Introduction
Understanding left ventricular hypertrophy (LVH) is essential for healthcare professionals, as it often indicates serious underlying cardiovascular issues. A significant portion of the population is affected by this condition, making it vital for clinicians to master ECG interpretation techniques. This mastery can lead to timely interventions that save lives. However, navigating the complexities of LVH diagnosis can be challenging due to potential confounding factors and evolving technologies.
This article explores the challenges in ECG analysis and introduces the MaxYield™ platform, which enhances ECG interpretation. The platform offers features designed to simplify the diagnostic process, making it easier for healthcare professionals to identify LVH accurately. By leveraging advanced algorithms and user-friendly interfaces, MaxYield™ improves the efficiency of ECG analysis, allowing clinicians to focus on patient care.
The advantages of using MaxYield™ are significant. Healthcare professionals can expect improved diagnostic accuracy, reduced time spent on analysis, and ultimately better patient outcomes. With the right tools, clinicians can enhance their understanding of LVH and its implications for cardiovascular health. This article aims to equip readers with essential insights and strategies for mastering ECG analysis of LVH, fostering a deeper understanding of this critical condition.
Define Left Ventricular Hypertrophy and Its Clinical Importance
ECG left ventricular hypertrophy (LVH) is characterized by an increase in the size of the myocardial fibers in the left ventricle, which is the heart's main pumping chamber. Clinically, ECG left ventricular hypertrophy (LVH) is significant as it often indicates underlying conditions such as hypertension or aortic stenosis, which can lead to serious cardiovascular events if left untreated. The prevalence of LVH is notably high, affecting 15% to 20% of the general population, with rates reaching up to 77% among high-risk hypertensive individuals. Early detection of ECG left ventricular hypertrophy (LVH) is vital, as it facilitates timely interventions that can significantly reduce morbidity and mortality associated with heart disease.
The MaxYield™ platform enhances ECG analysis by identifying and labeling critical data, even in recordings with high levels of noise and artifact. This capability allows for the rapid isolation of ECG waves from recordings affected by baseline wander, movement, and muscle artifact. As a result, previously obscured sections of lengthy Holter, 1-Lead, and patch monitor recordings can be salvaged, improving the overall quality of ECG interpretation.
Notably, only 26% of individuals with TTE-LVH are on antihypertensive medications, highlighting a critical treatment gap. The algorithm evolves with each use, continuously enhancing its precision and effectiveness. This evolution is crucial for cardiologists and healthcare providers, enabling them to implement successful treatment strategies and enhance patient outcomes.
