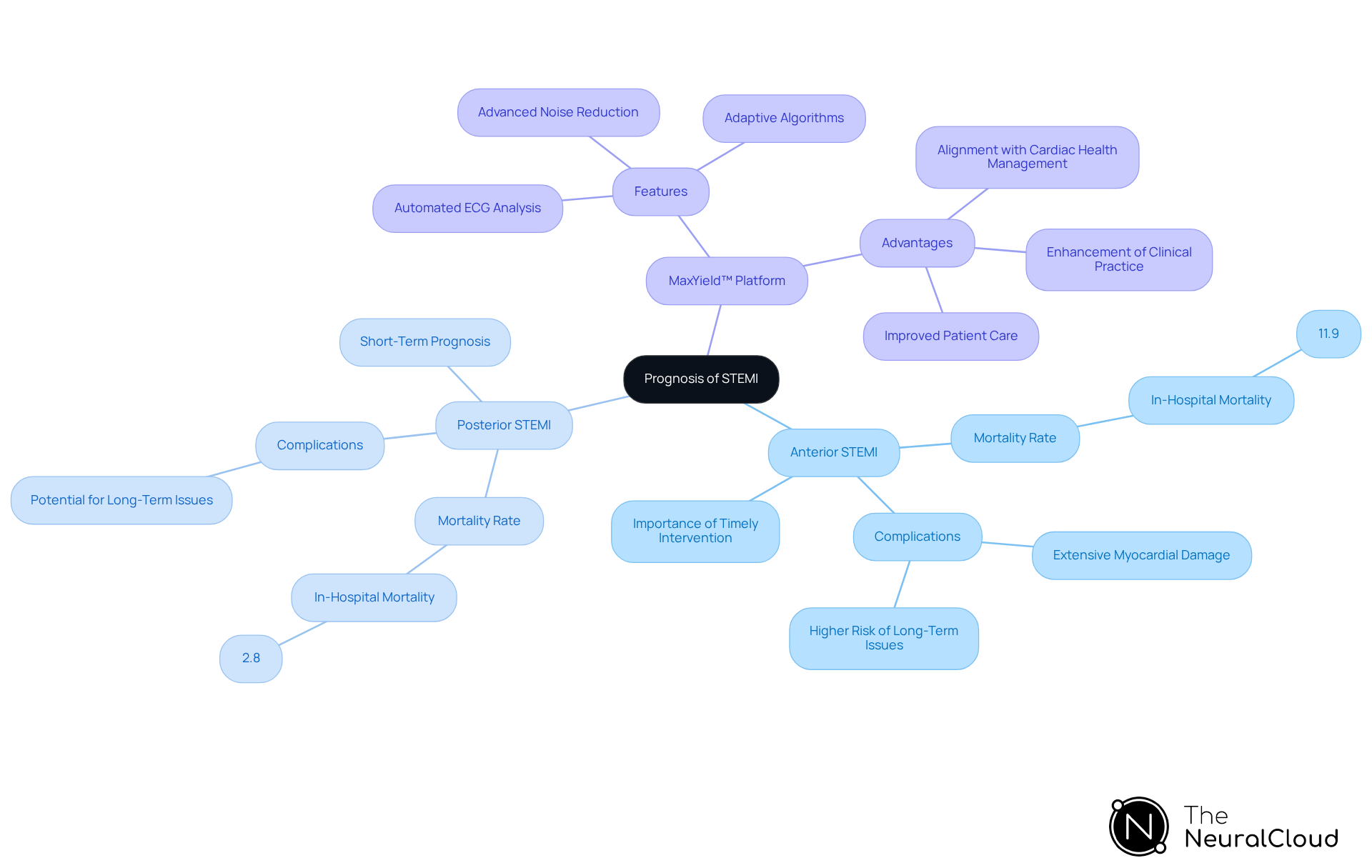
Prognosis: Comparing Outcomes of Anterior and Posterior STEMI
The outlook for heart attacks shows significant variations when comparing anterior vs posterior STEMI. In the context of anterior vs posterior STEMI, anterior cases are generally linked to increased mortality rates and more serious complications due to extensive myocardial damage. In-hospital mortality for anterior vs posterior STEMI is 11.9%, significantly higher than the 2.8% observed for inferior myocardial infarction. This disparity highlights the critical need for timely intervention, as the extent of coronary disease adversely affects long-term outcomes. Conversely, while posterior myocardial infarction may initially appear to have a better short-term prognosis than anterior vs posterior STEMI, it can lead to long-term complications if not managed effectively.
