Overview
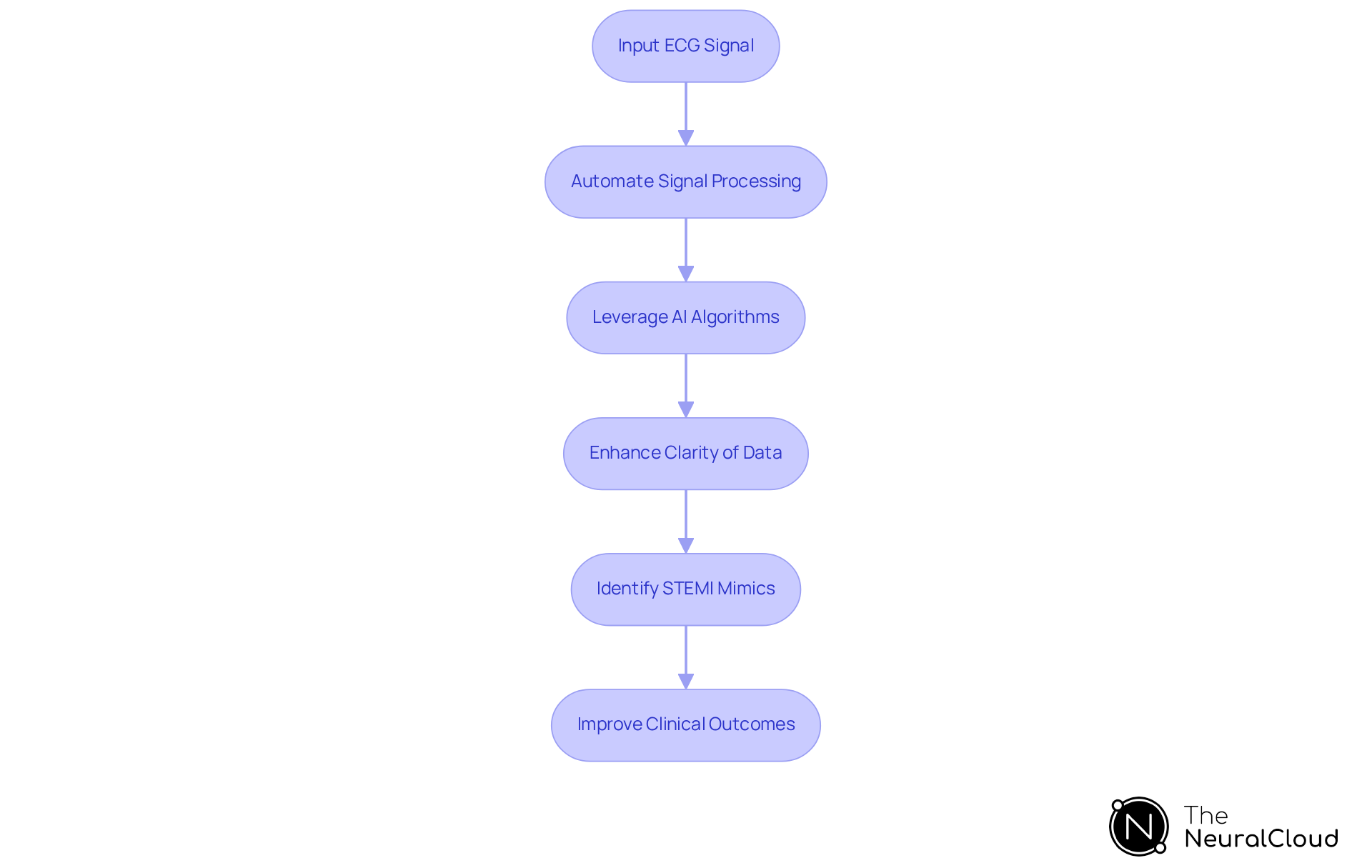
The article highlights the critical need for health tech developers to recognize and identify the ten key mimics of ST-Elevation Myocardial Infarction (STEMI), which can complicate ECG interpretations. It underscores the importance of advanced AI-driven platforms, such as Neural Cloud Solutions' MaxYield™, in enhancing diagnostic accuracy and improving clinical outcomes. By automating ECG analysis, MaxYield™ effectively distinguishes between true myocardial infarctions and various STEMI mimics, addressing the challenges faced in ECG analysis.
MaxYield™ offers several features that contribute to its effectiveness. The platform automates the ECG analysis process, allowing for quicker and more accurate interpretations. This automation reduces the cognitive load on healthcare professionals, enabling them to focus on patient care rather than manual analysis. Additionally, the platform is designed to adapt to various ECG presentations, ensuring comprehensive coverage of potential STEMI mimics.
The advantages of utilizing MaxYield™ are significant for healthcare professionals. By leveraging this technology, clinicians can achieve higher diagnostic accuracy, leading to timely interventions and improved patient outcomes. Furthermore, the platform's ability to distinguish between true myocardial infarctions and mimics minimizes the risk of misdiagnosis, ultimately enhancing the quality of care provided to patients.
In summary, the integration of advanced AI-driven platforms like MaxYield™ represents a pivotal advancement in ECG analysis. By understanding the complexities of STEMI and its mimics, health tech developers can contribute to more effective diagnostic tools that support healthcare professionals in delivering high-quality patient care.
Introduction
Identifying the nuances of ST-Elevation Myocardial Infarction (STEMI) is a lifesaving skill. However, the presence of various conditions that mimic its symptoms complicates diagnosis. For health tech developers, understanding these STEMI mimics is crucial. Misinterpretation can lead to inappropriate treatments and adverse patient outcomes. How can developers leverage advanced technologies like AI to enhance ECG analysis and improve diagnostic accuracy? This article delves into ten key STEMI mimics that every health tech developer should know. It highlights the importance of precise differentiation in clinical practice.