As Daniel Levy M.D. noted, "Left ventricular mass (corrected for height) was associated with death from all causes," underscoring the importance of recognizing LVH as an independent risk factor for cardiovascular disease. Real-world examples demonstrate that effective screening and monitoring, supported by advanced technologies like MaxYield™, can lead to better management of hypertension and ECG left ventricular hypertrophy, ultimately enhancing cardiovascular health.

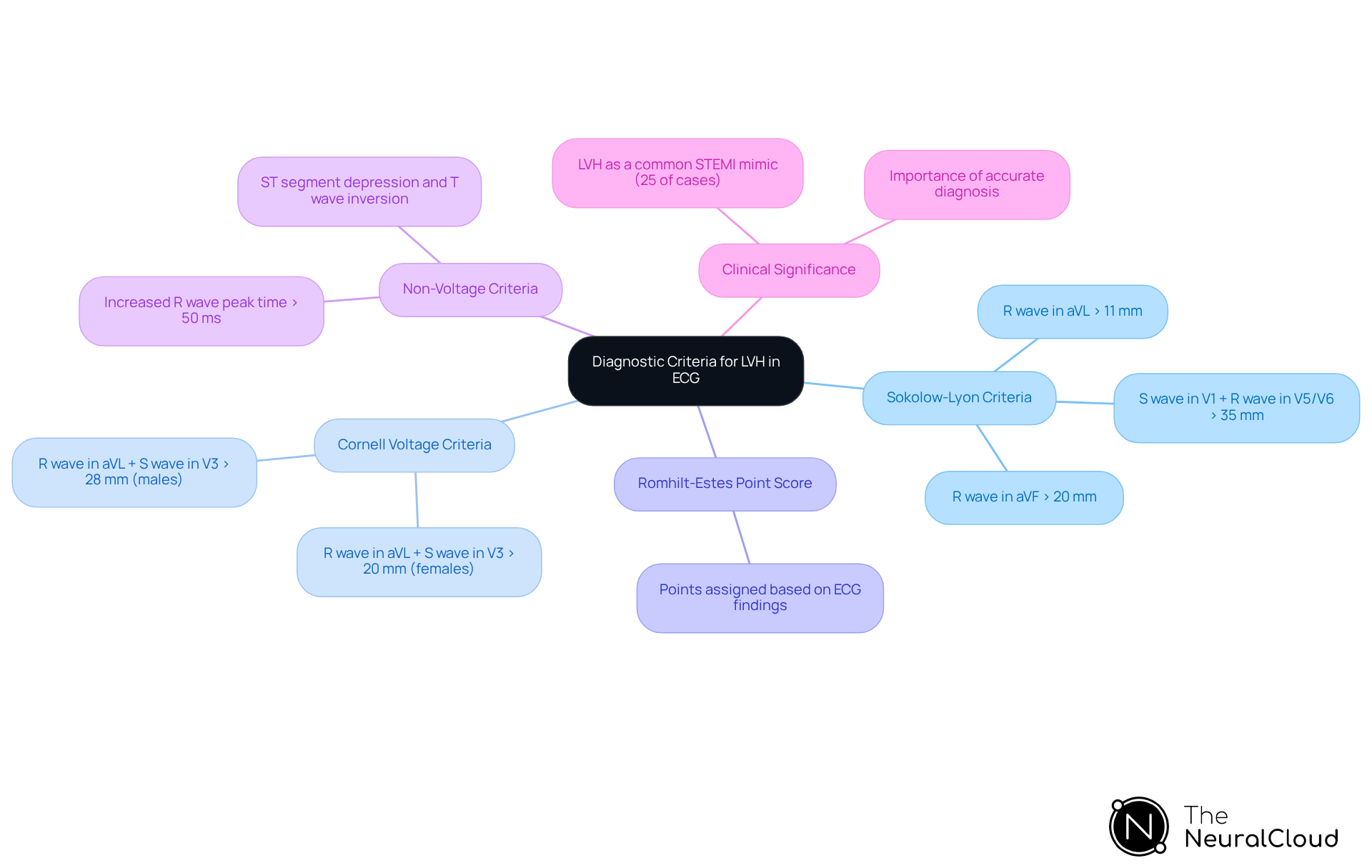
Explore Diagnostic Criteria for LVH in ECG Interpretation
Diagnosing ECG left ventricular hypertrophy (LVH) involves several established criteria, with the Sokolow-Lyon criteria being a cornerstone. According to these criteria, when the sum of the S wave in position V1 and the tallest R wave in position V5 or V6 exceeds 35 mm, it indicates ECG left ventricular hypertrophy (LVH). Additionally, the Cornell voltage criteria state that the total of the R wave in aVL and the S wave in V3 should surpass 28 mm in males and 20 mm in females.
The Romhilt-Estes point score system further aids in diagnosing ECG left ventricular hypertrophy (LVH) by assigning points based on various ECG findings, which enhances diagnostic accuracy. Recent updates for 2025 emphasize the need for clinicians to integrate these criteria with non-voltage indicators, such as increased R wave peak time and ST segment abnormalities, to improve diagnostic sensitivity. It is crucial to note that LVH is the most common STEMI mimic, accounting for 25% of cases, underscoring the importance of accurate diagnosis.
Understanding these criteria is essential for effective ECG interpretation, especially concerning ECG left ventricular hypertrophy, and optimal patient management. This is particularly important in distinguishing LVH from other conditions like myocardial ischemia, which can present similarly on ECG. By mastering these diagnostic tools, healthcare professionals can enhance their clinical decision-making and improve patient outcomes.
Examine Pathophysiology and Causes of Left Ventricular Hypertrophy
ECG left ventricular hypertrophy (LVH) involves an increase in myocardial mass, primarily due to chronic pressure overload from conditions like hypertension and aortic stenosis. This hypertrophy acts as a compensatory mechanism, allowing the heart to maintain adequate cardiac output despite increased workload demands.
Research shows that untreated hypertension has a prevalence of ECG left ventricular hypertrophy ranging from 19% to 48%, which can increase to 58% to 77% in high-risk hypertensive patients. Additionally, conditions causing volume overload, such as mitral regurgitation, along with genetic factors - especially in cases of hypertrophic cardiomyopathy - also play a role in the development of ECG left ventricular hypertrophy.
Understanding these mechanisms is essential for clinicians. It helps identify patients at risk and enables the customization of management strategies to slow the progression of this condition.

