Overview
The article presents ten key insights into second degree type 2 heart block, highlighting its serious implications and the critical need for timely diagnosis and management. It details the defining characteristics of the condition and potential complications. Furthermore, it underscores the significance of advanced ECG analysis technologies, such as Neural Cloud Solutions' MaxYield™, in enhancing diagnostic accuracy and improving patient outcomes.
Introduction
Understanding the complexities of second degree type 2 heart block is crucial, as this condition can have serious implications for cardiovascular health. The challenges in ECG analysis are significant, demanding advanced solutions to enhance accuracy. With advancements in technology, particularly through platforms like Neural Cloud Solutions' MaxYield™, healthcare professionals are equipped with powerful tools that improve the accuracy of ECG analysis. This leads to better patient outcomes, addressing a critical need in cardiovascular care.
However, the challenge remains: how can one effectively differentiate this condition from other heart blocks, and what proactive measures can be taken to mitigate its risks?
This article delves into ten key insights that illuminate the significance, symptoms, and management strategies for second degree type 2 heart block, offering a comprehensive guide for both patients and practitioners.
Neural Cloud Solutions' MaxYield™: Advanced ECG Analysis for Heart Block Detection
Neural Cloud Solutions' MaxYield™ platform is at the forefront of revolutionizing ECG analysis, particularly in the automated identification of cardiac interruptions, including the second degree type 2 heart block. This platform leverages to process over 200,000 heartbeats in under five minutes, providing rapid and precise insights that empower healthcare professionals. By isolating critical ECG features such as P-waves, QRS complexes, and T-waves, MaxYield™ enhances the clarity of ECG signals, aiding in the detection of irregularities linked to cardiac obstruction.
The integration of AI algorithms not only streamlines the analysis process but also boosts diagnostic accuracy. A recent study revealed that AI-driven models achieved an impressive accuracy of 93.6% in predicting cardiac illnesses, underscoring the potential of these technologies in clinical settings. Cardiologists have commended the automated ECG analysis technology for its capacity to reduce manual workload and improve clinical workflows, enabling them to concentrate on high-level decision-making rather than time-consuming tasks.
Case studies further demonstrate the effectiveness of the MaxYield™ platform. In one instance, a 65-year-old male patient with complete atrioventricular obstruction experienced notable clinical improvements following the implementation of a dual-chamber pacemaker, guided by insights derived from MaxYield™ analysis. This case highlights the platform's role in not only identifying cardiac issues but also in informing treatment decisions that lead to better patient outcomes.
As AI continues to reshape ECG analysis in cardiology, the MaxYield™ platform emerges as an essential tool for healthcare professionals aiming to enhance diagnostic accuracy and improve patient care.

Understanding Second Degree Type 2 Heart Block: Definition and Importance
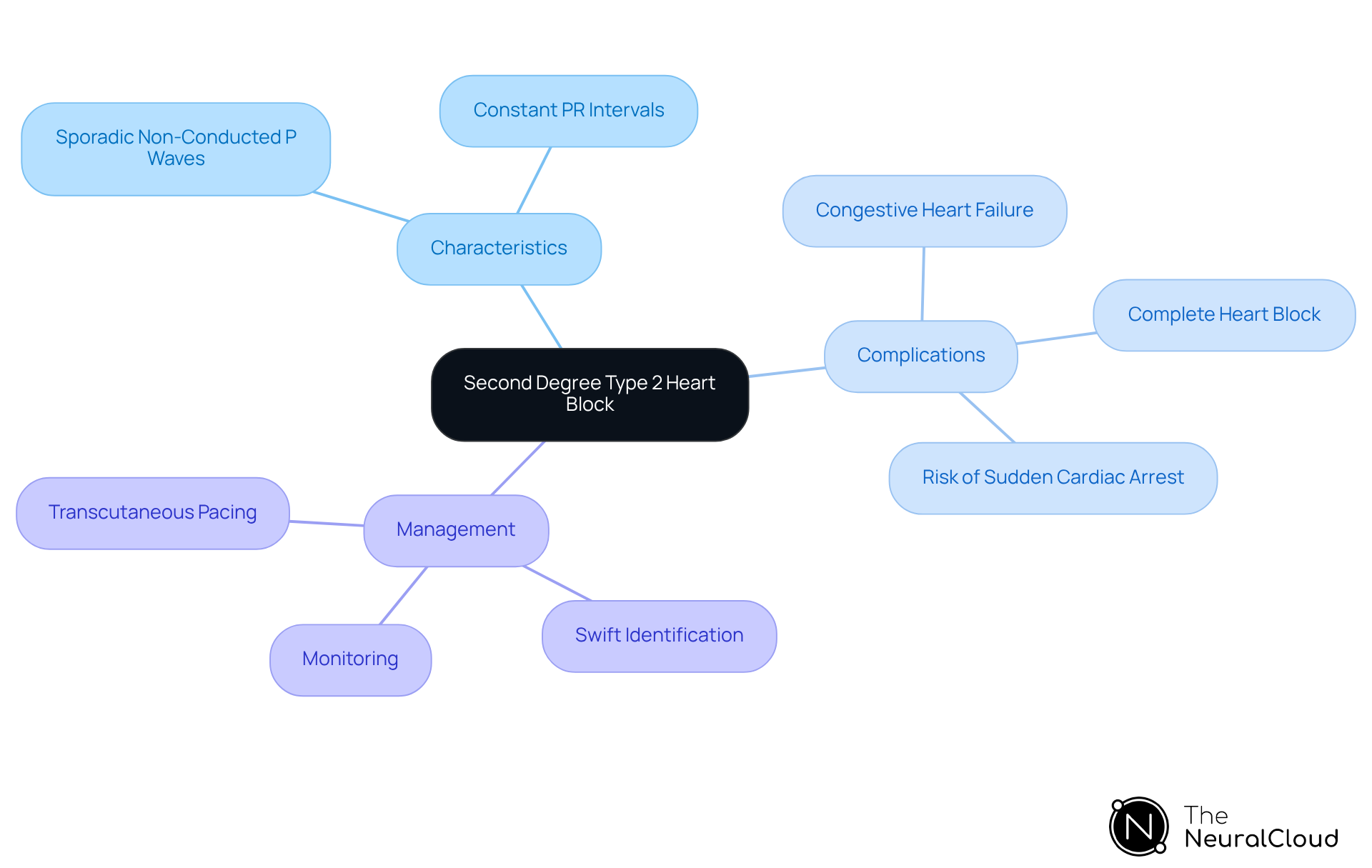
The condition known as [second degree type 2 heart block](https://pmc.ncbi.nlm.nih.gov/articles/PMC11390567), often referred to as Mobitz type II, is characterized by sporadic non-conducted P waves that appear without gradual lengthening of the PR interval. This condition signifies a serious conduction disturbance within the heart's electrical system, specifically identified as second degree type 2 heart block, which can lead to severe complications, including:
- Complete heart block
- Congestive heart failure
- An increased risk of sudden cardiac arrest
Statistics suggest that second degree type 2 heart block can lead to considerable negative consequences, such as syncope and bradycardia, requiring swift identification and action. Cardiologists stress that comprehending second degree type 2 heart block is crucial for effective management, as failure to recognize this condition can result in life-threatening situations.
