Overview
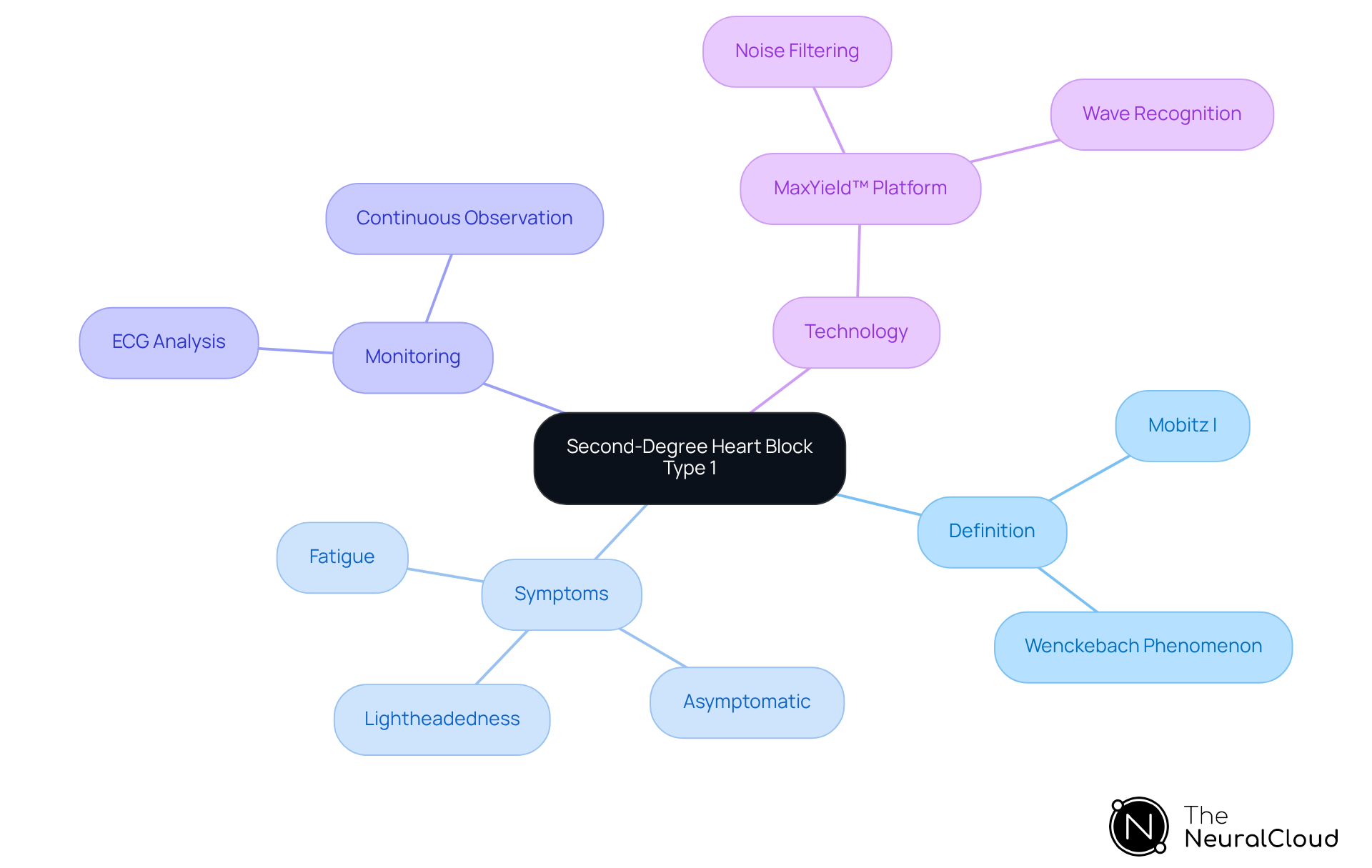
Second-degree heart block type 1, commonly referred to as Mobitz I or the Wenckebach phenomenon, is identified by a progressive elongation of the PR interval observed on an ECG. This condition can lead to occasional missed beats and is generally regarded as less serious due to its benign nature and low risk of evolving into more severe forms.
The article discusses the challenges associated with ECG analysis and introduces advanced diagnostic methods utilizing the MaxYield™ platform for precise ECG interpretation. This platform enhances the accuracy of ECG analysis, providing healthcare professionals with reliable tools for diagnosis.