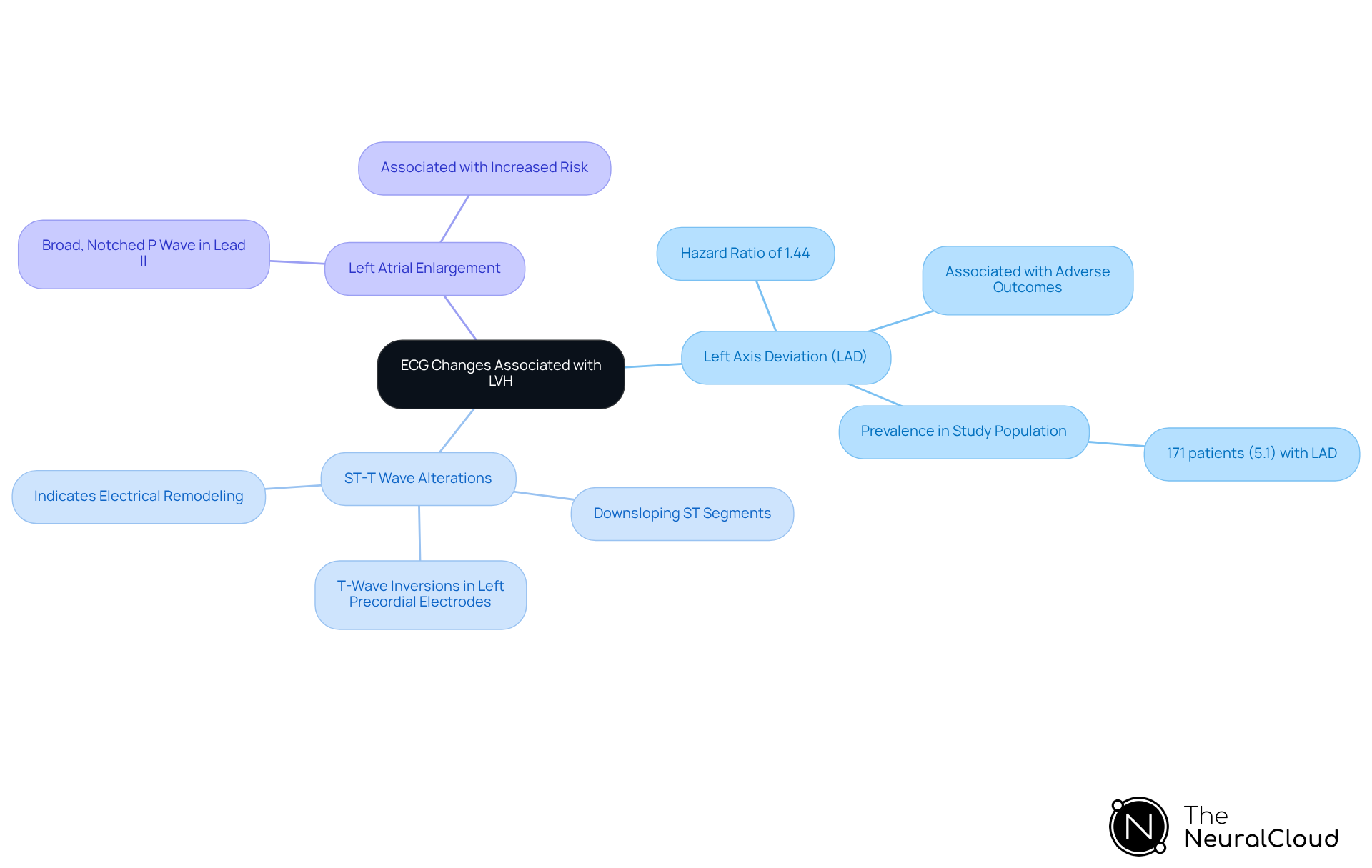
Identify Additional ECG Changes Associated with LVH
In addition to the primary voltage criteria for diagnosing ECG left ventricular hypertrophy (LVH), several significant changes warrant attention. Notably, left axis deviation (LAD) serves as an important indicator, reflecting a shift in the heart's electrical axis often due to increased left ventricular mass. Recent studies indicate that LAD correlates with a higher risk of adverse clinical outcomes, with a hazard ratio of 1.44, underscoring its critical role in diagnosing ECG left ventricular hypertrophy.
Moreover, secondary ST-T wave alterations, such as downsloping ST segments and T-wave inversions in the left precordial electrodes, frequently accompany ECG left ventricular hypertrophy. These changes can signal underlying electrical remodeling and are essential for assessing the patient's cardiac health. Additionally, left atrial enlargement may be suggested by a broad, notched P wave in lead II, further complicating the clinical picture. Recognizing these additional ECG changes, particularly ECG left ventricular hypertrophy, is vital for a comprehensive evaluation of cardiac conditions, as they provide valuable insights into the patient's overall cardiovascular status.
