Overview
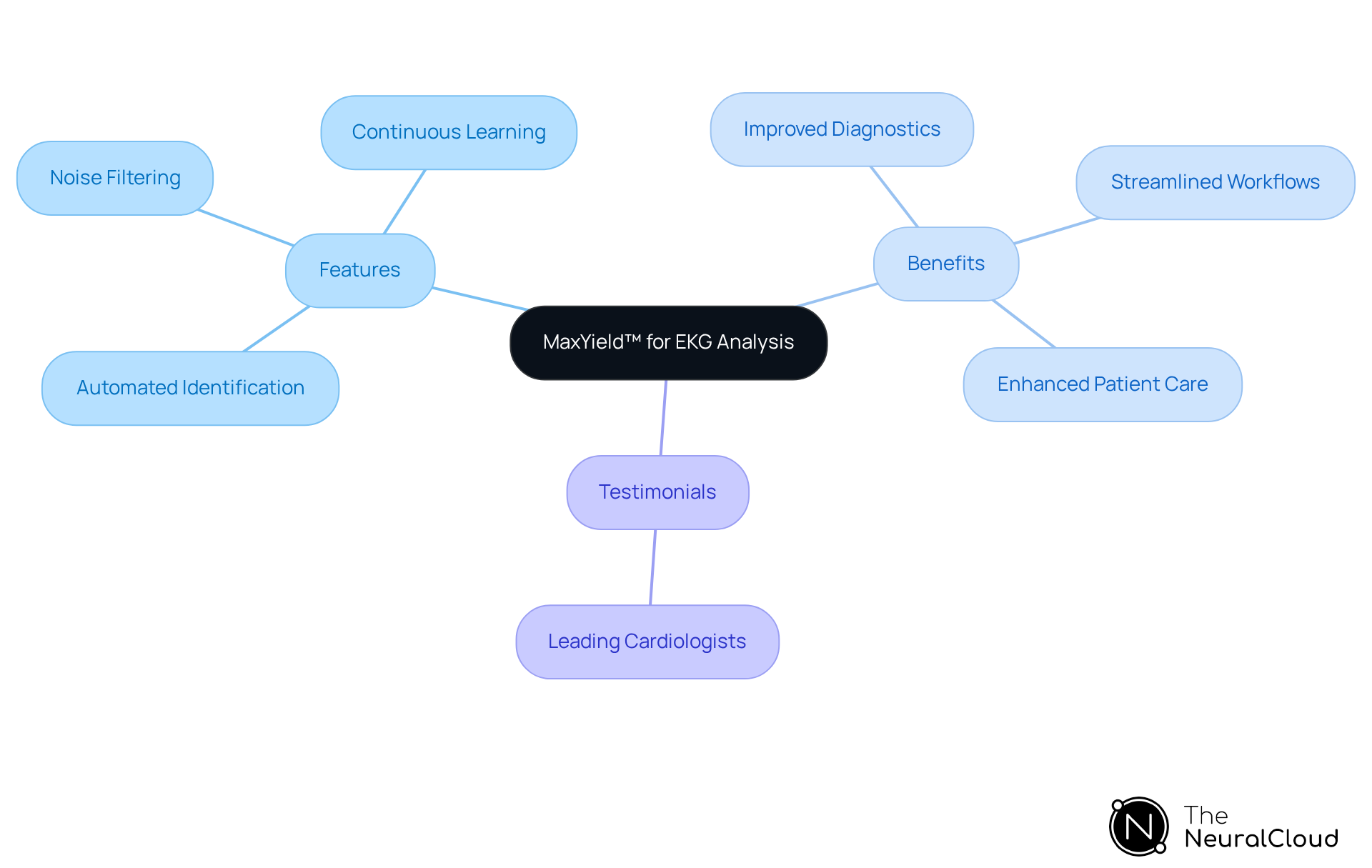
The primary objective of this article is to deliver essential insights regarding junctional rhythm EKG, specifically tailored for health tech developers. It highlights the transformative impact of Neural Cloud Solutions' MaxYield™ platform, which enhances EKG analysis through AI-driven automation. This innovation not only boosts diagnostic accuracy but also streamlines clinical workflows, ultimately leading to improved patient care.
Introduction
The world of cardiac health is rapidly evolving, with junctional rhythm EKG analysis leading this transformation. Healthcare professionals face significant challenges in achieving precision in diagnostics, making it essential to understand the nuances of junctional rhythms. This article explores ten key insights that highlight the importance of junctional rhythm EKGs. Additionally, it showcases how advanced technologies, such as Neural Cloud Solutions' MaxYield™, are revolutionizing cardiac monitoring. Clinicians encounter obstacles in accurately interpreting these rhythms, and innovative solutions can pave the way for improved patient outcomes.
Neural Cloud Solutions: MaxYield™ for Enhanced Junctional Rhythm EKG Analysis
Neural Cloud Solutions' MaxYield™ platform is at the forefront of transforming EKG analysis by automating the identification and labeling of essential features within ECG signals. This advanced technology can in under five minutes, enabling healthcare professionals to quickly and precisely assess junctional rhythm EKG patterns.
By leveraging sophisticated AI algorithms, MaxYield™ significantly enhances the clarity of ECG signals, which leads to more reliable diagnostics and streamlined clinical workflows. The platform's advanced noise filtering capabilities allow it to effectively manage noise and signal artifacts, addressing critical pain points in ECG analysis.
MaxYield™ is capable of salvaging previously obscured sections of lengthy Holter, 1-Lead, and patch monitor recordings, ensuring accurate analysis even in recordings plagued by high levels of noise and artifacts. Moreover, its continuous learning model ensures that the technology evolves over time, improving both accuracy and efficiency with each use.