The consequences of second degree type 2 heart block, also known as Mobitz variant II, reach beyond immediate symptoms; untreated instances may advance to more severe heart conduction issues, emphasizing the necessity for careful monitoring and suitable treatment approaches. Additionally, it is crucial to highlight that second degree type 2 heart block, which corresponds to Mobitz classification II AVB, is linked with bundle branch obstruction in roughly 70-80% of instances.
The integration of wearable technology with Neural Cloud Solutions' MaxYield™ platform can significantly enhance the efficiency of ECG analysis by automating the labeling process and addressing challenges such as physiological variability and signal artifacts.
MaxYield™'s advanced noise filtering capabilities allow for the rapid isolation of ECG waves, even in recordings affected by baseline wander and muscle artifact. This ensures that critical data is salvaged, enabling healthcare professionals to make informed decisions swiftly. Transcutaneous pacing should be applied to all patients with second degree type 2 heart block, even if asymptomatic, to .
Recognizing Symptoms of Second Degree Type 2 Heart Block
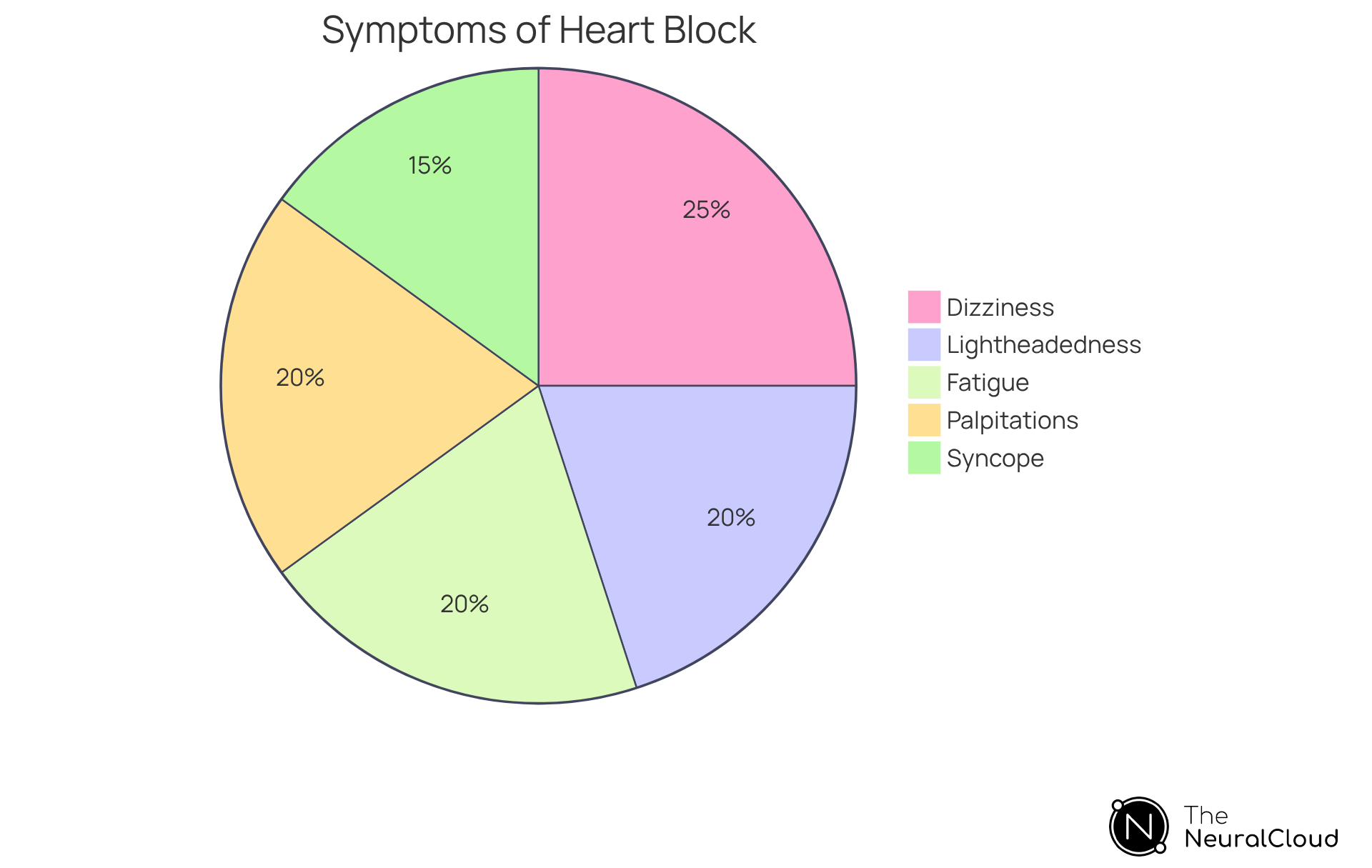
Identifying the signs of second-degree category 2 cardiac interruption is crucial for prompt action. Common symptoms of second degree type 2 heart block include:
- Dizziness
- Lightheadedness
- Fatigue
- Syncope
- Palpitations or a sensation of skipped heartbeats
These symptoms may indicate a worsening condition that requires immediate medical attention. The MaxYield™ platform significantly enhances the recognition and analysis of these symptoms through advanced ECG interpretation. Healthcare specialists are encouraged to utilize ECG analysis tools to efficiently track these symptoms, as prompt diagnosis and treatment can avert serious complications, including cardiac failure. Understanding the relationship between these symptoms and is essential for improving patient outcomes.