The MaxYield™ platform from Neural Cloud Solutions significantly enhances ECG analysis by automating the process, effectively reducing noise and improving signal clarity. It delivers beat-by-beat analysis, processing 200,000 heartbeats in less than 5 minutes, which aids in the accurate identification of these critical ECG changes. By integrating wearable technology with advanced solutions, health tech developers can streamline the analysis workflow, ensuring that technicians can focus on interpreting complex cases without the burden of manual data labeling.
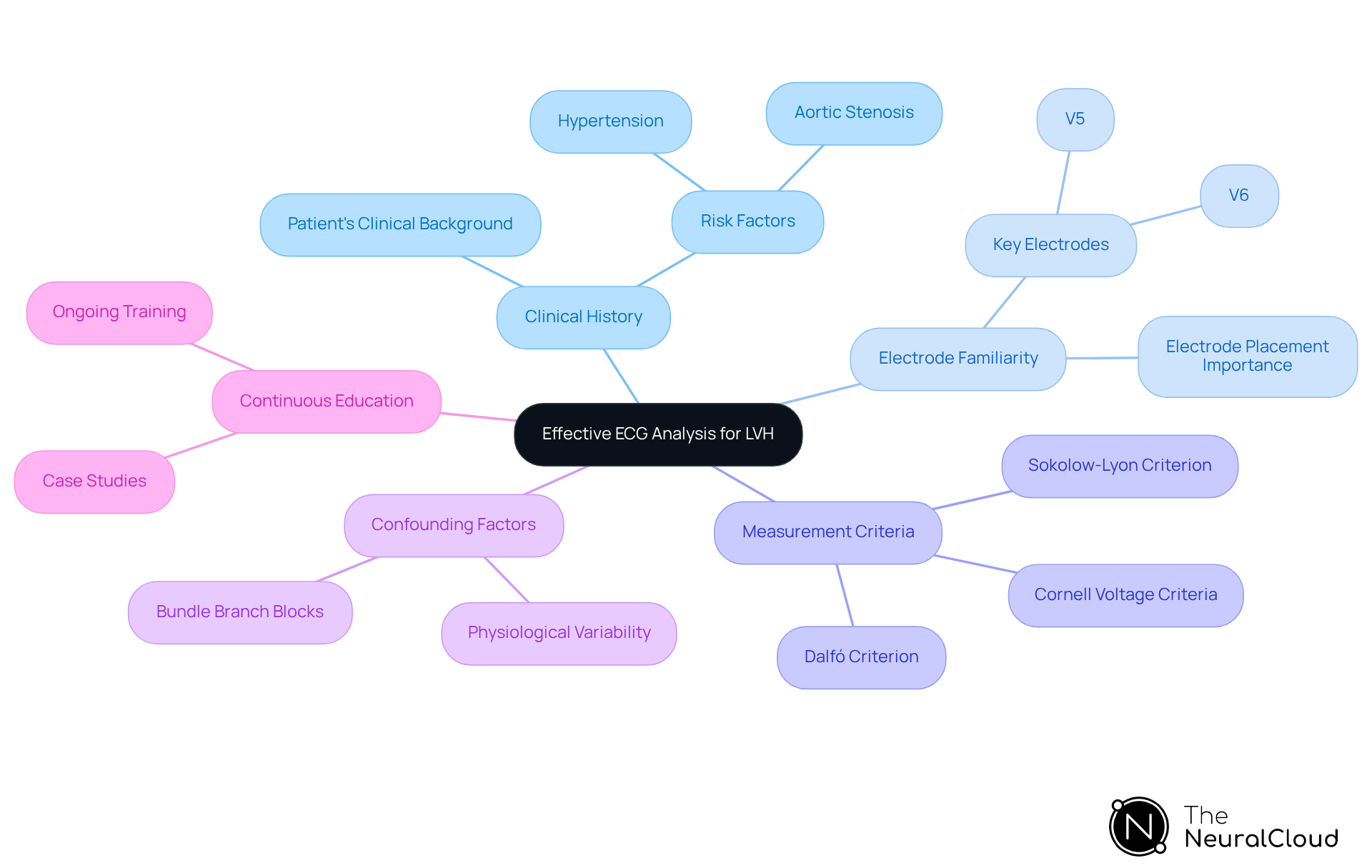
Apply Handy Tips for Effective ECG Analysis of LVH
To optimize ECG analysis for detecting ECG left ventricular hypertrophy, healthcare professionals face several challenges. Understanding the patient's clinical history and risk factors, such as hypertension and aortic stenosis, is crucial for accurate interpretation. The MaxYield™ platform addresses this need by providing AI-driven insights that correlate clinical history with ECG findings, enhancing diagnostic accuracy.