Neural Cloud Solutions: Advanced ECG Analysis for Identifying STEMI Mimics
Neural Cloud Solutions addresses the challenges in ECG analysis through its MaxYield™ platform, which provides advanced ECG analysis crucial for identifying stemi mimics. By automating ECG signal processing and leveraging sophisticated AI algorithms, the platform enhances the clarity of cardiac data. This advancement empowers healthcare practitioners to effectively distinguish between genuine heart attack cases and stemi mimics that may present similar ECG patterns.
The significance of accurate ECG interpretation is highlighted by cardiologists, who stress that ongoing chest pain accompanied by ECG changes should not be disregarded, even if it does not meet traditional ST-elevation MI criteria. Recent studies reveal that AI-driven ECG analysis can achieve an area under the curve (AUC) of 0.938 in detecting Occlusion Myocardial Infarction (OMI), demonstrating its superior accuracy compared to conventional methods.
Additionally, the MaxYield™ platform's capability to process over 200,000 heartbeats in less than five minutes facilitates rapid differentiation between myocardial infarction and stemi mimics, ultimately leading to improved clinical outcomes. As the field of AI in ECG analysis evolves in 2025, the integration of such advanced technologies becomes essential for health tech developers focused on enhancing accuracy and patient care.
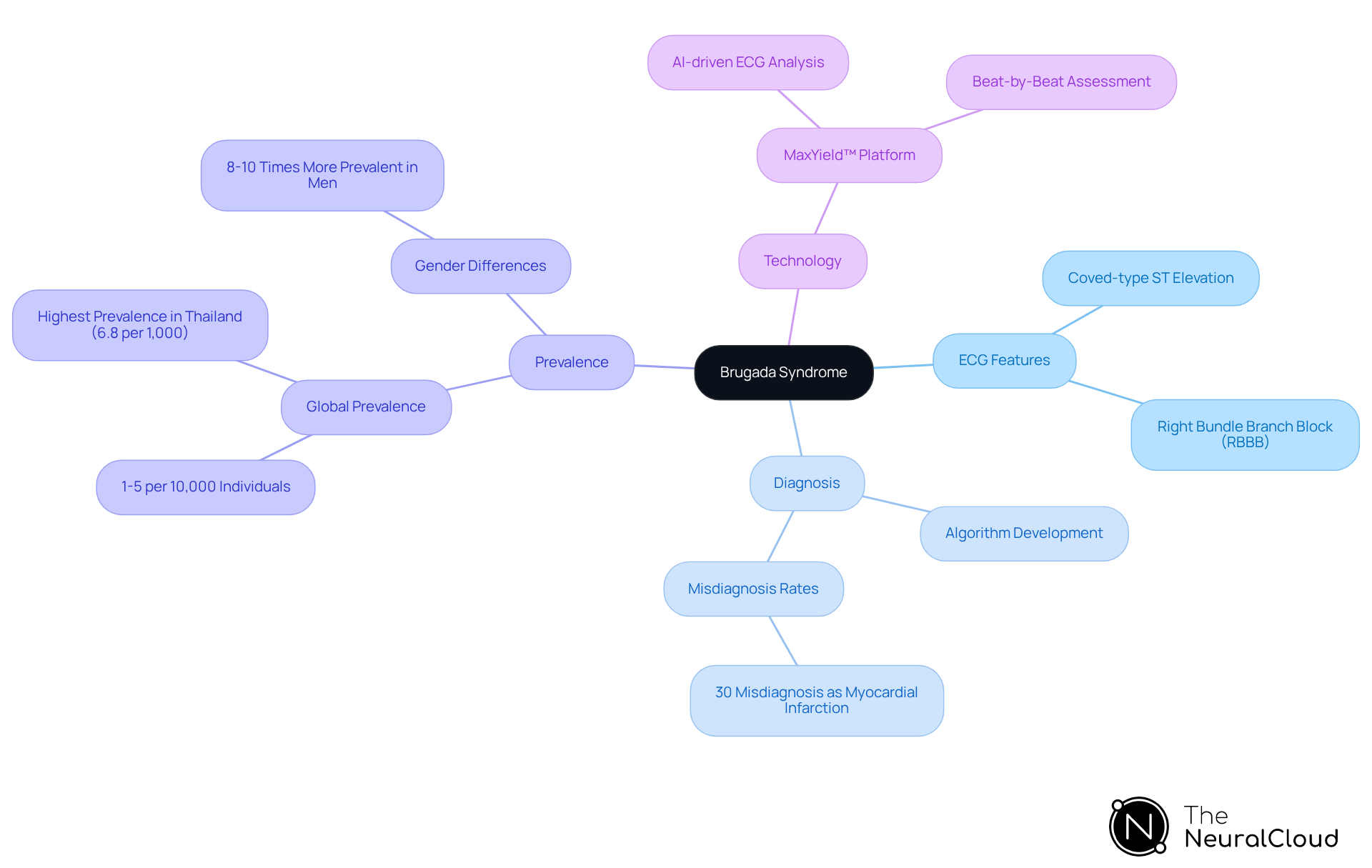
Brugada Syndrome: Recognizing ECG Features to Differentiate from STEMI
Brugada Syndrome is characterized by a distinctive coved-type ST-segment elevation in the right precordial leads (V1-V3), which can often be mistaken for a heart attack. Developers must prioritize the identification of this specific ST elevation pattern, along with the presence of a right bundle branch block (RBBB), to enhance assessment accuracy. Misdiagnosis rates for STEMI mimics versus Brugada Syndrome can be significant; studies indicate that up to 30% of cases may be incorrectly identified as myocardial infarction. This highlights the necessity of developing algorithms capable of recognizing these critical ECG features.
Neural Cloud Solutions' MaxYield™ platform plays a pivotal role in this process by leveraging advanced AI-driven automation and a continuous learning model to analyze ECG signals amidst noise, isolating and labeling key features in every heartbeat. MaxYield™ delivers beat-by-beat analysis, providing an assessment of 200,000 heartbeats in under 5 minutes, which enhances diagnostic yield over time. Practical applications of such algorithms have demonstrated their efficiency in differentiating STEMI mimics from these two conditions, ultimately improving outcomes for individuals.