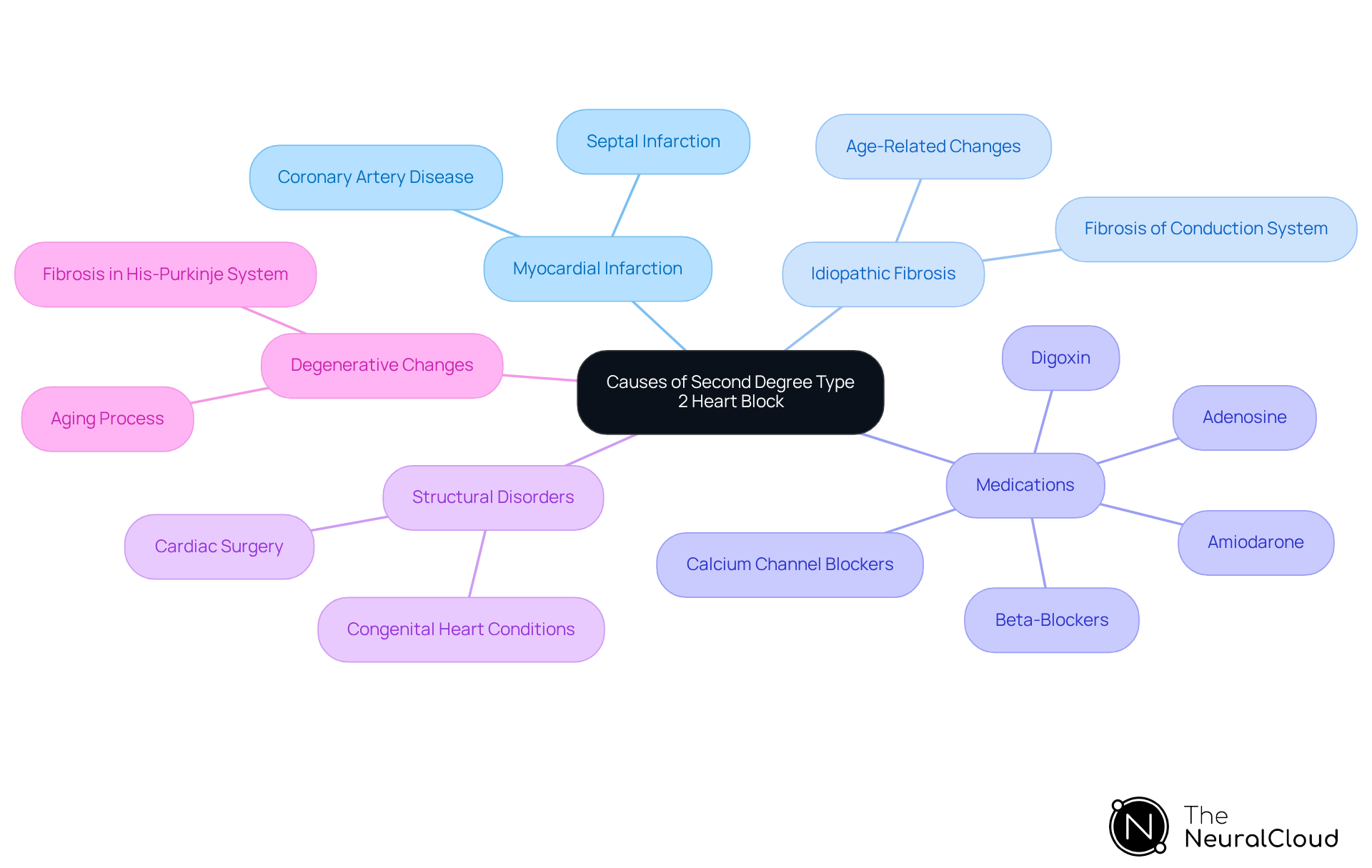
Identifying Causes of Second Degree Type 2 Heart Block
Second-degree type 2 heart block can arise from various causes, including:
Identifying these causes is essential for effective management and treatment planning, as it directly impacts patient outcomes.