By minimizing the time spent on manual tasks, MaxYield™ empowers clinicians to concentrate on high-level decision-making, ultimately enhancing patient care outcomes. Testimonials from leading cardiologists highlight the platform's transformative impact, particularly in revolutionizing Holter monitor data processing and improving clinical workflows.
Understanding Junctional Rhythm: Definition and Importance in EKG
The junctional rhythm EKG represents a heart pattern that arises from the atrioventricular (AV) junction rather than the sinoatrial (SA) node, typically displaying a heart rate between 40 and 60 beats per minute. Recognizing junctional rhythm EKG is vital, as it may signal underlying heart issues such as AV block or other conduction disorders. Accurate identification of the junctional rhythm EKG pattern is crucial for effective clinical management, particularly in light of evolving cardiac health statistics.
For example, the sinoatrial node receives blood supply from the sinoatrial nodal artery in approximately 60% of individuals, while the atrioventricular node is supplied by the atrioventricular nodal branch from the right coronary artery in 90% of cases. This anatomical insight aids in understanding how connection patterns affect overall cardiac function.
Case studies underscore the significance of the heart's electrical conduction system, which comprises specialized pacemaker cells, including the sinoatrial and atrioventricular nodes. These structures are responsible for regulating heart contractions and are essential for identifying and categorizing connection patterns. The sinoatrial node, in particular, plays a critical role in maintaining normal sinus rhythms; its dysfunction can activate secondary pacemaker sites, leading to alternative patterns.
In clinical practice, the ability to recognize specific patterns enhances patient care by enabling healthcare professionals to identify underlying electrophysiological issues. As we move toward 2025, the importance of connection patterns in cardiac health continues to grow, emphasizing the need for precise EKG assessments. This comprehension is further reinforced by a commitment to employing , which enhances diagnostic accuracy and improves patient outcomes.

Types of Junctional Rhythms: Key Variants and Their EKG Characteristics
Junctional rhythm EKG encompasses several types, including junctional escape rhythm, accelerated junctional rhythm, and junctional tachycardia, each with unique characteristics. Understanding the is essential for accurate diagnosis and treatment, as they can present with overlapping features yet differ significantly in clinical implications.