Treatment strategies for patients often include observation and medication, highlighting that many individuals remain asymptomatic and may not require intervention. The emphasis on the MaxYield™ platform reflects its significant role in improving patient outcomes through better diagnostic capabilities.
Introduction
Understanding the complexities of second-degree heart block type 1, also known as Mobitz I, is essential for both patients and healthcare providers. This condition is characterized by a progressive delay in electrical signals within the heart. While it often presents minimal symptoms and a favorable prognosis, it raises critical questions about diagnosis and management strategies. The challenge lies in effectively navigating the nuances of this heart block to ensure optimal patient outcomes.
Advancements in technology, such as the MaxYield™ platform, enhance the precision of electrocardiogram (ECG) analysis. The MaxYield™ platform offers several key features:
- It improves the accuracy of signal detection
- It streamlines the interpretation process
- It provides real-time data analytics
These features enable healthcare professionals to make informed decisions based on precise data.
The advantages of utilizing the MaxYield™ platform are significant. By improving the accuracy of ECG analysis, healthcare providers can reduce the likelihood of misdiagnosis and enhance patient safety. Furthermore, the platform's user-friendly interface allows for quicker interpretation, which can lead to timely interventions and better patient outcomes. As a result, healthcare professionals are better equipped to manage conditions like Mobitz I effectively.
In conclusion, understanding second-degree heart block type 1 is crucial for effective patient management. With tools like the MaxYield™ platform, healthcare providers can navigate the complexities of ECG analysis with greater confidence, ultimately leading to improved patient care.
Define Second-Degree Heart Block Type 1
2nd degree heart block type 1, commonly referred to as Mobitz I or the Wenckebach phenomenon, is characterized by a progressive elongation of the PR interval on an electrocardiogram (ECG) until a P wave fails to transmit to the ventricles, resulting in a missed beat. This condition, which is identified as 2nd degree heart block type 1, typically arises from a reversible conduction interruption at the atrioventricular (AV) node. In contrast to more severe cardiac conduction disorders, 2nd degree heart block type 1 is generally considered less serious, as it rarely indicates intrinsic conduction disease and seldom requires pacemaker installation.
Patients diagnosed with 2nd degree heart block type 1 may remain asymptomatic; however, some might experience mild symptoms such as lightheadedness or fatigue, particularly if the conduction obstruction is more pronounced. Recent studies indicate that this type of cardiac obstruction can occur in highly trained athletes and individuals without structural cardiac abnormalities, often during sleep or periods of rest. The benign nature of 2nd degree heart block type 1, as classified by Mobitz Classification I, is underscored by its low probability of progressing to more severe heart block types, offering a favorable prognosis for the majority of patients.
Practical examples of ECG analysis illustrate that Mobitz Classification I can be effectively monitored through continuous electrocardiographic observation, especially among younger and physically fit individuals. The incorporation of advanced technologies, such as Neural Cloud Solutions' MaxYield™ platform, significantly enhances this monitoring process by employing sophisticated noise filtering and distinctive wave recognition capabilities. This technology facilitates the rapid isolation of ECG waves from recordings that may be affected by baseline wander, movement, or muscle artifacts, thereby enabling healthcare professionals to make informed decisions based on reliable cardiac insights.
Understanding the intricacies of 2nd degree heart block type 1 in the is crucial for developing effective diagnostic and treatment strategies within clinical practice. The MaxYield™ platform not only streamlines ECG analysis but also empowers healthcare providers with the tools necessary to improve patient outcomes.