Diagnostic Approaches for Second Degree Type 2 Heart Block
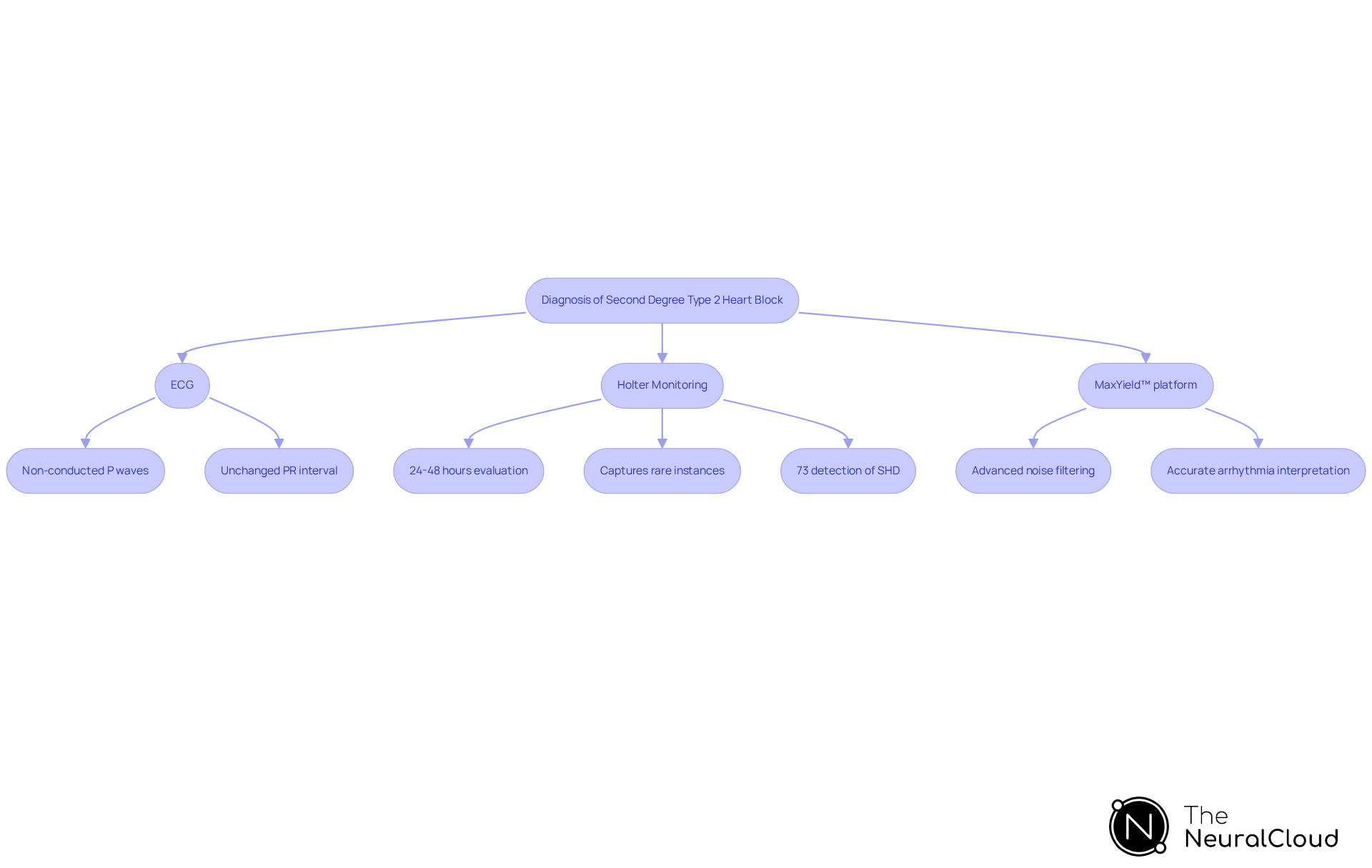
The electrocardiogram (ECG) serves as the primary diagnostic tool for identifying second degree type 2 heart block, which is characterized by the distinctive pattern of non-conducted P waves. This condition necessitates careful interpretation, as the diagnosis relies on recognizing the unchanged PR interval before and after the blocked impulse.
Holter monitoring is crucial in this context, allowing for continuous evaluation of rhythms over 24 to 48 hours. This method is particularly effective in capturing rare instances of obstruction that may not be visible during . In a study involving 150 patients, Holter monitoring demonstrated its effectiveness in detecting arrhythmias, with significant findings revealing that 73% of high-risk participants had previously unrecognized structural cardiovascular disease (SHD).
Experts emphasize that incorporating various Holter ECG parameters can significantly enhance the diagnostic evaluation of heart conditions, ultimately improving patient outcomes and management strategies. Additionally, the MaxYield™ platform has the capability to transform noisy Holter recordings into comprehensive insights, quickly isolating ECG waves even amidst baseline wander and muscle artifacts. This advanced noise filtering feature ensures that critical data remains unobscured, facilitating more accurate interpretation of arrhythmias.
It is vital to acknowledge that the second degree type 2 heart block, which is a Mobitz form II AV conduction abnormality, can escalate into more severe levels of AV disruption, necessitating prompt intervention to prevent serious complications. Moreover, a stable sinus rate is essential for diagnosing Mobitz variant II AVB, underscoring the importance of precise interpretation in clinical practice.