Cardiologists emphasize that identifying the distinctive morphology of the coved-type ST elevation is essential for accurate diagnosis, as it directly influences treatment choices and safety. Additionally, Brugada Syndrome has a prevalence estimated at 1-5 per 10,000 individuals and is genetically determined, with approximately 50% of familial cases exhibiting an autosomal dominant inheritance pattern. The SCN5A gene accounts for around 30% of cases, underscoring the genetic factors associated with the condition.
It is also important to note that Brugada Syndrome is 8-10 times more prevalent in men than in women, with the typical individual being young, male, and otherwise healthy. Recognizing triggers for arrhythmias, such as fever and certain medications, is crucial for health tech developers in algorithm design. Integrating MaxYield™ can enhance the clarity and efficiency of this analysis.
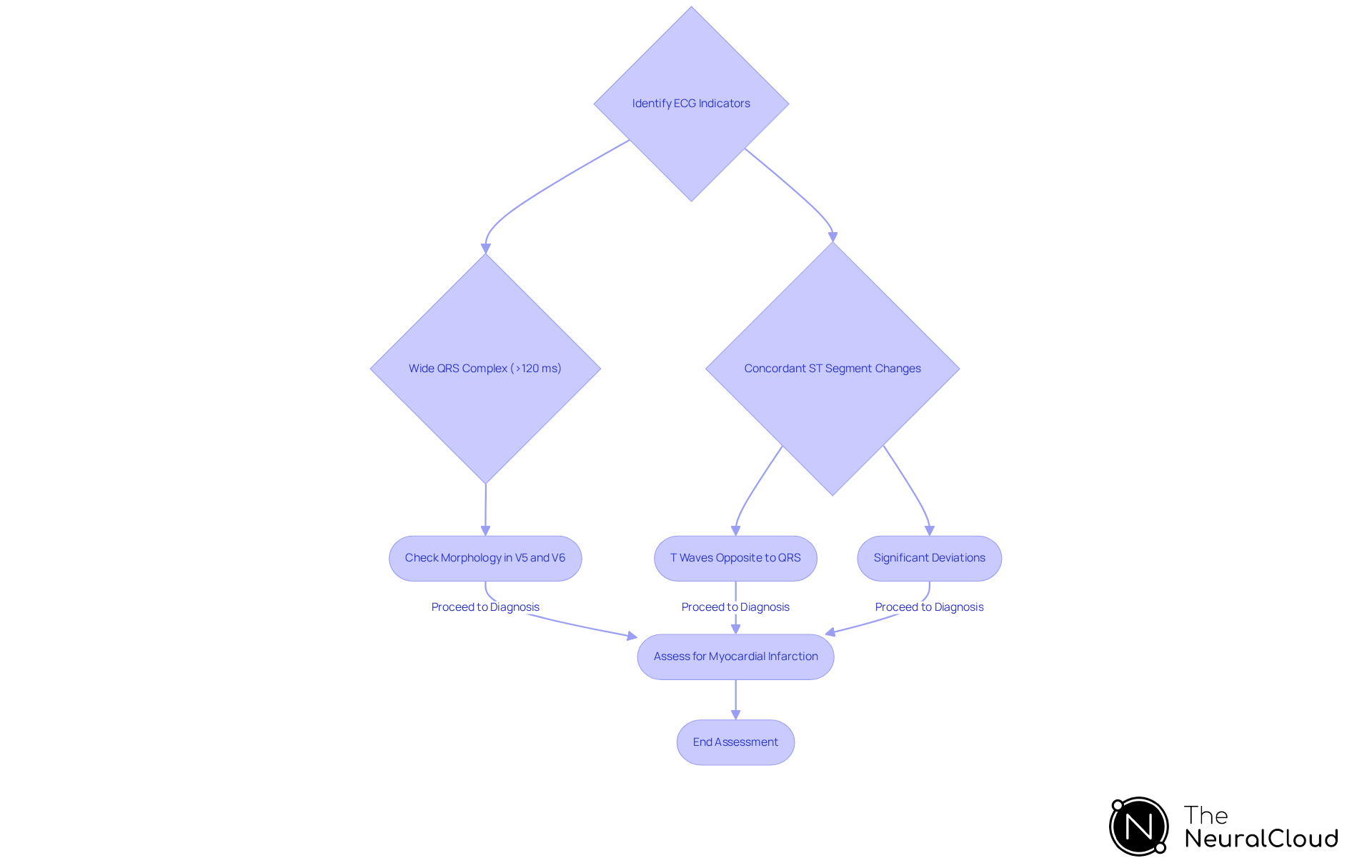
Left Bundle Branch Block (LBBB): Key ECG Indicators to Distinguish from STEMI
Left Bundle Branch Block (LBBB) is characterized by a wide QRS complex, typically exceeding 120 ms, and presents a distinctive 'M' shape in leads V5 and V6. This morphology can obscure the diagnosis of ST-Elevation Myocardial Infarction, particularly in anterior leads, resulting in stemi mimics that complicate clinical decision-making. Statistics indicate that LBBB is the second most prevalent stemi mimics of acute myocardial infarction, with only 1.2% of patients admitted for acute myocardial infarction also presenting with newly diagnosed LBBB. This highlights the assessment challenges encountered by healthcare professionals.
To reduce misdiagnosis, it is essential to create algorithms that accurately distinguish between LBBB and myocardial infarction. Key indicators include the presence of concordant ST segment changes and the morphology of the QRS complex. In LBBB, T waves typically orient opposite to the QRS terminal forces; significant deviations may indicate underlying cardiac dysfunction. Advanced algorithms, such as those utilized by Neural Cloud Solutions' MaxYield™, efficiently interpret ECG signals amidst interference and provide beat-by-beat analysis, enhancing accuracy in differentiating LBBB from other conditions.
Healthcare professionals emphasize the importance of recognizing these ECG indicators, as the presence of LBBB can lead to a 2.9 times increased risk of cardiovascular mortality and complicate the identification of stemi mimics and acute myocardial infarction. Understanding these subtleties is crucial for health tech developers aiming to design reliable assessment instruments that improve patient outcomes.