- Junctional Rhythm EKG: This variant typically displays inverted P-waves that may appear before or after the QRS complexes, indicating a heart rate of 40 to 60 bpm. It serves as a backup mechanism when the sinoatrial node fails to initiate impulses effectively. Symptoms may include dizziness and fatigue, highlighting the need for timely identification and management. MaxYield™ can assist in isolating these critical signals even in recordings with significant noise, ensuring accurate diagnosis.
- Accelerated Junctional Rhythm EKG: Defined by a heart rate between 60 and 100 bpm, this pattern frequently maintains analogous P-wave features to the escape pattern. It reflects heightened activity at the junction and may not show significant symptoms. Continuous monitoring is essential to identify potential complications. The adaptability of MaxYield™ enhances the recognition of these patterns, improving clinical decision-making.
- Junctional Tachycardia: This type, seen on a junctional rhythm EKG, is defined by a heart rate exceeding 100 bpm, with P-waves that may be absent or inverted. It can lead to symptoms such as palpitations and may require medical evaluation to determine the underlying cause. The automated labeling features of MaxYield™ streamline the analysis process, reducing the risk of oversight in busy clinical settings.
For healthcare professionals, utilizing MaxYield™ effectively can enhance the accuracy of ECG interpretations and improve patient outcomes. For example, escape beats may suggest a more severe underlying condition if symptomatic, while accelerated escape is often harmless. Prompt recognition and handling of these patterns can avert advancement to more serious arrhythmias, highlighting the significance of comprehensive analysis of junctional rhythm EKG in medical practice. Furthermore, it is significant that one in every 600 Americans over 65 with heart issues experiences problems with their sinus node, highlighting the commonality of specific heart patterns in this demographic.

Common Causes of Junctional Rhythm: Identifying Underlying Factors
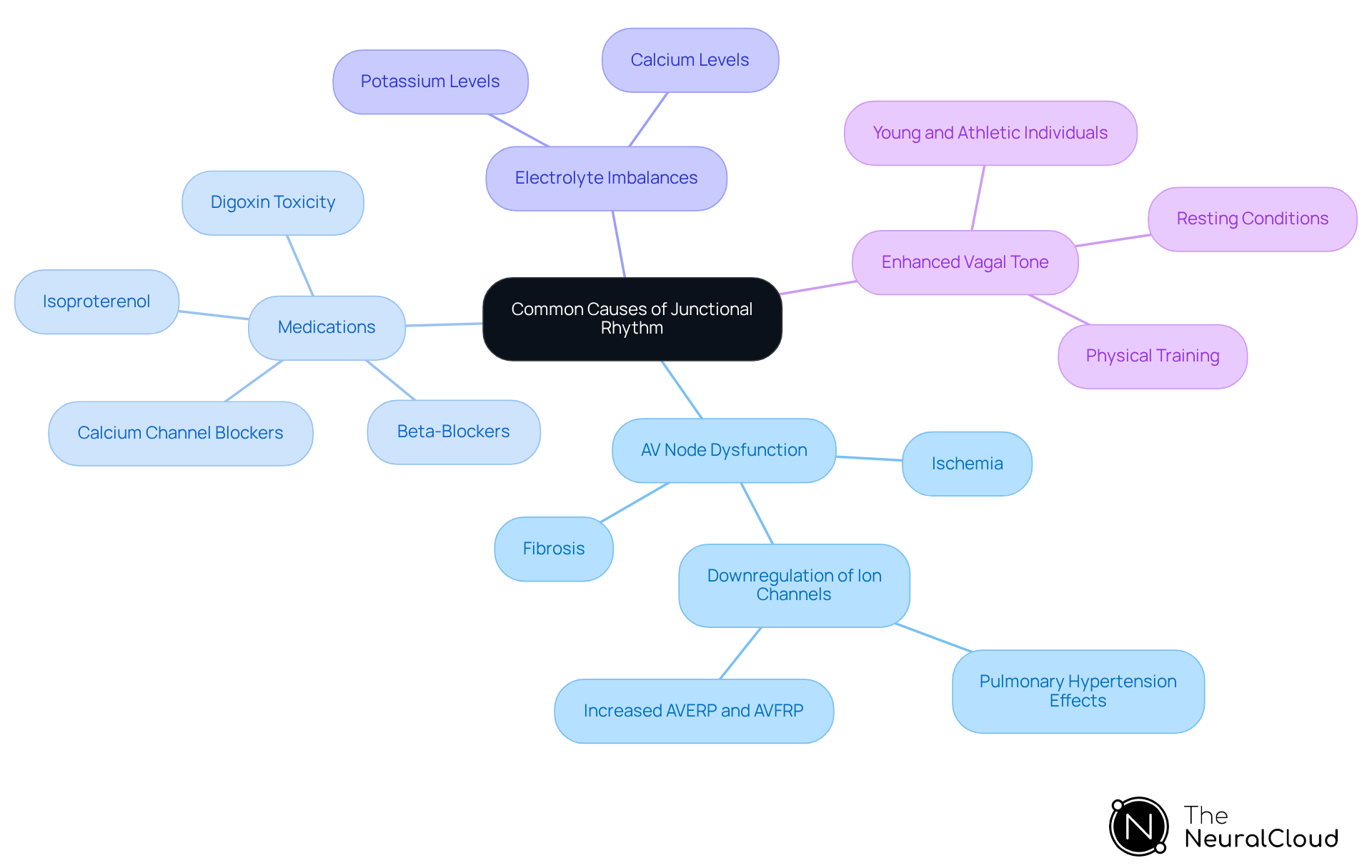
Common causes of junctional rhythm include:
- AV Node Dysfunction: Conditions such as ischemia or fibrosis significantly impair the normal conduction pathway, leading to junctional rhythms. Research indicates that downregulation of ion channels in the AV node, particularly in conditions like pulmonary hypertension, contributes to this dysfunction and results in altered conduction dynamics. Notably, significant increases in AVERP and AVFRP have been observed in PHT rats, highlighting the impact of AV node dysfunction on cardiac conduction.