Recent studies indicate that up to 65% of heart attack patients may present with multivessel disease, complicating their management and outcomes. Therefore, developers should prioritize integrating robust prognostic analytics into their tools. For instance, Neural Cloud Solutions' MaxYield™ platform automates ECG analysis, enhancing diagnostic yield through advanced noise reduction and adaptive algorithms. By leveraging MaxYield™, clinicians can efficiently assess patient risk and tailor treatment plans.
The MaxYield™ platform offers several key features:
- It automates ECG analysis, which reduces the time required for interpretation.
- Advanced noise reduction ensures clearer signals, leading to more accurate diagnoses.
- Adaptive algorithms allow for real-time adjustments based on patient data, enhancing the overall effectiveness of ECG assessments.
The advantages of using MaxYield™ are significant:
- Healthcare professionals can improve patient care by making timely and informed decisions.
- The platform aligns with the evolving landscape of cardiac health management, ultimately contributing to better patient outcomes.
- By integrating such advanced tools, clinicians can enhance their practice, ensuring they meet the complex needs of heart attack patients.
Advanced Technologies: Enhancing STEMI Diagnosis with AI
Cutting-edge technologies, especially artificial intelligence (AI) and machine learning, are transforming the diagnosis of ST-segment elevation myocardial infarction. These innovations facilitate the analysis of extensive ECG datasets, enabling the identification of subtle patterns and anomalies that may elude human interpretation. For instance, Neural Cloud Solutions' MaxYield™ platform enhances long-form electrocardiogram (ECG) analysis through automated, distinct, and scalable methods, effortlessly capturing ECG recordings from any 1-lead or 3-lead device.
MaxYield™ effectively maps ECG signals through noise, isolating and labeling key features in every heartbeat, including P-wave, QRS complex, and T-wave onsets and offsets. This platform delivers beat-by-beat analysis of 200,000 heartbeats in less than 5 minutes, showcasing AI's potential to enhance diagnostic precision. Machine learning models within MaxYield™ demonstrate an impressive accuracy of 99.2% in detecting ventricular arrhythmias, underscoring the platform's reliability.
Industry leaders emphasize that AI transcends mere task automation; it unlocks personalized medicine and tailors treatments to individual patients. Furthermore, AI's integration into clinical decision-making processes, as exemplified by MaxYield™, significantly improves diagnostic accuracy and efficiency. Health technology creators are encouraged to leverage these advancements to develop tools that enhance diagnostic precision and efficiency, ultimately leading to improved patient outcomes in acute myocardial infarction cases.
Real-world applications of machine learning in ECG analysis have already shown promise. Studies indicate that AI can reduce false positives and negatives in diagnoses, thereby streamlining clinical workflows and enhancing patient care. However, the real-time deployment of AI models for prospective validation and clinical utility assessment remains critical for ongoing development in this field. Additionally, addressing challenges such as data privacy and the necessity for human expertise is essential for the successful integration of AI technologies in healthcare.

Educational Resources: Learning About Anterior and Posterior STEMI
Educational resources are essential for improving the understanding of anterior vs posterior STEMI myocardial infarction. These resources include:
- Research articles
- Case studies
- Interactive learning modules
These can significantly enhance the knowledge base of healthcare practitioners. By providing access to these materials, developers can improve diagnostic abilities and treatment outcomes in heart attack cases. Ultimately, equipping healthcare professionals with comprehensive educational tools leads to better patient care and more effective management of myocardial infarction.

Key Takeaways: Understanding Anterior vs Posterior STEMI
Understanding the distinctions between anterior vs posterior STEMI is crucial for accurate diagnosis and treatment. The differences in anterior vs posterior STEMI are evident as anterior myocardial infarction typically presents with ST-segment elevation in the precordial electrodes, while posterior myocardial infarction is characterized by reciprocal changes in the anterior electrodes. Misdiagnosis can result in significant clinical consequences, including delayed treatment and increased mortality rates. For example, timely reperfusion through primary percutaneous coronary intervention (PCI) within 120 minutes can lower mortality from 9% to 7%, highlighting the importance of precise diagnosis.