Diagnose Second-Degree Heart Block Type 1
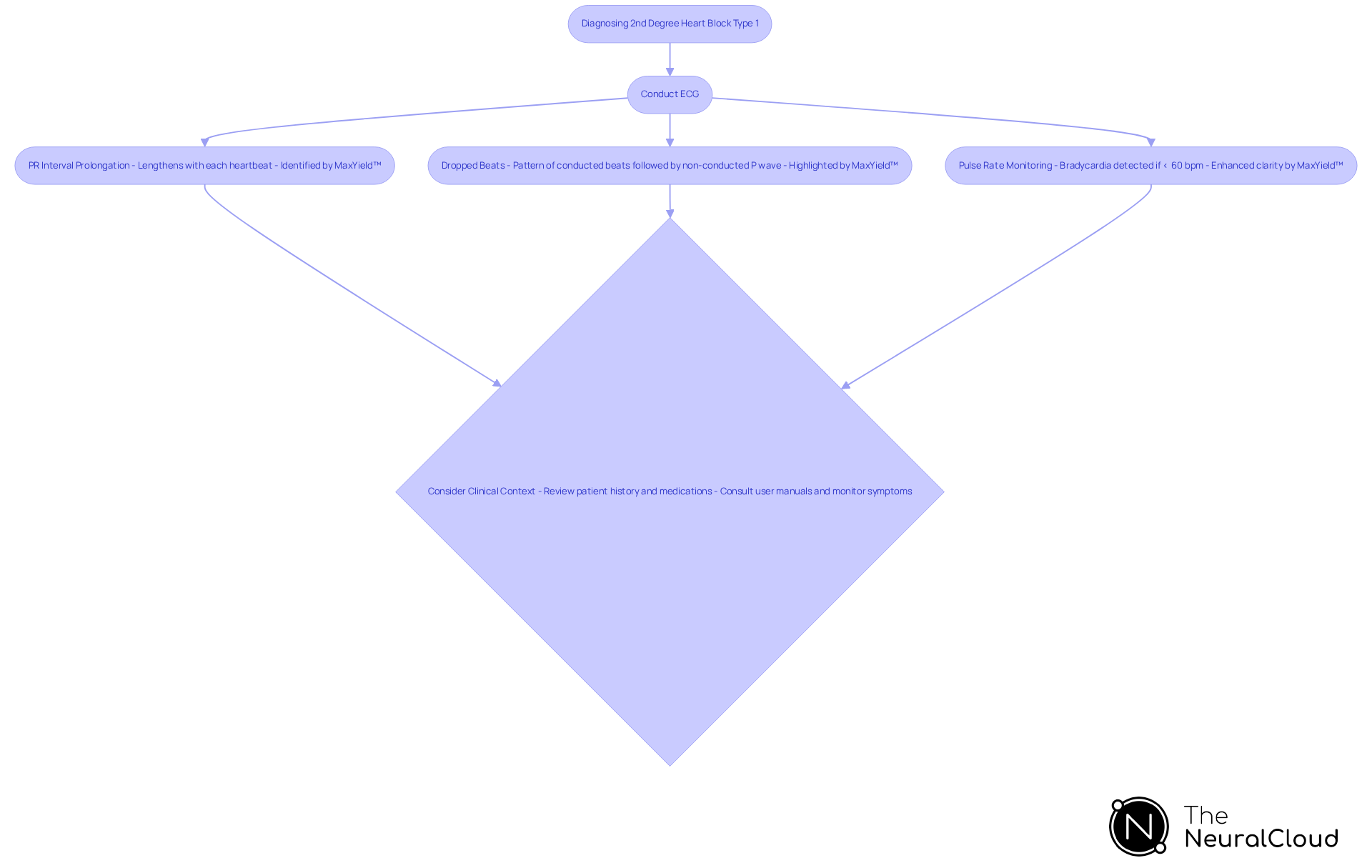
The diagnosis of 2nd degree heart block type 1 primarily involves the use of an electrocardiogram (ECG), and the integration of MaxYield™ significantly enhances this process. The challenges in ECG analysis include accurately identifying key diagnostic features, which are crucial for effective patient management.
Key Diagnostic Features of MaxYield™:
- PR Interval Prolongation: The PR interval progressively lengthens with each heartbeat until a P wave is not followed by a QRS complex. MaxYield™'s advanced algorithms accurately identify these changes, even in recordings with high levels of noise and artifact.
- Dropped Beats: The ECG will show a pattern of conducted beats followed by a non-conducted P wave, which is indicative of 2nd degree heart block type 1 and signifies a missed ventricular contraction. The platform's automated labeling capabilities ensure that these critical data points are highlighted for healthcare professionals.
- Pulse Rate Monitoring: Patients may exhibit bradycardia, characterized as a pulse rate of fewer than 60 beats per minute, which can be detected during the ECG. MaxYield™ enhances the clarity of these readings, allowing for more precise monitoring.
- Clinical Context: It is important to consider the individual's clinical history, symptoms, and any medications that may contribute to the 2nd degree heart block type 1, such as beta-blockers or digoxin. The adaptability of MaxYield™ means that it evolves with each use, continuously improving its diagnostic yield and efficiency.