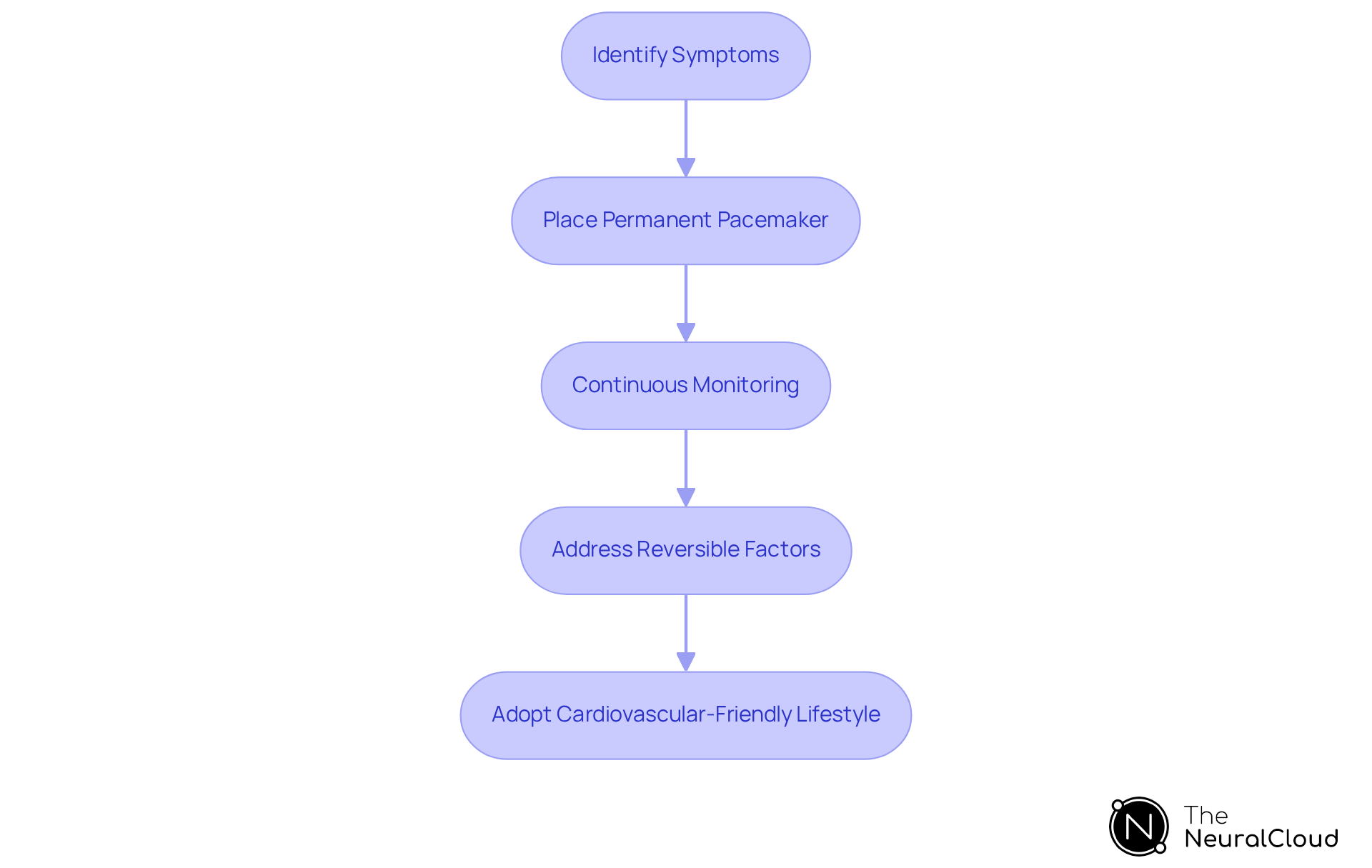
Treatment Strategies for Second Degree Type 2 Heart Block
Management of second degree type 2 heart block primarily involves the placement of a permanent pacemaker, particularly for individuals exhibiting symptoms. This device is crucial for maintaining a steady pulse and mitigating , such as dizziness and fainting.
In some cases, it may be essential to address reversible factors, including adjustments to medications, to optimize patient health. Continuous monitoring and follow-up care are vital to ensure favorable outcomes, as they enable healthcare providers to evaluate the pacemaker's effectiveness and implement necessary adjustments.
Recent advancements in pacemaker technology, including improved battery life and enhanced integration with remote health monitoring systems, have significantly elevated their functionality and overall management of cardiac conditions.
Cardiologists emphasize that timely intervention with pacemakers can greatly enhance patients' quality of life, reducing the risk of severe complications related to untreated cardiac issues, such as the potential progression to third-degree blockage or cardiac arrest.
Furthermore, adopting a cardiovascular-friendly lifestyle, which includes regular physical activity and a balanced diet, is essential for patients with cardiac obstruction to improve their overall well-being.
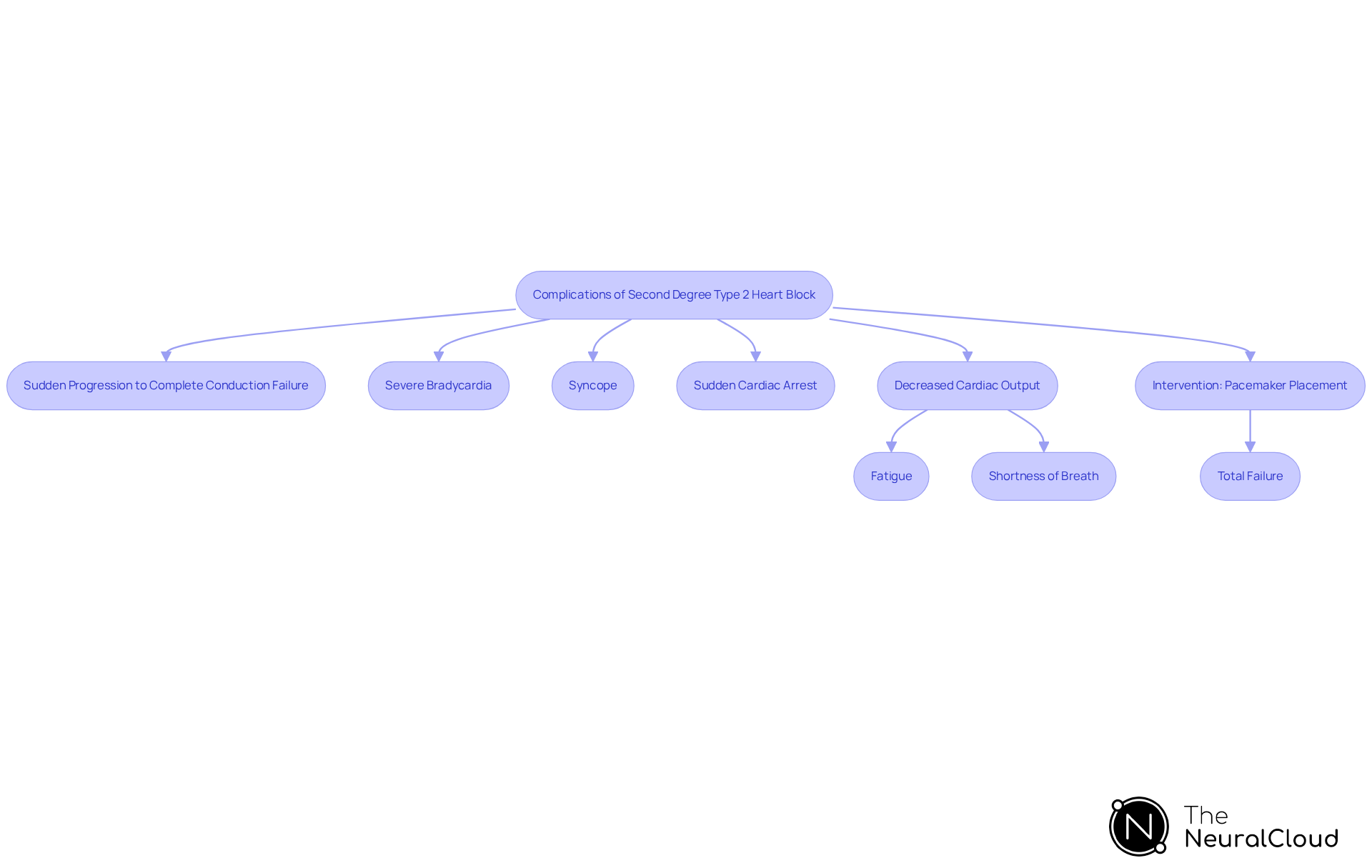
Complications of Second Degree Type 2 Heart Block
Complications arising from second degree type 2 heart block pose significant risks, including the potential for sudden progression to complete conduction failure. This can lead to severe bradycardia, syncope, and even sudden cardiac arrest. Patients may experience a decrease in cardiac output, which can manifest as fatigue and shortness of breath. Without appropriate interventions, such as the , the likelihood of advancing to total failure remains considerable.
Research indicates that second degree type 2 heart block can result in total failure in a notable number of cases. Awareness of these complications is essential for healthcare providers, as timely interventions can prevent serious outcomes. Healthcare professionals must remain vigilant in observing patients for signs and managing potential risks associated with cardiac obstruction.