- Medications: Certain drugs, particularly beta-blockers and calcium channel blockers, are recognized to trigger specific patterns. For instance, nonparoxysmal atrioventricular tachycardia is frequently associated with digoxin toxicity, acute myocardial infarction, or the use of isoproterenol. Most AV conduction patterns resulting from digitalis toxicity exhibit a rate of fewer than 130 beats/min, demonstrating how these medications can increase automaticity within the AV node, enabling it to surpass the sinus node under certain conditions.
- Electrolyte Imbalances: Abnormal levels of potassium or calcium can interfere with cardiac conduction, potentially resulting in irregular heart patterns. Such imbalances are critical to monitor, as they can exacerbate existing cardiac conditions by affecting the normal electrical activity of the heart.
- Enhanced Vagal Tone: Conditions like rest or physical training can boost vagal impact on the heart, leading to specific heart patterns. This phenomenon is especially prevalent in younger and athletic individuals, where instances of heart activity are often harmless and do not necessitate intervention. Understanding the benign characteristics of these patterns, particularly in relation to , in specific demographics is essential for targeted treatment and management strategies.
Symptoms of Junctional Rhythm: Recognizing Clinical Indicators
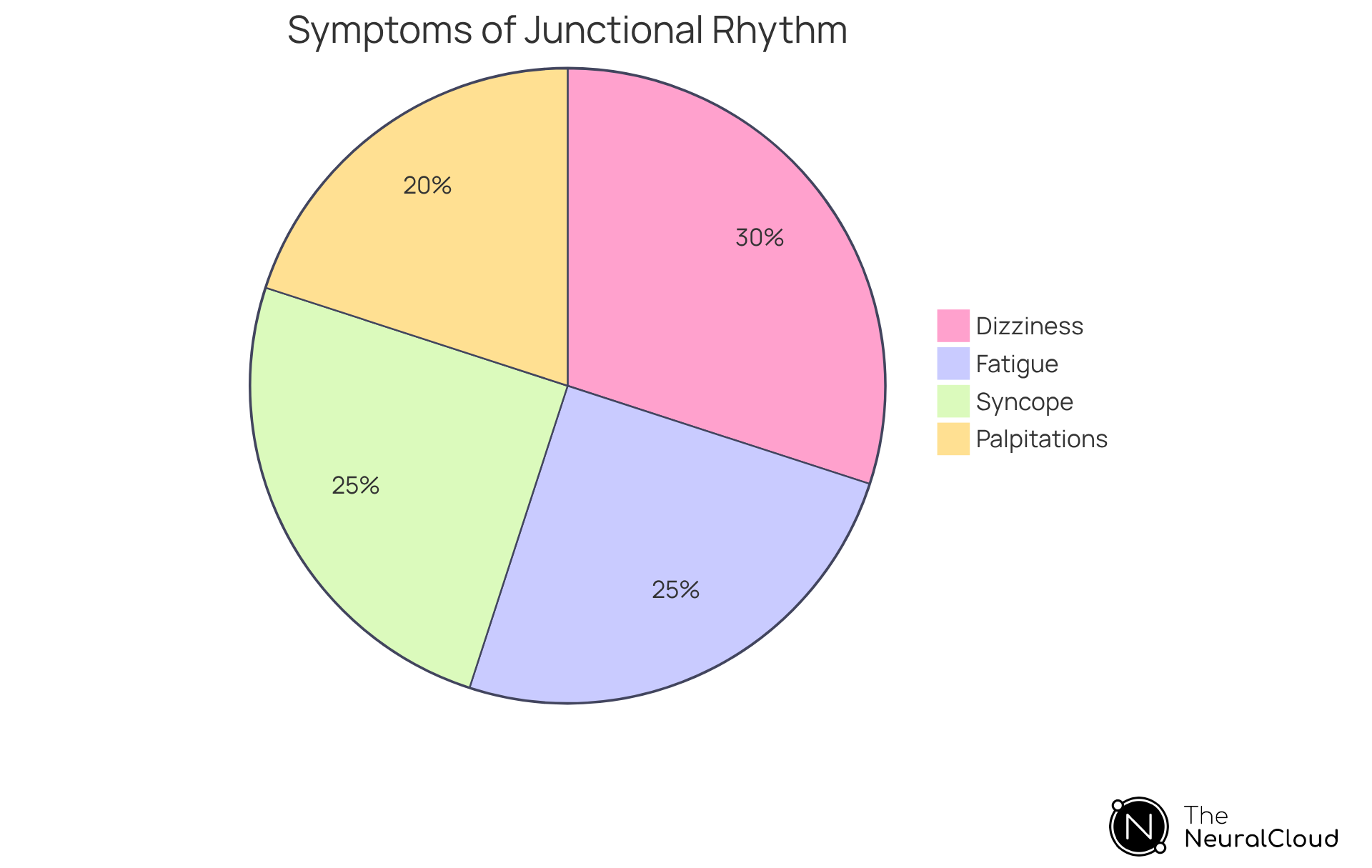
Symptoms of junctional rhythm EKG can manifest in various ways, and recognizing them is crucial for effective management. Key clinical indicators include:
- Dizziness or Lightheadedness: Often resulting from reduced cardiac output, this symptom can indicate the severity of the rhythm disturbance.
- Fatigue: Patients may experience fatigue due to inadequate heart rate, which can significantly impact their daily activities.
- Palpitations: Irregular heartbeats are frequently mentioned, resulting in heightened anxiety and discomfort for individuals.
- Syncope: In severe instances, individuals may experience fainting spells, which can pose risks of injury.
The occurrence of dizziness and syncope among individuals with specific heart patterns highlights the necessity for alertness. Studies indicate that these symptoms are frequently observed, particularly in cases of atrioventricular dissociation, where the heart's electrical signals are disrupted. For example, an observational study discovered that 38% of patients with a specific heart pattern reported a history of fainting, emphasizing the significance of tracking these clinical signs.