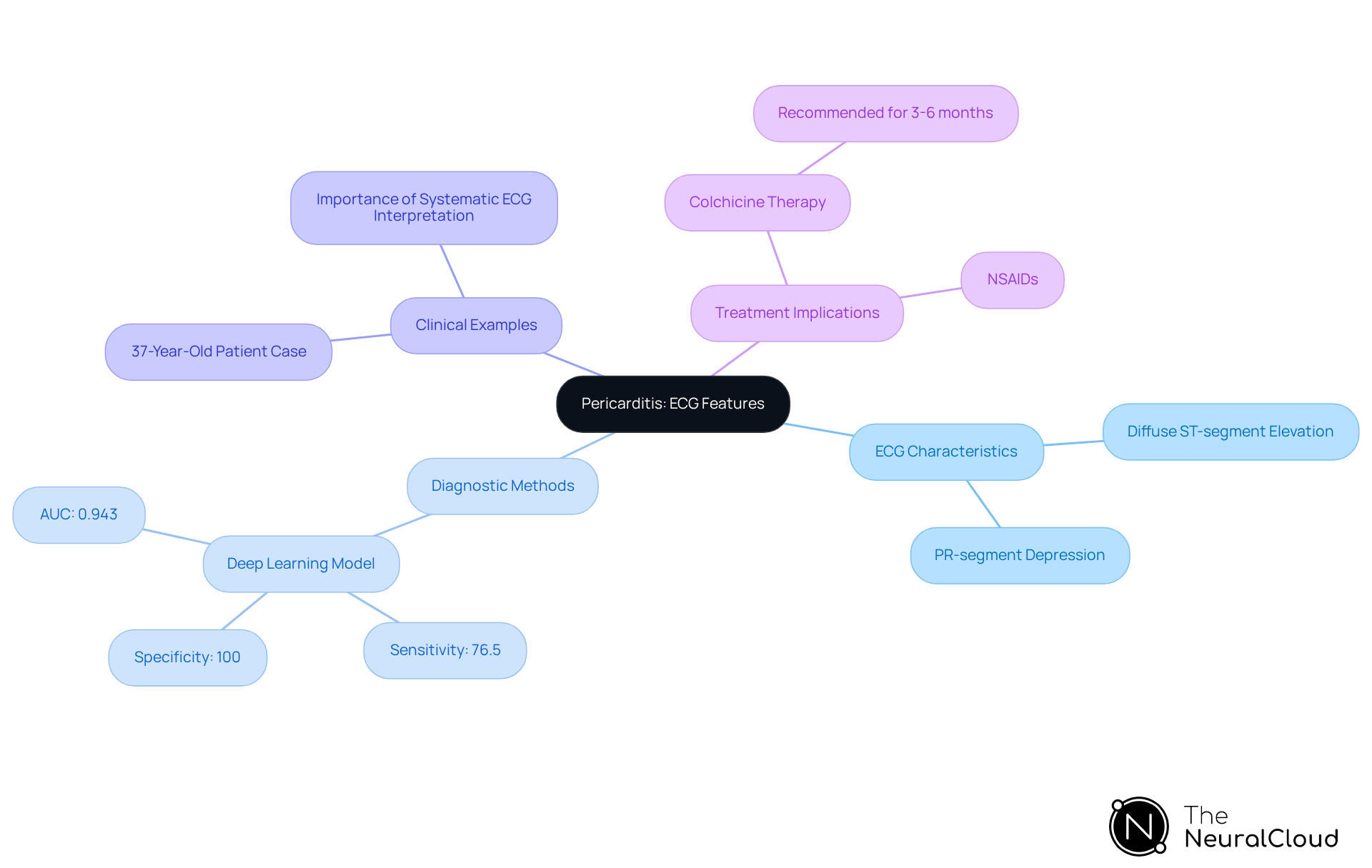
Pericarditis: Clinical Clues and ECG Features That Mimic STEMI
Pericarditis is characterized by diffuse ST-segment elevation across multiple leads, often accompanied by PR-segment depression. This pattern is essential for developers to identify, as it sharply contrasts with the localized ST elevation typically observed in stemi mimics. Understanding these unique ECG characteristics is vital for creating assessment instruments that can accurately distinguish between stemi mimics and myocardial infarction, including conditions like pericarditis.
In a recent study, a deep learning model demonstrated a sensitivity of 76.5% and a specificity of 100% in detecting pericarditis, outperforming traditional methods and human experts. This highlights the potential of advanced algorithms in enhancing assessment accuracy.
Real-world examples illustrate the importance of systematic ECG interpretation. For instance, a 37-year-old individual presenting with chest pain required a thorough examination to determine whether the ECG indicated myocardial infarction or pericarditis. By following established algorithms, clinicians were able to identify the condition as pericarditis, emphasizing the necessity for ongoing education in ECG analysis.
Experts emphasize that recognizing the typical ECG pattern of acute pericarditis—generalized, concave-upward ST-segment elevation with accompanying PR-segment depression—is crucial to differentiate it from stemi mimics. This understanding not only facilitates accurate diagnosis but also informs treatment decisions, as misdiagnosis can lead to inappropriate management strategies.
Integrating these insights into the development of assessment tools will enhance their effectiveness, ultimately improving patient outcomes in emergency situations.
Left Ventricular Hypertrophy (LVH): ECG Characteristics That Overlap with STEMI
Left Ventricular Hypertrophy (LVH) is characterized by increased voltage in the QRS complexes, particularly in the left precordial leads (V1-V6). This rise can result in ST-segment alterations that closely resemble those seen in stemi mimics, complicating the evaluation process. For instance, a T/QRS ratio greater than 0.36 suggests acute myocardial infarction rather than LVH, yet distinguishing between these conditions remains a challenge.
Healthcare professionals emphasize the importance of advanced algorithms in differentiating LVH from myocardial infarction. The MaxYield™ platform from Neural Cloud Solutions features advanced noise reduction and adaptive algorithms, significantly enhancing the ability to differentiate these patterns. This platform quickly isolates ECG waves from recordings with noise and artifacts, directly influencing assessment accuracy. Consequently, developers can create algorithms that effectively distinguish between LVH and myocardial infarction.