Health tech developers are encouraged to utilize advanced technologies, such as the MaxYield™ platform, to improve the accuracy and efficiency of STEMI diagnosis. This platform automates ECG analysis and employs gold standard methodologies for noise filtering, significantly enhancing signal clarity. As a result, clinicians can make informed decisions quickly. Real-world examples indicate that hospitals that adopt advanced ECG analysis have experienced improved patient outcomes, including reduced time to treatment and better management of acute coronary syndrome (ACS).
Cardiologists stress the importance of recognizing the differences in anterior vs posterior STEMI, as they have a direct impact on patient care. With over 7 million individuals diagnosed with ACS annually worldwide, the demand for precise diagnostic tools is more urgent than ever. By concentrating on these insights, developers can create solutions that not only streamline the diagnostic process but also ultimately enhance patient care.

Conclusion
Understanding the distinctions between anterior and posterior STEMI is vital for ensuring accurate diagnosis and effective treatment. These two types of myocardial infarction exhibit different ECG patterns: anterior STEMI typically shows significant ST-segment elevation in the precordial leads, while posterior STEMI often presents with more subtle, reciprocal changes. Misdiagnosis can lead to severe clinical repercussions, including delayed interventions and increased mortality. This underscores the importance of precise diagnostic tools in cardiac care.
The revolutionary capabilities of Neural Cloud Solutions' MaxYield™ platform enhance ECG analysis through advanced AI-driven noise reduction and automation. This technology improves diagnostic accuracy and streamlines clinical workflows, allowing healthcare providers to make timely decisions that can significantly impact patient outcomes. Health tech developers must focus on these differences and the associated risks, advocating for the integration of educational resources to bolster the understanding of these conditions among healthcare professionals.
The ongoing development and implementation of innovative diagnostic technologies like MaxYield™ are essential for improving the management of acute myocardial infarctions. As the demand for precise and efficient diagnostic tools grows, prioritizing the understanding of anterior versus posterior STEMI will be crucial in enhancing patient care and outcomes. By leveraging advanced technologies and fostering education in this field, healthcare practitioners can ensure they are well-equipped to address the complexities of heart attack diagnosis and treatment effectively.
Frequently Asked Questions
What is MaxYield™ and how does it enhance ECG analysis?
MaxYield™ is a platform from Neural Cloud Solutions that automates cardiac signal processing to improve ECG analysis. It utilizes advanced AI algorithms to enhance the precision of ECG readings, addressing challenges such as noise and signal artifacts, which can obscure ECG data.
What are the processing capabilities of MaxYield™?
MaxYield™ can process over 200,000 heartbeats in less than five minutes, making it an efficient tool for healthcare professionals and researchers involved in cardiac diagnostics.
Is MaxYield™ compatible with different ECG devices?
Yes, MaxYield™ is device-agnostic and can capture ECG recordings from any 1-lead or 3-lead device.
What are the key features of the MaxYield™ platform?
Key features of MaxYield™ include advanced algorithms for ECG interpretation, noise reduction to enhance accuracy, and automation of labeling processes.
How does MaxYield™ improve patient outcomes in emergency settings?
By providing clearer and more reliable ECG data, MaxYield™ empowers healthcare providers to make better-informed decisions, which is crucial for timely interventions in cases of myocardial infarction.
What are the key ECG patterns associated with anterior STEMI?
Key patterns include significant ST segment elevation in leads V2 and V3, often accompanied by Q waves, and hyperacute T waves that may precede these changes.
What challenges do health tech developers face in identifying ECG patterns?
Health tech developers face challenges in accurately identifying ECG patterns, particularly in the context of anterior and posterior STEMI, which is essential for timely detection and improving patient outcomes.
What unique ECG features are associated with posterior STEMI?
Unique features include ST segment depression in leads V1-V3 and tall R waves in leads V7-V9, located on the back.
How does MaxYield™ assist in recognizing back wall myocardial infarction?
MaxYield™ enhances the visibility of subtle ECG changes through advanced AI technology, improving diagnostic accuracy and assisting healthcare practitioners in real-time clinical decision-making.
Where can users find practical guidance on utilizing MaxYield™?
Users can refer to the user manuals available on the Neural Cloud Solutions website for practical guidance on utilizing the MaxYield™ platform.