With MaxYield™, healthcare professionals can utilize to convert lengthy and noisy ECG recordings into clear, distinct signals, improving the precision of identifying patterns. This technology assists in identifying symptoms quickly, enabling timely intervention and possibly preventing complications related to untreated heart patterns. Comprehending the fundamental reasons for this type of cardiac activity, including acute myocardial infarction and hyperkalemia, is crucial for effective management of individuals exhibiting junctional rhythm EKG, as many of these causes are reversible and do not require permanent pacemaker implantation. This insight strengthens the essential role of healthcare professionals in recognizing and managing related symptoms to enhance patient outcomes, supported by the accuracy and automation provided by MaxYield™.
Diagnostic Tests for Junctional Rhythm: Methods and Procedures
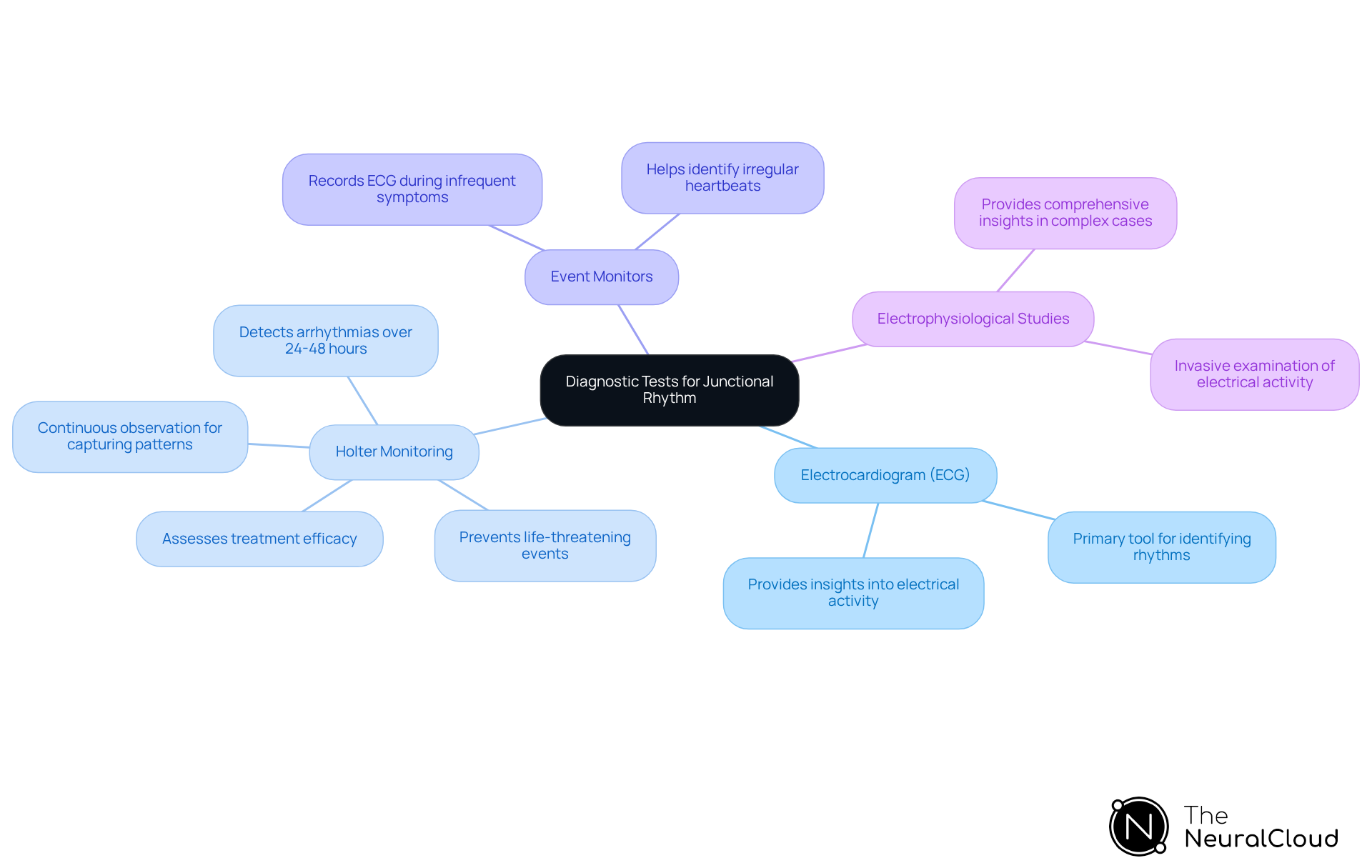
Diagnostic tests for junctional rhythm encompass several key methods:
- Electrocardiogram (ECG): This remains the primary tool for identifying junctional rhythms, providing essential insights into the heart's electrical activity.
- Holter Monitoring: Continuous ECG observation over 24 to 48 hours is essential for capturing temporary patterns that may not be apparent during standard ECG tests. Holter monitors are especially efficient in detecting arrhythmias by recording every heartbeat, assisting in recognizing irregularities that could suggest underlying conditions.
- Event Monitors: These devices are utilized for patients experiencing infrequent symptoms, allowing them to record their ECG during episodes. This focused method assists in when symptoms occur infrequently.
- Electrophysiological Studies: Invasive examinations that evaluate the heart's electrical activity offer comprehensive insights into connection patterns, especially in intricate situations where non-invasive techniques may not produce definitive outcomes.
The use of Holter monitoring has demonstrated considerable efficacy in identifying abnormal patterns, including junctional rhythm EKG. Research suggests that prolonged monitoring durations can improve detection rates of previously unrecognized arrhythmias. For instance, a recent study highlighted that Holter monitoring can prevent potentially life-threatening events, such as strokes or heart attacks, by enabling early detection of arrhythmias. Healthcare experts emphasize the significance of these diagnostic instruments, noting that Holter monitoring not only records temporary patterns but also assists in evaluating the effectiveness of therapies for individuals already identified with arrhythmias. Practical uses of Holter monitoring have shown its ability to detect abnormal heart patterns efficiently, establishing it as an essential instrument in modern cardiac care.
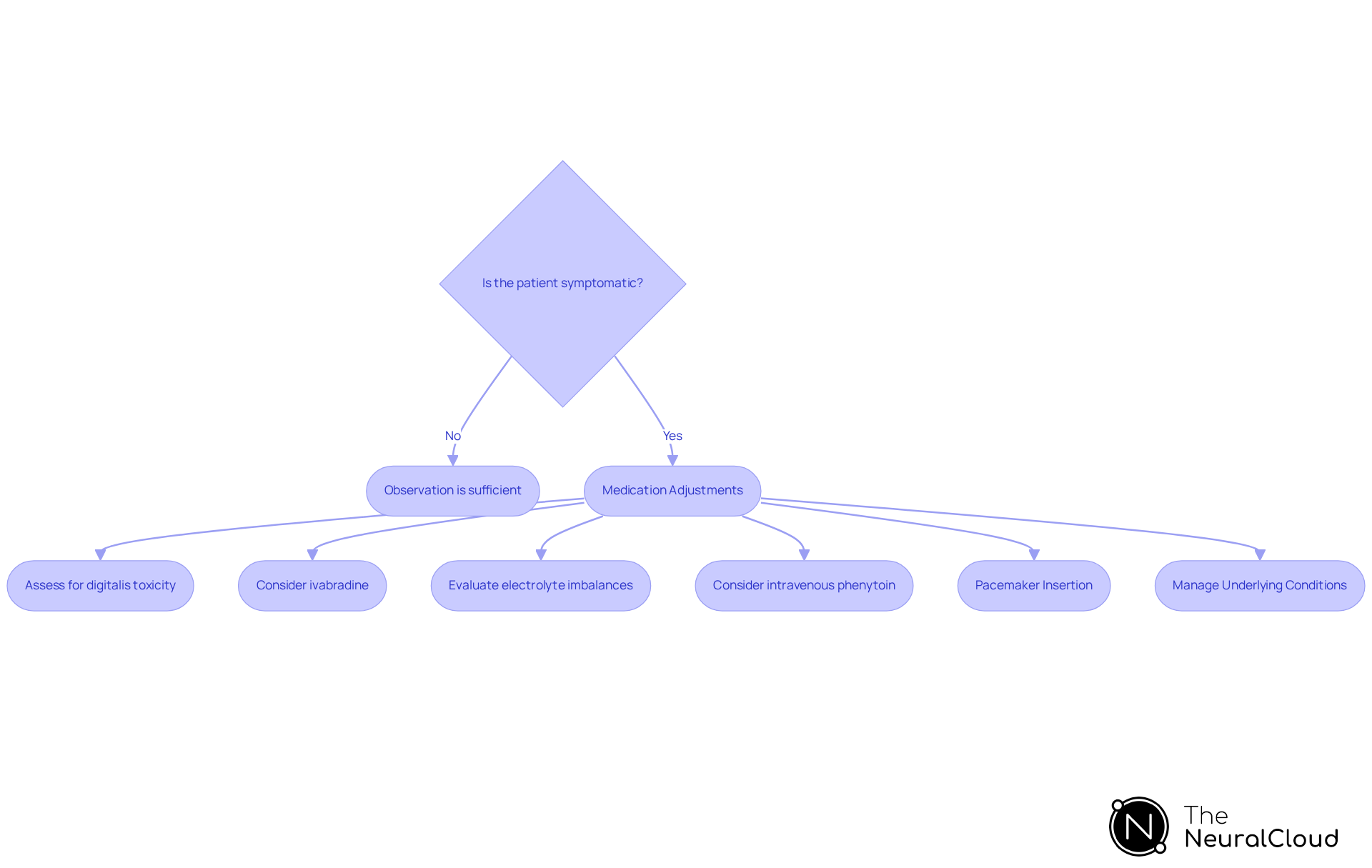
Treatment Options for Junctional Rhythm: Approaches and Considerations
Treatment options for consist of various strategies tailored to patient needs and underlying causes.