For healthcare professionals utilizing MaxYield™, it is recommended to refer to the user manuals for detailed guidance on effectively implementing these features in practice. In certain situations, additional monitoring might be necessary, particularly if the individual shows symptoms or if there is concern about underlying heart disease. With MaxYield™, healthcare professionals can , overcoming inefficiencies and physiological variability to provide improved care for individuals.
Treat Second-Degree Heart Block Type 1
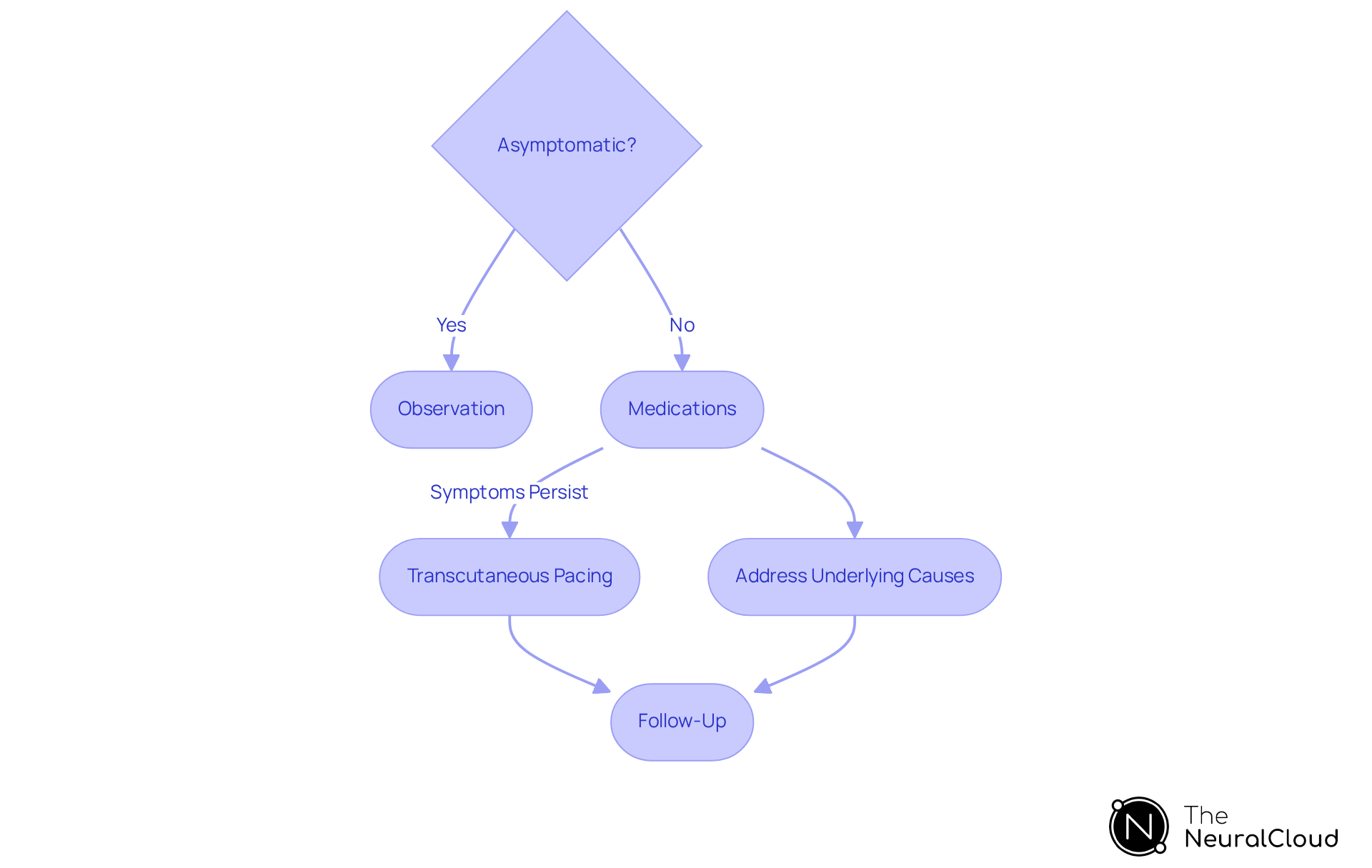
Management for 2nd degree heart block type 1 is often unnecessary for individuals who are asymptomatic. However, when symptoms do occur, several management strategies are recommended:
- Observation: For those who are asymptomatic, regular monitoring is typically adequate, as many individuals with 2nd degree heart block type 1 do not progress to a more severe block.