Misunderstandings between LVH and stemi mimics can significantly impact the accuracy of assessments. Studies indicate that the prevalence of LVH diagnosed by ECG is around 17.6%, and its presence can lead to stemi mimics that may result in misinterpretation of ST-segment elevation. This misinterpretation potentially results in delayed treatment for patients experiencing acute coronary events. Therefore, it is crucial for developers to focus on creating algorithms that accurately differentiate these overlapping ECG patterns, thereby improving clinical outcomes and resource allocation in emergency settings.
Incorporating machine learning models into ECG interpretation has shown promise in enhancing diagnostic precision. These models analyze subtle changes in ECG waveforms that may indicate ischemia, providing a more objective assessment compared to traditional methods. As the field advances, the integration of such technologies will be vital in addressing the complexities related to LVH and its effects on diagnosis.

Early Repolarization: Identifying ECG Features That Confuse STEMI Diagnosis
Early repolarization is characterized by J-point elevation and a concave ST-segment in the precordial leads, which can easily be mistaken for STEMI mimics like an ST-elevation myocardial infarction. This misdiagnosis is significant, as studies suggest that approximately 25% of acute myocardial infarction cases may show negative initial high-sensitivity troponin results, which can be mistaken for STEMI mimics. This complicates the clinical situation and emphasizes the necessity for precise assessment tools. Developers should prioritize algorithms capable of distinguishing between early repolarization and true STEMI mimics, as these tools are essential for enhancing assessment precision and outcomes for individuals.
Neural Cloud Solutions' MaxYield™ technology exemplifies this approach. It utilizes advanced noise filtering and automated signal processing to enhance ECG analysis. A recent study demonstrated that a machine learning model achieved a sensitivity of 89% and specificity of 95% in differentiating STEMI mimics from early repolarization. This underscores the importance of algorithmic differentiation in clinical practice.
Cardiologists stress the importance of relating ECG findings with clinical symptoms and other assessment markers, such as troponin levels, to ensure precise identification. As Dr. Smith notes, "It is critical to correlate ECG findings with the individual’s clinical presentation, symptoms, and additional diagnostic markers, such as troponin levels, to ensure an accurate diagnosis." The integration of advanced algorithms, like those found in MaxYield™, into clinical workflows can significantly reduce the risk of misdiagnosis, ultimately improving patient outcomes.

Ventricular Paced Rhythm: ECG Features to Differentiate from STEMI
Ventricular paced rhythms present significant challenges in ECG analysis, particularly due to the wide QRS complexes that can obscure classic findings of stemi mimics, especially in the inferior leads. This masking effect complicates the interpretation of ECGs, leading to potential diagnostic errors. Studies indicate that approximately 10-36% of individuals with ST-segment elevation on ECGs do not exhibit acute coronary occlusion upon angiography, underscoring the necessity for accurate rhythm identification.
Healthcare professionals recognize the difficulties in diagnosing stemi mimics in patients who have paced rhythms. The Modified Sgarbossa Criteria play a crucial role in assessing discordance between the ST-segment and QRS complex, facilitating the differentiation of true myocardial infarction from baseline abnormalities associated with pacing. Algorithms designed to identify paced rhythms can significantly enhance assessment accuracy, ensuring timely and appropriate treatment.
Neural Cloud Solutions' MaxYield™ platform effectively addresses these challenges by automating ECG analysis and providing beat-by-beat insights, analyzing 200,000 heartbeats in less than 5 minutes. This capability enables healthcare professionals to accurately identify cardiac events, even in the presence of ventricular paced rhythms. By transforming noisy recordings into detailed insights, MaxYield™ supports the detection of critical features such as P-wave, QRS complex, and T-wave intervals, thereby enhancing clarity and workflow efficiency.
Case studies illustrate that ECG features in ventricular paced rhythms can lead to misinterpretation, especially in the presence of stemi mimics and ST elevations. The occurrence of reciprocal changes, which are ST depressions found on the opposite side of the heart from the myocardial infarction, can further complicate diagnosis. Therefore, it is essential for developers to prioritize the integration of advanced algorithms like MaxYield™ that can accurately detect and differentiate paced rhythms, optimizing patient outcomes in emergency settings. Utilizing MaxYield™ can significantly enhance diagnostic accuracy and empower healthcare professionals to make informed clinical decisions.