Observation is often sufficient for asymptomatic patients, as junctional rhythm EKGs can frequently be well tolerated without intervention. Case studies indicate that asymptomatic individuals typically do not require pharmacologic therapy, suggesting that treatment should be customized based on symptoms and underlying causes.
Medication adjustments are critical; it is essential to assess and modify medications that may exacerbate the junctional rhythm EKG. This is particularly relevant in cases of digitalis toxicity, where treatments like atropine or digoxin immune Fab may be necessary. Additionally, ivabradine could serve as a beneficial supplementary therapy for ectopic tachycardia, warranting consideration in treatment strategies.
In instances of symptomatic bradycardia, pacemaker insertion is a vital intervention. This approach is especially significant for individuals with complete or high-grade AV block, where a permanent pacemaker may be required to maintain adequate heart rates. Recent trends indicate an increasing reliance on pacemakers for regulating heart patterns, particularly among high-risk groups. As highlighted by Sean C Beinart, MD, patients with significant comorbidities may struggle to manage secondary heart patterns effectively and may require procedures such as pacemaker insertion.
Managing underlying conditions is essential for effective treatment. Addressing contributing factors such as electrolyte imbalances or ischemia is crucial. For example, intravenous phenytoin may be employed in resistant cases of symptomatic digitalis toxicity that result in abnormal heart rhythms.
Current practices underscore the significance of individualized treatment plans, with consultations from cardiologists or electrophysiologists recommended for symptomatic cases. Emergency care protocols for this cardiac condition include evaluating 12-lead ECG findings, ensuring airway protection, oxygenation, and blood pressure support. This approach guarantees that immediate care is tailored to the underlying cause of the arrhythmia.
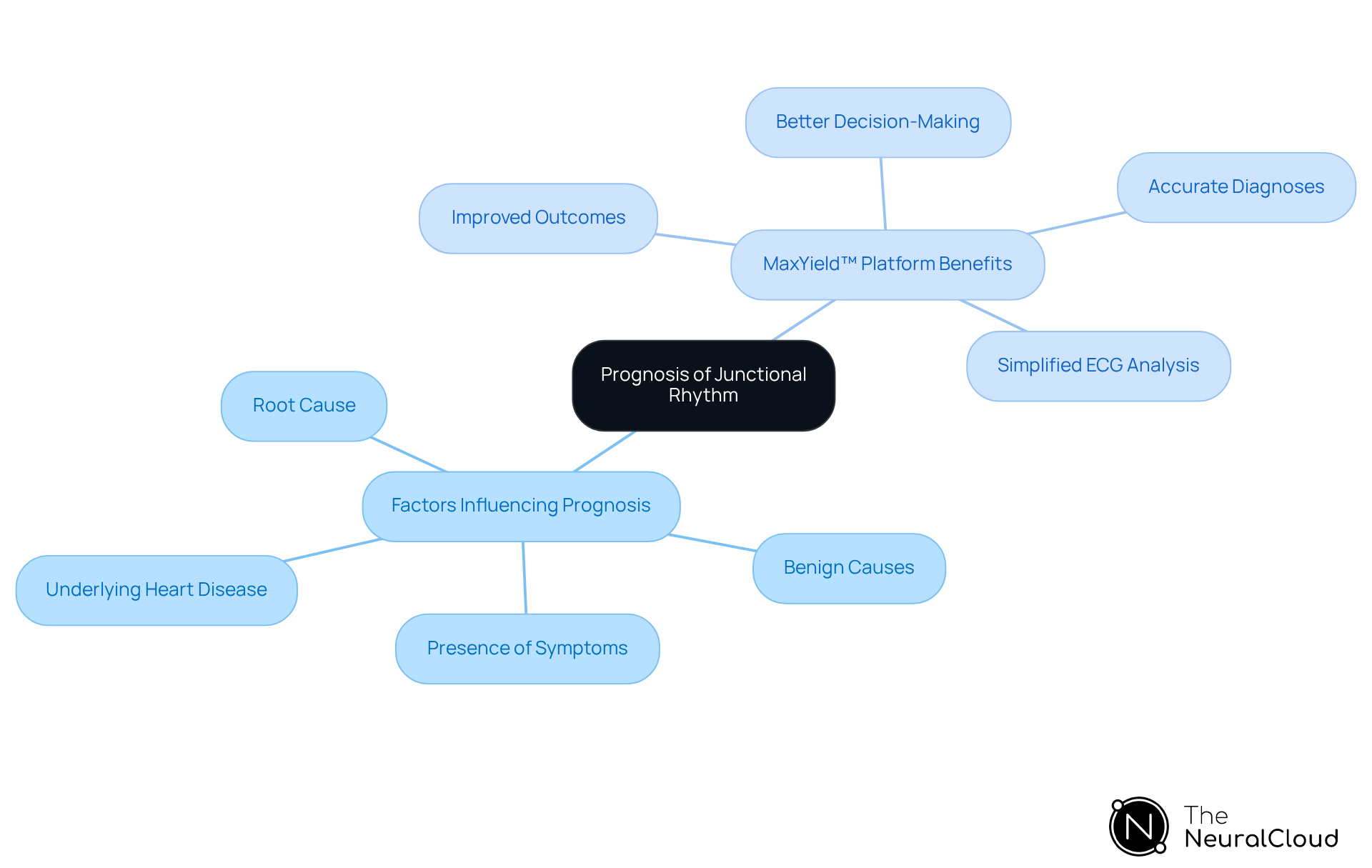
Prognosis of Junctional Rhythm: Understanding Patient Outcomes
The outlook of the heart's electrical pattern primarily depends on the root cause and the presence of symptoms. In many cases, if the pattern is asymptomatic and arises from benign causes, the outlook is favorable. Conversely, if a specific heart pattern is associated with significant underlying heart disease, the prognosis may warrant a more cautious approach.