Differentiating Second Degree Type 2 Heart Block from Other Heart Blocks
Distinguishing second degree type 2 heart block from other forms, such as Mobitz variant I, is crucial for effective management. Mobitz form I is characterized by a progressive prolongation of the PR interval until a dropped beat occurs, whereas Mobitz form II maintains a constant PR interval until a P wave is not followed by a QRS complex. This differentiation is vital, as Mobitz II is frequently linked to an increased risk of progression to total conduction failure and may necessitate prompt action, such as pacemaker placement.
Recent studies indicate that misdiagnosis rates of heart block categories in clinical practice can be significant, underscoring the necessity for accurate ECG interpretation. For instance, Mobitz classification I typically presents with symptoms like lightheadedness or syncope, yet it is often asymptomatic and may not require treatment. In contrast, the second degree type 2 heart block classification can lead to severe complications, including decreased cardiac output and sudden cardiac arrest, making timely diagnosis and management imperative.
Cardiologists emphasize the significance of PR interval patterns in determining the appropriate course of action. As one specialist noted, "The outlook for Mobitz classification II fluctuates depending on the root cause and may necessitate pacemaker insertion to prevent complications." Understanding these characteristics not only aids in but also enhances patient outcomes by ensuring that those at risk receive the necessary interventions promptly. Ongoing studies continue to explore the intricacies of these cardiac interruptions, highlighting the importance of continuous education and awareness within the medical field.

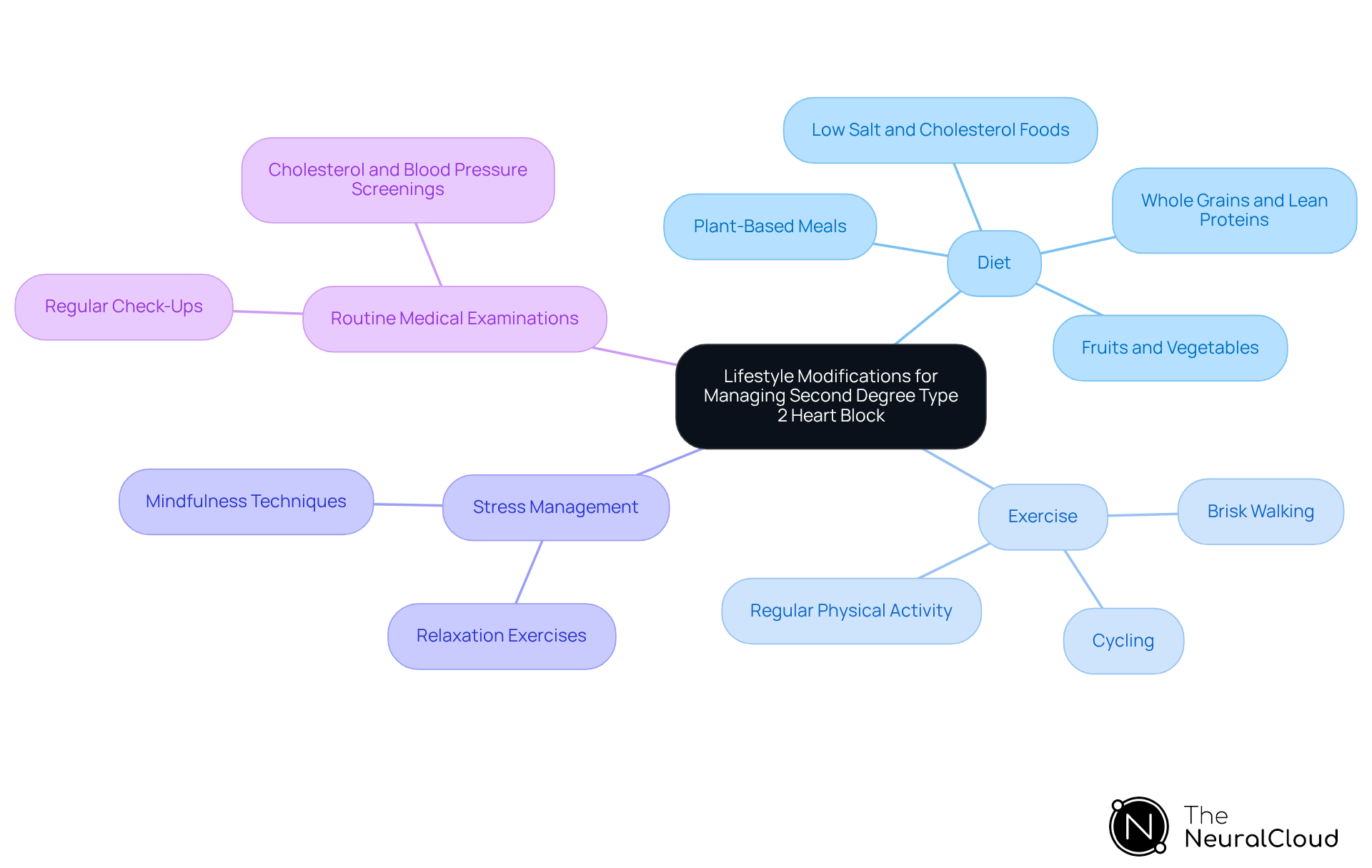
Lifestyle Modifications for Managing Second Degree Type 2 Heart Block
Individuals with second degree type 2 heart block can significantly enhance their cardiovascular well-being through lifestyle changes. Adopting a heart-healthy diet, which is rich in fruits, vegetables, whole grains, and lean proteins, is essential. Research indicates that a and improve overall health outcomes. Notably, studies suggest that 90 percent of nearly 18 million cardiovascular disease cases worldwide