Hyperkalemia: ECG Indicators and Clinical Clues That Mimic STEMI
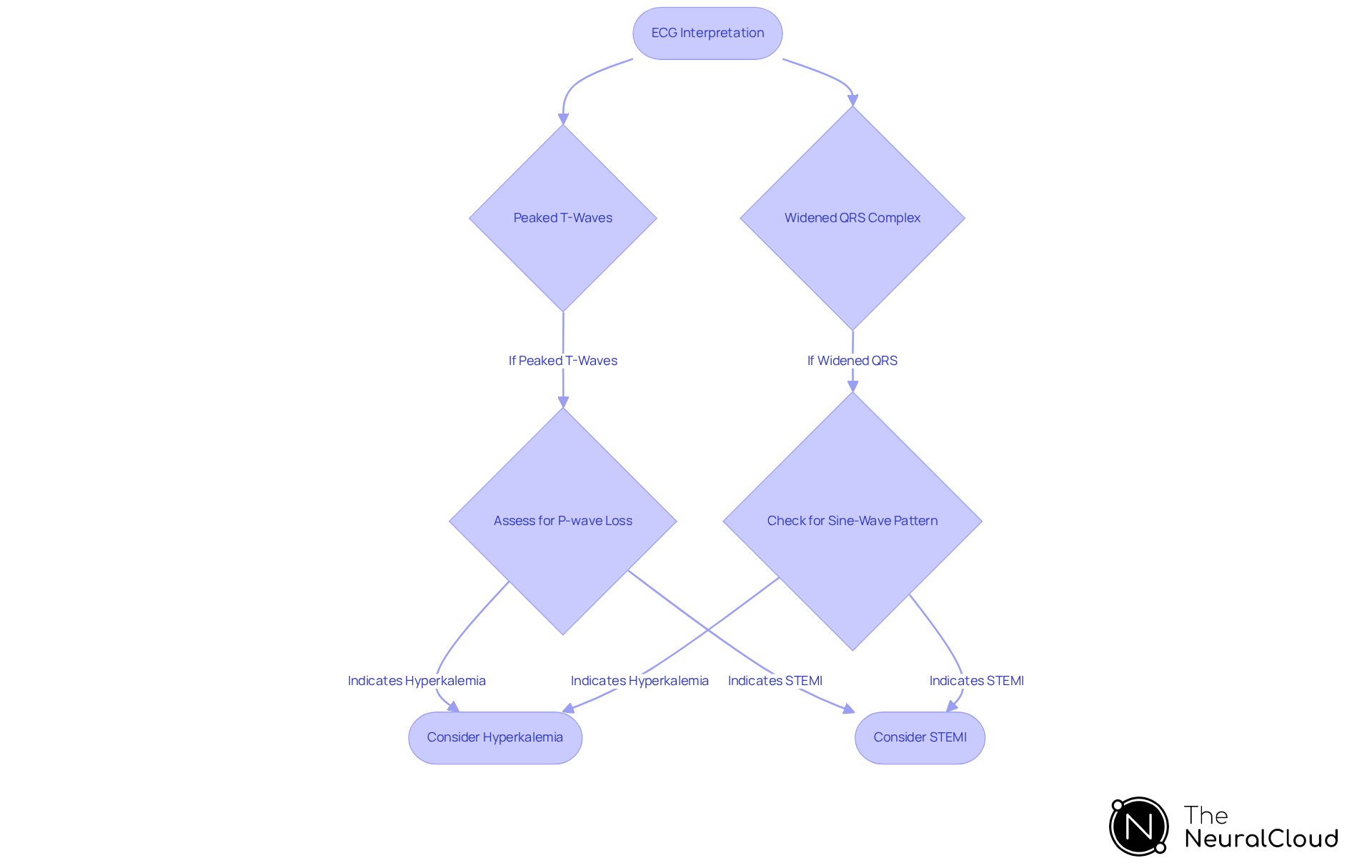
Hyperkalemia presents distinct ECG changes, such as peaked T-waves, widening of the QRS complex, and potential loss of P-waves. These modifications can closely resemble stemi mimics observed in acute myocardial infarction, making precise interpretation essential. For example, hyperacute T-waves, characterized by increased height and symmetry, may be the first sign of an evolving infarct, warranting close observation. In severe cases, the QRS complex can widen significantly, leading to a sine-wave pattern that complicates diagnosis.
To address these challenges, experts emphasize the necessity for developers to incorporate algorithms capable of differentiating between hyperkalemia and myocardial infarction. Neural Cloud Solutions' MaxYield™ platform offers advanced noise filtering and wave recognition. This technology enables the rapid isolation and labeling of critical ECG features, even in recordings with high levels of noise. As Daniel Kreider, MD, notes, early recognition of cardiac ischemia is crucial, as time is myocardium. Such differentiation is vital, given that studies show only approximately 43% of acute myocardial occlusions meet traditional criteria, emphasizing the need for improved diagnostic awareness of stemi mimics.
The implementation of MaxYield™, which continuously learns and enhances its algorithms, can significantly improve sensitivity in ECG interpretation. By focusing on these ECG indicators and leveraging MaxYield™'s capabilities, developers can contribute to more accurate and timely diagnoses. This ultimately leads to improved patient outcomes, as healthcare professionals can make informed decisions based on precise ECG analysis.
Pulmonary Embolism: ECG Features and Clinical Signs That Mimic STEMI
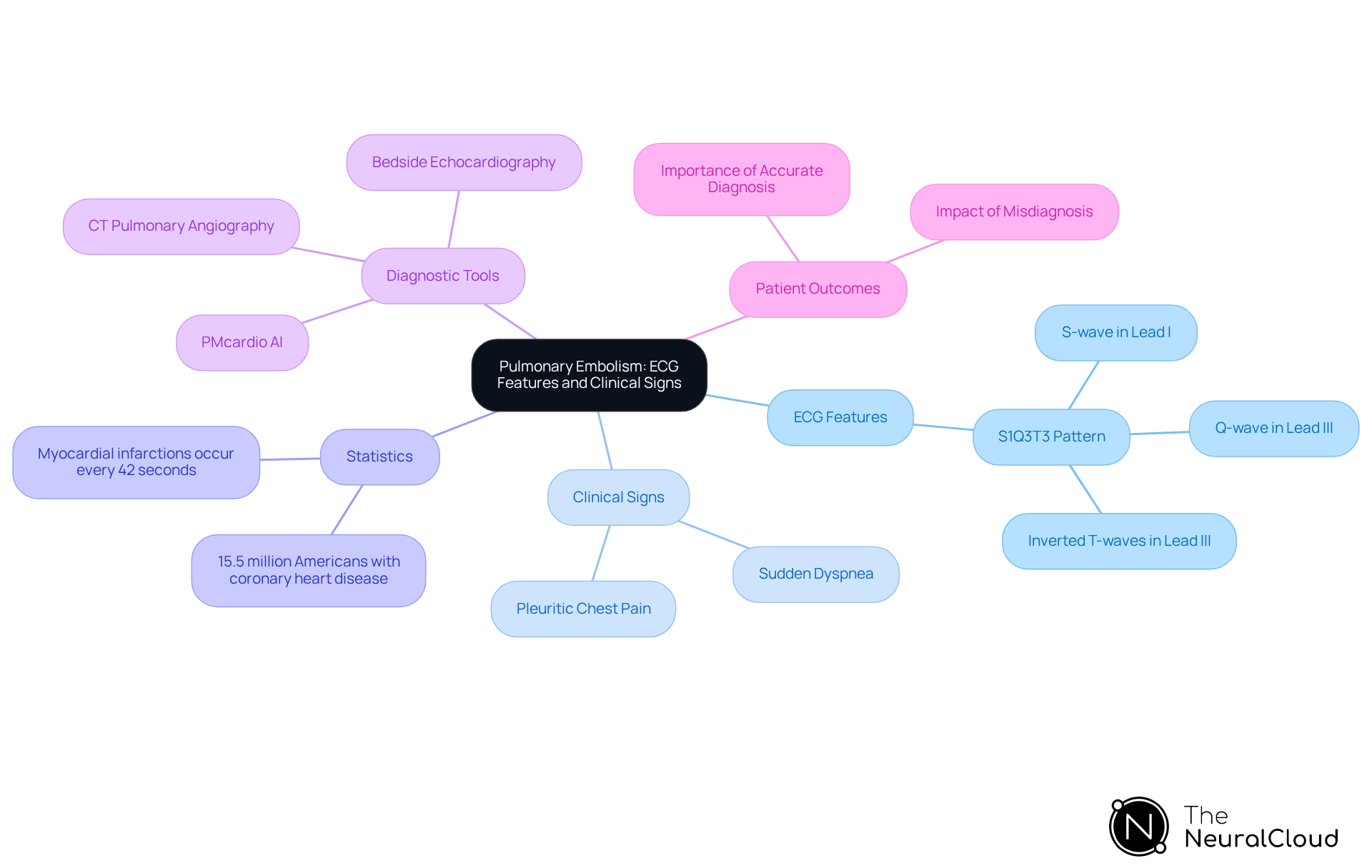
Pulmonary embolism (PE) can present with the S1Q3T3 pattern, which is characterized by a deep S-wave in lead I, a Q-wave in lead III, and inverted T-waves in lead III. Recognizing this unique pattern is essential for developers, as it markedly contrasts with the usual ECG results related to myocardial infarction. Understanding these differences is crucial for developing diagnostic instruments capable of precisely distinguishing between PE and myocardial infarction.