The MaxYield™ platform from Neural Cloud Solutions addresses these challenges by significantly enhancing early identification and management of contributing factors. This platform features , which improve the accuracy of ECG analysis, even in recordings that exhibit high levels of noise and artifact. By automating the labeling process, MaxYield™ provides clearer ECG signals, enabling health tech developers to effectively tackle the issues of physiological variability and signal artifacts.
The advantages of using the MaxYield™ platform are substantial. Healthcare professionals can expect improved outcomes for individuals, as the platform facilitates better decision-making and more accurate diagnoses. By integrating this technology, the complexities of ECG analysis are simplified, allowing for a more efficient workflow and enhanced patient care.
Monitoring Junctional Rhythm: The Role of Continuous ECG Analysis
Ongoing ECG assessment is crucial for observing junctional rhythm EKG patterns, as it provides real-time insights into heart activity. and remote monitoring systems empower healthcare professionals to track individuals' patterns beyond clinical settings. This proactive approach not only aids in the early detection of rhythm changes but also facilitates prompt interventions, significantly enhancing safety for individuals.
In 2025, advancements in wearable technology have resulted in devices that offer improved accuracy and comfort, making them more accessible to users. For instance, studies show that 14-day patch-type ECG monitoring can identify arrhythmias more effectively than traditional 24-hour Holter monitors, highlighting the potential of wearables in cardiac care.
Healthcare professionals emphasize that these devices can transform user engagement, enabling continuous monitoring that supports better health management. As the landscape of cardiac monitoring evolves, the integration of wearables is becoming standard practice, reflecting a shift towards more patient-centered care.

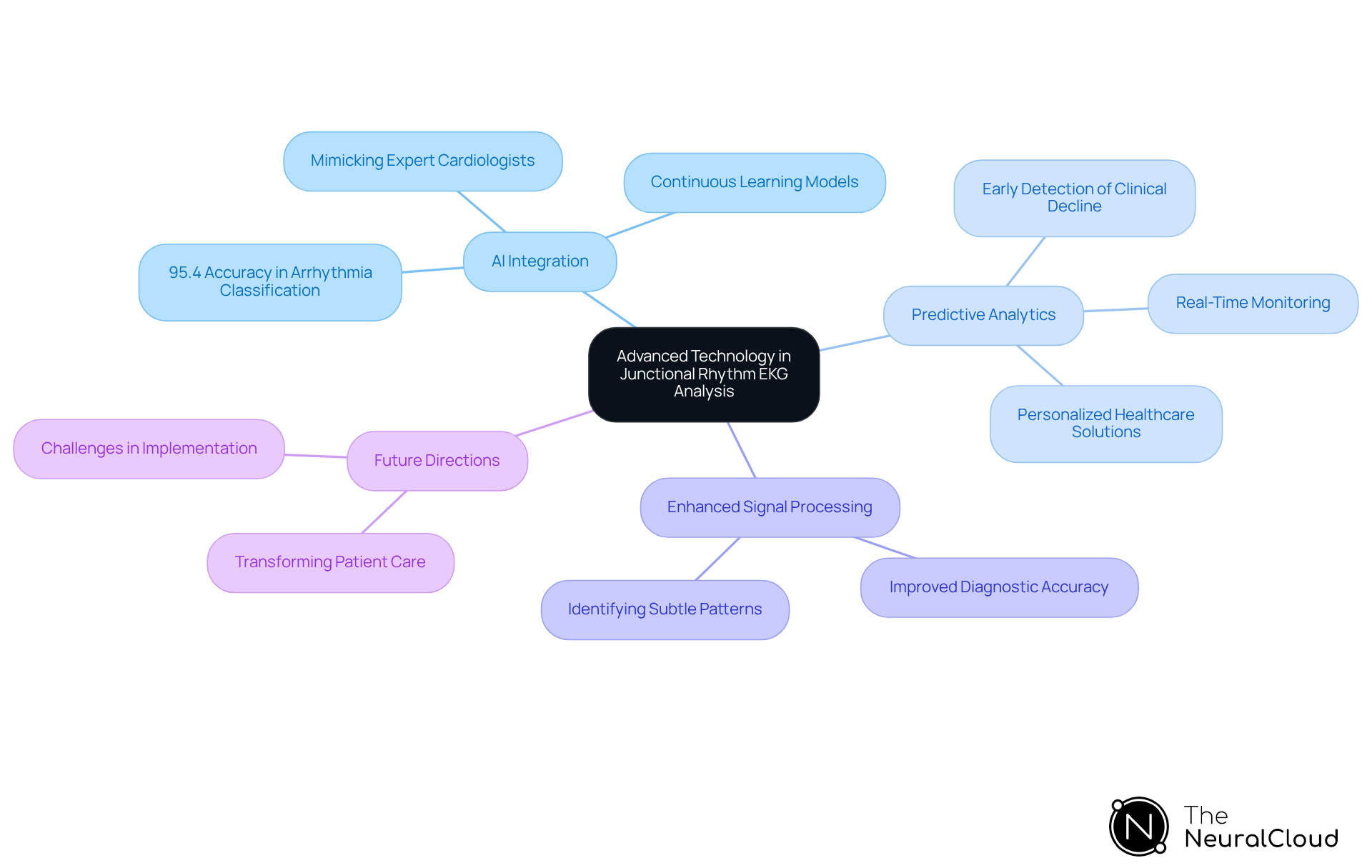
Advanced Technology in Junctional Rhythm Analysis: Innovations and Future Directions
The future of junctional rhythm EKG analysis is poised for significant advancements through the integration of AI and machine learning. Innovations such as predictive analytics and enhanced signal processing are expected to transform the automated interpretation of EKGs, thereby improving diagnostic accuracy and efficiency.
For example, AI models have achieved an impressive 95.4% accuracy in classifying arrhythmias, highlighting their potential to enhance clinical decision-making. As the field evolves, continuous learning models, like those utilized by Neural Cloud Solutions, will be crucial in refining ECG analysis and enabling healthcare providers to deliver superior patient care.
Industry thought leaders emphasize that AI's capacity to mimic expert cardiologists and detect subtle abnormalities will further elevate the standards of ECG diagnostics. Looking ahead to 2025, the ongoing evolution of is set to enhance predictive capabilities, ultimately leading to more personalized and effective healthcare solutions.
Conclusion
The exploration of junctional rhythm EKG has unveiled critical insights that underscore its significance in cardiac health. Understanding the unique characteristics of junctional rhythms, their causes, and the implications for patient care highlights the importance of accurate EKG analysis. Technologies like Neural Cloud Solutions' MaxYield™ platform are revolutionizing the way healthcare professionals interpret these rhythms, ensuring timely and precise diagnostics.