could be prevented by embracing a healthier diet, engaging in regular exercise, and avoiding smoking. Regular physical activity is equally vital; individuals who maintain consistent exercise routines can reduce their risk of cardiovascular complications. Additionally, steering clear of tobacco and minimizing alcohol consumption are crucial steps in safeguarding cardiovascular health.
Stress management techniques, including mindfulness and relaxation exercises, can further bolster cardiovascular function. As highlighted in the case study on mental health and cardiovascular conditions, promoting mental well-being is key to sustaining cardiovascular health and preventing disease progression. Routine medical examinations are essential for evaluating cardiovascular wellness and making necessary adjustments to treatment strategies. These lifestyle modifications not only enhance overall cardiovascular function but also play a significant role in mitigating the risk of complications associated with second degree type 2 heart block. Dr. Leslie Cho emphasizes, "Cardiovascular disease is 90 percent manageable - anyone can avoid cardiovascular issues anywhere globally, particularly by consuming foods that are low in salt and cholesterol, exercising consistently, and refraining from smoking."
Integrating diet and exercise into daily routines presents a powerful strategy for improving cardiovascular health and preventing disease progression. To implement these insights, consider incorporating more plant-based meals into your diet and establishing a regular exercise routine, such as brisk walking or cycling, to support your cardiovascular health.
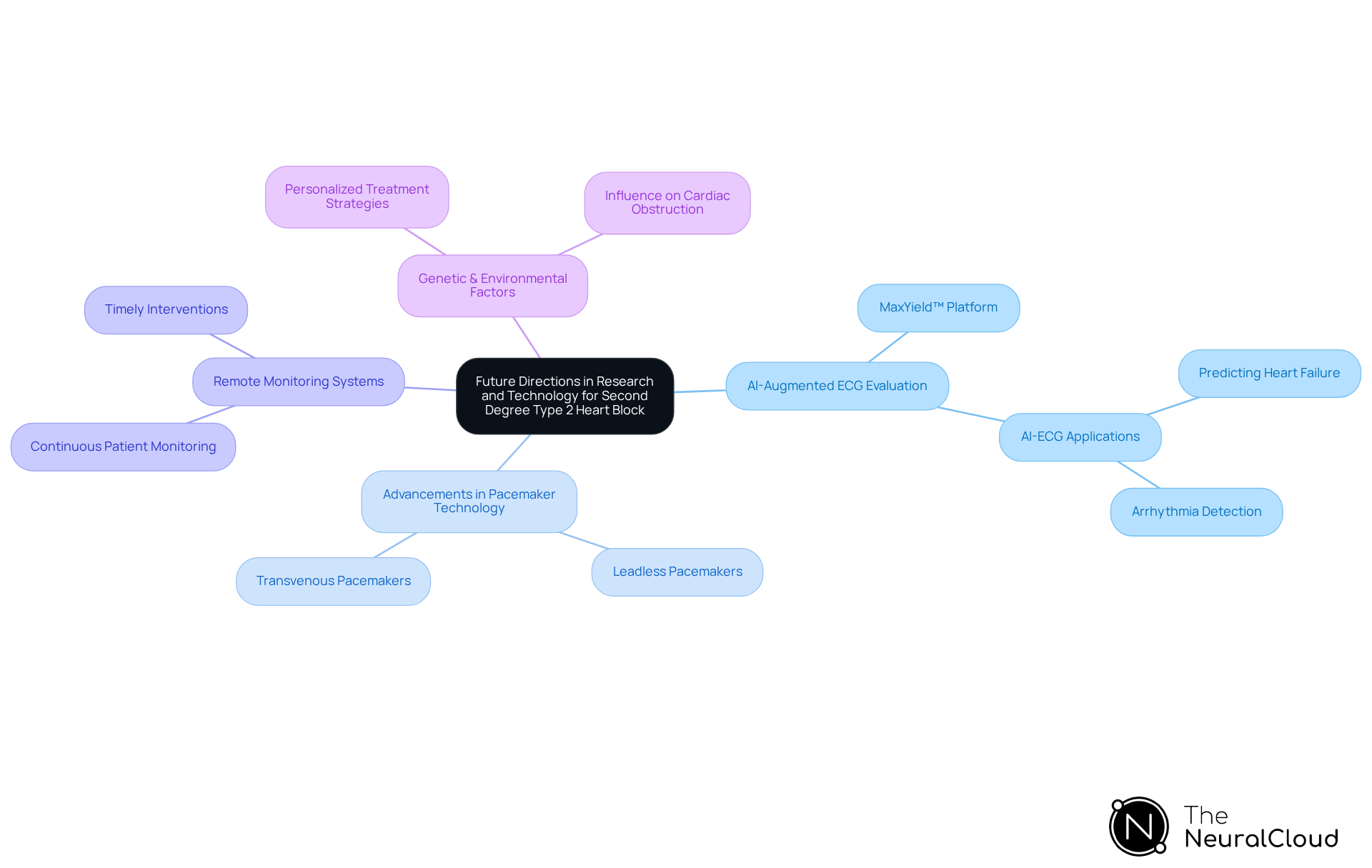
Future Directions in Research and Technology for Second Degree Type 2 Heart Block
Future studies on second degree type 2 heart block are poised to leverage AI-augmented ECG evaluation through Neural Cloud Solutions' MaxYield™ platform, which has shown significant promise in delivering more accurate and timely assessments. MaxYield™ effectively maps ECG signals amidst noise, isolating and labeling key features in each heartbeat, and possesses the capability to analyze 200,000 heartbeats in under 5 minutes. This technological innovation is expected to , particularly in the early detection of cardiac obstruction conditions.