Statistics reveal that approximately 15.5 million Americans over the age of 20 suffer from coronary heart disease, with myocardial infarctions occurring every 42 seconds in the U.S. This highlights the importance of accurate ECG interpretation in emergency settings. Misdiagnosing STEMI mimics, such as PE, can lead to unnecessary invasive procedures and mismanagement of patient care.
Healthcare professionals stress the necessity of maintaining a high clinical suspicion when interpreting ECGs for PE. Although the classic S1Q3T3 pattern is indicative of PE, it lacks the sensitivity and specificity required to exclude myocardial infarction. Consequently, integrating advanced diagnostic tools and imaging studies, such as CT pulmonary angiography, is vital for achieving accurate diagnoses. Neural Cloud Solutions' MaxYield™ platform enhances this process by automating ECG analysis, reducing noise, and providing detailed insights that assist in differentiating between these critical conditions. MaxYield™ offers beat-by-beat analysis, isolating key features in ECG signals to transform noisy recordings into actionable insights.
Real-world examples illustrate the challenges in distinguishing PE from STEMI mimics. For instance, an individual with PE may exhibit respiratory symptoms like sudden dyspnea and pleuritic chest pain, which complicates the clinical picture. Effective communication among healthcare providers, combined with the advanced algorithms integral to the MaxYield™ platform, can enhance accuracy in assessments, ultimately improving patient outcomes in critical situations.
Advanced Diagnostics: Leveraging AI to Identify STEMI Mimics Effectively
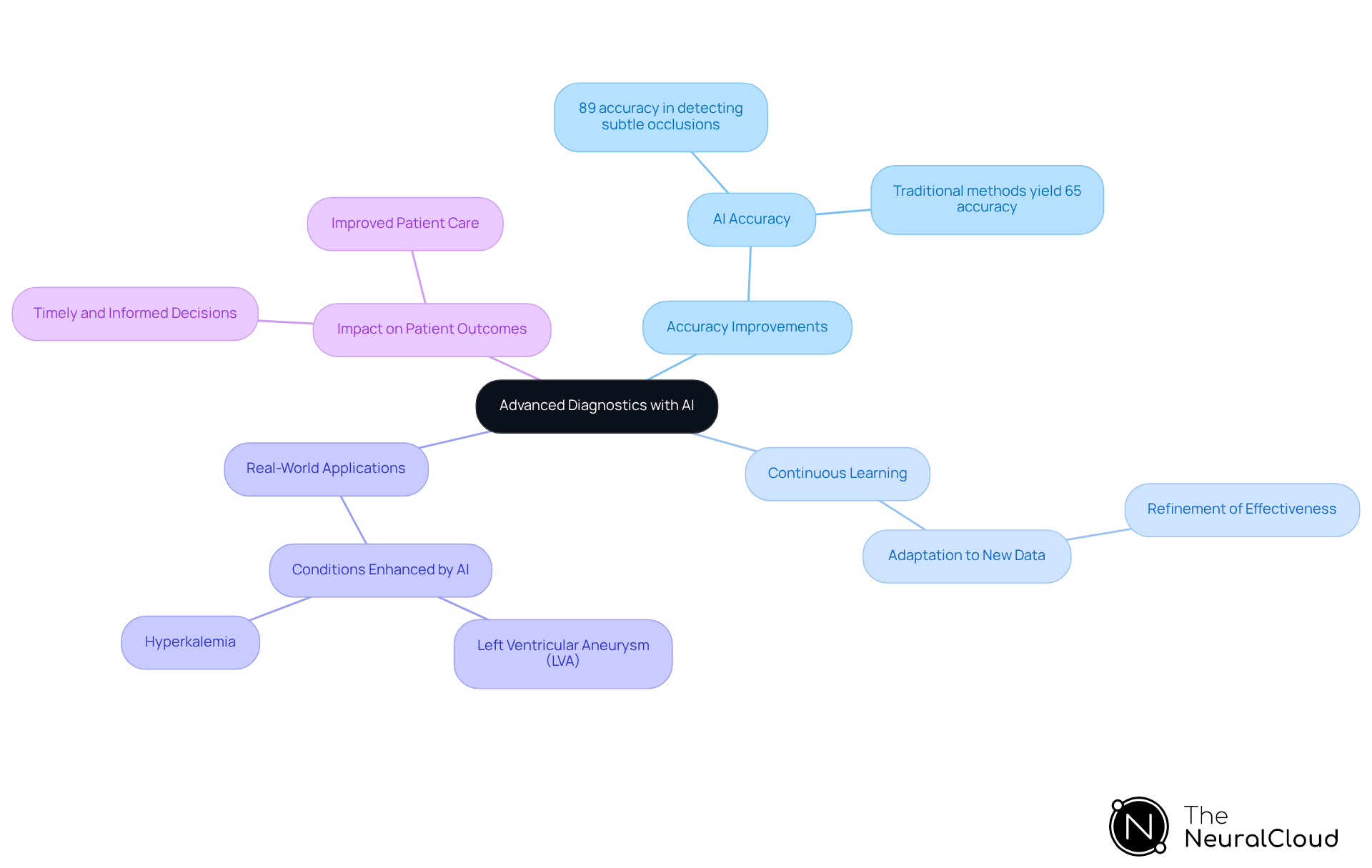
Advanced diagnostics powered by artificial intelligence are transforming the identification of stemi mimics. By utilizing machine learning algorithms that analyze extensive datasets of ECG patterns, developers are creating innovative tools that significantly enhance assessment precision and minimize the risk of misdiagnosis. Recent advancements indicate that AI can achieve an accuracy of approximately 89% in detecting subtle occlusions, surpassing traditional methods that yield around 65% accuracy. This development highlights AI's potential to revolutionize emergency medicine and improve patient outcomes.