- Medications: In instances of symptomatic bradycardia or hypotension, such as in patients with 2nd degree heart block type 1, atropine is frequently administered. The standard dosage is 0.5 mg intravenously, which can be repeated every 3-5 minutes, up to a maximum of 3 mg. Research indicates that atropine effectively alleviates bradycardia symptoms in many patients, enhancing pulse stability. For instance, a study found that atropine improved pulse rate in 70% of patients experiencing symptomatic bradycardia.
- Transcutaneous Pacing: In emergency situations where symptoms persist despite atropine administration, may be necessary to stabilize the pulse rate.
- Addressing Underlying Causes: If the cardiac obstruction is due to reversible factors, such as medication side effects or electrolyte imbalances, correcting these issues can often resolve the problem.
- Follow-Up: Continuous monitoring and follow-up ECGs are crucial to ensure that the condition does not worsen and to evaluate the effectiveness of the treatment plan. Regular assessments are particularly important for patients over 45 years old, who face an increased risk of progression to higher degrees of heart block, as emphasized in recent guidelines.
Conclusion
Understanding 2nd degree heart block type 1, also known as Mobitz I or the Wenckebach phenomenon, is essential for effective diagnosis and management. This condition is characterized by a gradual elongation of the PR interval leading to missed beats. Generally benign, it often does not necessitate invasive interventions like pacemaker installation. The insights provided about its diagnosis and treatment highlight the importance of accurate ECG analysis and the role of advanced technologies, such as the MaxYield™ platform, in enhancing patient care.
Key points discussed include the diagnostic features that healthcare professionals should be aware of, such as:
- The progressive PR interval prolongation
- The presence of dropped beats
The article emphasizes the significance of continuous monitoring, especially in asymptomatic patients, while outlining treatment strategies for symptomatic individuals. From medication administration to potential pacing in emergencies, managing 2nd degree heart block type 1 requires a nuanced approach tailored to the patient's clinical context.
Ultimately, this guide serves as a crucial resource for healthcare providers, equipping them with the knowledge and tools needed to navigate the complexities of 2nd degree heart block type 1. By prioritizing accurate diagnosis and effective management strategies, healthcare professionals can significantly improve patient outcomes and ensure that individuals with this condition receive appropriate care.
Frequently Asked Questions
What is second-degree heart block type 1?
Second-degree heart block type 1, also known as Mobitz I or the Wenckebach phenomenon, is characterized by a progressive elongation of the PR interval on an electrocardiogram (ECG) until a P wave fails to transmit to the ventricles, resulting in a missed beat.
What causes second-degree heart block type 1?
This condition typically arises from a reversible conduction interruption at the atrioventricular (AV) node.
How serious is second-degree heart block type 1?
It is generally considered less serious than more severe cardiac conduction disorders, as it rarely indicates intrinsic conduction disease and seldom requires pacemaker installation.
What symptoms might patients with second-degree heart block type 1 experience?
Patients may remain asymptomatic, but some might experience mild symptoms such as lightheadedness or fatigue, especially if the conduction obstruction is more pronounced.
Can second-degree heart block type 1 occur in athletes?
Yes, recent studies indicate that this type of cardiac obstruction can occur in highly trained athletes and individuals without structural cardiac abnormalities, often during sleep or periods of rest.
What is the prognosis for patients with second-degree heart block type 1?
The prognosis is generally favorable, as there is a low probability of progressing to more severe heart block types.
How can second-degree heart block type 1 be monitored?
It can be effectively monitored through continuous electrocardiographic observation, particularly among younger and physically fit individuals.
What technologies enhance the monitoring of second-degree heart block type 1?
Advanced technologies, such as Neural Cloud Solutions' MaxYield™ platform, enhance monitoring by employing sophisticated noise filtering and distinctive wave recognition capabilities.
What benefits does the MaxYield™ platform provide in ECG analysis?
The platform facilitates the rapid isolation of ECG waves from recordings affected by baseline wander, movement, or muscle artifacts, enabling healthcare professionals to make informed decisions based on reliable cardiac insights.
Why is understanding second-degree heart block type 1 important in clinical practice?
Understanding this condition is crucial for developing effective diagnostic and treatment strategies, ultimately improving patient outcomes.