The challenges in EKG analysis often stem from the complexity of identifying junctional rhythms. MaxYield™ addresses these challenges through advanced automation, allowing for rapid analysis of large data volumes and effective noise filtering. These features enhance the accuracy of EKG interpretations, directly benefiting healthcare professionals by streamlining their diagnostic processes. Moreover, recognizing the symptoms and underlying causes of junctional rhythm is essential for effective management and improved patient outcomes.
As the field of cardiac care advances, the integration of innovative technologies and continuous monitoring systems will play a pivotal role in enhancing patient safety and care quality. The future of junctional rhythm EKG analysis lies in harnessing these advancements to facilitate personalized healthcare solutions. Embracing these innovations not only enhances clinical workflows but also empowers healthcare professionals to deliver superior care, ultimately transforming the landscape of cardiac diagnostics and treatment.
Frequently Asked Questions
What is MaxYield™ and how does it enhance EKG analysis?
MaxYield™ is a platform developed by Neural Cloud Solutions that automates the identification and labeling of essential features within ECG signals. It can analyze over 200,000 heartbeats in under five minutes, enhancing the clarity of ECG signals and improving diagnostic reliability through sophisticated AI algorithms and advanced noise filtering capabilities.
What types of recordings can MaxYield™ analyze?
MaxYield™ can analyze lengthy Holter recordings, 1-Lead, and patch monitor recordings, effectively salvaging previously obscured sections even in recordings with high levels of noise and artifacts.
Why is recognizing junctional rhythm EKG important?
Recognizing junctional rhythm EKG is vital as it may indicate underlying heart issues such as AV block or other conduction disorders. Accurate identification is crucial for effective clinical management and improving patient care.
What are the key characteristics of junctional rhythm EKG?
Junctional rhythm EKG typically displays inverted P-waves that may appear before or after the QRS complexes, with a heart rate between 40 and 60 beats per minute. It serves as a backup mechanism when the sinoatrial node fails to initiate impulses effectively.
What differentiates accelerated junctional rhythm from junctional rhythm?
Accelerated junctional rhythm is characterized by a heart rate between 60 and 100 bpm, maintaining similar P-wave features to the escape pattern. It indicates heightened activity at the junction and may not present significant symptoms.
What is junctional tachycardia and its implications?
Junctional tachycardia is defined by a heart rate exceeding 100 bpm, with P-waves that may be absent or inverted. It can lead to symptoms such as palpitations and may require medical evaluation to determine the underlying cause.
How does MaxYield™ assist in clinical decision-making?
MaxYield™ enhances the accuracy of ECG interpretations by isolating critical signals, streamlining the analysis process, and reducing the risk of oversight in busy clinical settings, ultimately improving patient outcomes.
What is the significance of the heart's electrical conduction system in EKG analysis?
The heart's electrical conduction system, including the sinoatrial and atrioventricular nodes, regulates heart contractions and is essential for identifying and categorizing connection patterns, which are crucial for effective clinical management.