The continuous learning capabilities of AI ensure that these assessment tools evolve, adapting to new data and refining their effectiveness over time. Experts in the field emphasize that integrating machine learning into ECG analysis not only streamlines the diagnostic process but also increases the precision of distinguishing true myocardial infarctions from stemi mimics. This distinction is particularly critical given that approximately 24-35% of patients with non-STEMI present with total coronary occlusion, which requires urgent intervention.
Real-world applications of these algorithms illustrate their impact on heart attack diagnosis accuracy. For instance, machine learning models have been developed that markedly enhance the differentiation between STEMI and stemi mimics such as left ventricular aneurysm (LVA) and hyperkalemia, which may exhibit similar ECG patterns. By leveraging advanced AI-driven solutions, healthcare professionals can make timely and informed decisions, ultimately leading to improved patient care and outcomes.
Conclusion
Understanding the various conditions that can mimic ST-Elevation Myocardial Infarction (STEMI) is crucial for healthcare professionals, particularly health tech developers. This article highlights the significance of accurately identifying these STEMI mimics, as misdiagnosis can lead to inappropriate treatments and adverse patient outcomes. Leveraging advanced technologies, such as Neural Cloud Solutions' MaxYield™ platform, significantly enhances the differentiation between genuine myocardial infarction and conditions like:
- Brugada Syndrome
- Left Bundle Branch Block
- Pericarditis
- Others
Key insights emphasize the importance of recognizing specific ECG features associated with each mimic, which can be complex and nuanced. The integration of artificial intelligence into ECG analysis is transforming how these conditions are identified, providing healthcare practitioners with the tools necessary to make informed decisions swiftly. With AI achieving superior accuracy in distinguishing between STEMI and its mimics, the potential for improved patient care is substantial.
As the landscape of health technology continues to evolve, the role of advanced diagnostic tools cannot be overstated. Developers are encouraged to focus on creating algorithms that enhance the clarity and accuracy of ECG interpretation. By doing so, they not only contribute to better clinical outcomes but also ensure that healthcare professionals are equipped to navigate the complexities of cardiac diagnostics effectively. Recognizing and addressing STEMI mimics is not just an academic exercise; it is a vital component of improving patient safety and care in emergency settings.
Frequently Asked Questions
What is Neural Cloud Solutions' MaxYield™ platform?
The MaxYield™ platform is an advanced ECG analysis tool that automates ECG signal processing and uses sophisticated AI algorithms to enhance the clarity of cardiac data, helping healthcare practitioners distinguish between genuine heart attack cases and STEMI mimics.
How does the MaxYield™ platform improve ECG analysis?
It improves ECG analysis by processing over 200,000 heartbeats in less than five minutes, allowing for rapid differentiation between myocardial infarction and STEMI mimics, ultimately leading to better clinical outcomes.
What is the significance of accurate ECG interpretation?
Accurate ECG interpretation is crucial as ongoing chest pain with ECG changes should not be ignored, even if it does not meet traditional ST-elevation MI criteria. Misinterpretation can lead to significant clinical consequences.
What is Brugada Syndrome, and how can it be mistaken for a heart attack?
Brugada Syndrome is characterized by a distinctive coved-type ST-segment elevation in the right precordial leads (V1-V3) and can often be mistaken for a heart attack. Misdiagnosis rates for STEMI mimics versus Brugada Syndrome can be as high as 30%.
How does the MaxYield™ platform assist in diagnosing Brugada Syndrome?
The MaxYield™ platform uses advanced AI-driven automation and continuous learning to analyze ECG signals, isolating and labeling key features, which enhances the accuracy of diagnosing conditions like Brugada Syndrome.
What are the key ECG indicators for Left Bundle Branch Block (LBBB)?
LBBB is characterized by a wide QRS complex (exceeding 120 ms) and an 'M' shape in leads V5 and V6. Recognizing these indicators is essential to distinguish LBBB from ST-Elevation Myocardial Infarction.
Why is it important to differentiate LBBB from myocardial infarction?
Accurate differentiation is crucial as the presence of LBBB can lead to a 2.9 times increased risk of cardiovascular mortality and complicates the identification of STEMI mimics and acute myocardial infarction.
What role does AI play in ECG analysis for STEMI mimics?
AI enhances ECG analysis by providing beat-by-beat assessments and improving diagnostic yield over time, which is essential for distinguishing between conditions like STEMI mimics, Brugada Syndrome, and LBBB.