In addition, advancements in pacemaker technology, including leadless pacemakers, are changing the landscape of patient management. These devices provide a minimally invasive option with high implantation success rates and low infection risks, supported by studies indicating consistently low long-term complication rates. The incorporation of remote monitoring systems will further improve patient outcomes by facilitating continuous assessment and timely interventions.
Current research is also anticipated to investigate the genetic and environmental factors influencing cardiac obstruction, paving the way for personalized treatment strategies. As researchers delve into these aspects, the potential for customized therapies that cater to individual patient needs becomes increasingly attainable, ultimately enhancing care for those impacted by second degree type 2 heart block while utilizing MaxYield™'s capabilities to streamline workflows and bolster confident clinical decision-making.
Conclusion
Understanding second degree type 2 heart block is essential for effective diagnosis and management in cardiology. This condition, characterized by sporadic non-conducted P waves, poses significant risks, including complete heart block and sudden cardiac arrest. Advanced technologies, such as Neural Cloud Solutions' MaxYield™ platform, enhance the accuracy and efficiency of ECG analysis, providing healthcare professionals with vital insights for timely interventions.
The article has highlighted critical aspects of second degree type 2 heart block, including its:
- Definition
- Symptoms
- Diagnostic approaches
- Treatment strategies
Key points emphasize the importance of recognizing symptoms like dizziness and fatigue, identifying potential causes such as myocardial infarction, and understanding the role of pacemakers in management. Furthermore, the significance of lifestyle modifications, including a heart-healthy diet and regular exercise, cannot be overstated, as they contribute to better cardiovascular health.
As research continues to evolve, the potential for AI-driven technologies and advancements in pacemaker design promises to significantly improve patient outcomes. It is imperative for healthcare providers to stay informed about these developments and prioritize early detection and intervention strategies. By leveraging the insights provided in this article, both medical professionals and patients can work towards better management of second degree type 2 heart block, ultimately enhancing quality of life and reducing the risk of severe complications.
Frequently Asked Questions
What is Neural Cloud Solutions' MaxYield™ platform?
MaxYield™ is an advanced ECG analysis platform that utilizes AI algorithms to automate the identification of cardiac interruptions, including second degree type 2 heart block, by processing over 200,000 heartbeats in under five minutes.
How does MaxYield™ enhance ECG analysis?
MaxYield™ enhances ECG analysis by isolating critical ECG features such as P-waves, QRS complexes, and T-waves, which improves the clarity of ECG signals and aids in detecting irregularities linked to cardiac obstruction.
What is second degree type 2 heart block?
Second degree type 2 heart block, also known as Mobitz type II, is characterized by sporadic non-conducted P waves without gradual lengthening of the PR interval, indicating a serious disturbance in the heart's electrical conduction system.
Why is second degree type 2 heart block significant?
It can lead to severe complications such as complete heart block, congestive heart failure, and an increased risk of sudden cardiac arrest, making its swift identification and management crucial.
What symptoms are associated with second degree type 2 heart block?
Common symptoms include dizziness, lightheadedness, fatigue, syncope, and palpitations or a sensation of skipped heartbeats.
How effective is AI in predicting cardiac illnesses using MaxYield™?
AI-driven models within the MaxYield™ platform have achieved an accuracy of 93.6% in predicting cardiac illnesses, showcasing its potential in clinical settings.
How does MaxYield™ improve clinical workflows for cardiologists?
By automating ECG analysis, MaxYield™ reduces manual workload, allowing cardiologists to focus on high-level decision-making rather than time-consuming tasks.
Can MaxYield™ assist in treatment decisions?
Yes, case studies demonstrate that insights from MaxYield™ can inform treatment decisions, leading to improved patient outcomes, such as in cases where patients received pacemakers based on MaxYield™ analysis.
How does wearable technology integrate with MaxYield™?
Wearable technology can enhance ECG analysis efficiency by automating the labeling process and addressing challenges like physiological variability and signal artifacts when used alongside MaxYield™.
What should be done for patients with second degree type 2 heart block, even if asymptomatic?
Transcutaneous pacing should be applied to all patients with second degree type 2 heart block to prevent serious complications.