Familiarity with the various ECG electrodes is essential, particularly V5 and V6, which play a pivotal role in diagnosing ECG left ventricular hypertrophy. Changes in these leads can provide significant insights into left ventricular mass. The MaxYield™ platform offers advanced filtering methods that improve the clarity of these leads, facilitating more precise evaluations.
A systematic approach to measuring voltage criteria is vital for ensuring precision in calculations. For instance, the Sokolow-Lyon criterion is used to diagnose ECG left ventricular hypertrophy by requiring the summation of the S wave in V1 and the R wave in V5, with a total exceeding 35 mm indicating LVH. The automated features of the MaxYield™ platform streamline these measurements, reducing the likelihood of human error and enhancing diagnostic reliability.
Healthcare professionals must also be aware of common confounding factors, such as bundle branch blocks, which can obscure the interpretation of ECG left ventricular hypertrophy. Recognizing how these conditions affect ECG readings is essential for accurate diagnosis. The continuous learning model of the MaxYield™ platform aids in identifying and addressing these confounding factors, delivering clearer, filtered ECG signals that improve diagnostic accuracy.
Continuous skill development is key to maintaining proficiency in ECG interpretation. Regularly reviewing and practicing these skills can boost confidence in diagnostic abilities. Engaging with case studies and real-world examples enhances understanding of how clinical history impacts the interpretation of ECG left ventricular hypertrophy. The MaxYield™ platform supports ongoing education by providing access to a library of case studies and examples that illustrate best practices in ECG analysis.
Expert cardiologists emphasize the importance of integrating clinical history into ECG analysis for accurate assessments of conditions such as ECG left ventricular hypertrophy. As one noted, 'The presence of ECG left ventricular hypertrophy plays a crucial role in hypertension management,' highlighting the need for a comprehensive approach to interpreting ECGs. By following these guidelines and leveraging the capabilities of Neural Cloud Solutions' MaxYield™ platform, healthcare professionals can significantly enhance their diagnostic accuracy and improve patient outcomes.
Conclusion
Understanding and mastering ECG left ventricular hypertrophy (LVH) is crucial for healthcare professionals due to its significant implications for cardiovascular health. This article has explored the multifaceted nature of LVH, emphasizing its definition, clinical importance, and the necessity for accurate diagnosis and management. By leveraging advanced technologies and diagnostic criteria, clinicians can enhance their ability to identify and treat this condition effectively.
Key insights presented include:
- The prevalence of LVH in the population
- The critical role of the MaxYield™ platform in improving ECG analysis
- The importance of recognizing additional ECG changes that accompany LVH
The MaxYield™ platform offers features that streamline ECG interpretation, allowing for quicker and more accurate assessments. This improvement in analysis not only aids in diagnosis but also enhances the overall management of patients with LVH.
The diagnostic criteria, such as the Sokolow-Lyon and Romhilt-Estes systems, have been highlighted as essential tools for accurate interpretation. Understanding these criteria is vital for healthcare professionals, as they provide a framework for identifying LVH and its associated risks. The discussion on pathophysiology and contributing factors underscores the need for a comprehensive understanding of the condition, ensuring that clinicians are well-equipped to address it.
Ultimately, recognizing and managing ECG left ventricular hypertrophy can lead to improved patient outcomes and reduced cardiovascular risks. Healthcare professionals are encouraged to integrate their clinical knowledge with advanced diagnostic tools like the MaxYield™ platform and continue their education in ECG interpretation. By doing so, they can play a pivotal role in identifying patients at risk and implementing timely interventions that enhance cardiovascular health and longevity.
Frequently Asked Questions
What is left ventricular hypertrophy (LVH) and why is it clinically important?
Left ventricular hypertrophy (LVH) is characterized by an increase in the size of the myocardial fibers in the left ventricle, the heart's main pumping chamber. It is clinically important as it often indicates underlying conditions such as hypertension or aortic stenosis, which can lead to serious cardiovascular events if untreated.
How prevalent is LVH in the general population?
LVH affects approximately 15% to 20% of the general population, with rates as high as 77% among high-risk hypertensive individuals.
Why is early detection of LVH crucial?
Early detection of LVH is vital as it facilitates timely interventions that can significantly reduce morbidity and mortality associated with heart disease.
What role does the MaxYield™ platform play in ECG analysis for LVH?
The MaxYield™ platform enhances ECG analysis by identifying and labeling critical data, even in recordings with high noise and artifact levels. This allows for the rapid isolation of ECG waves from affected recordings, improving the overall quality of ECG interpretation.
What treatment gap exists for individuals with LVH?
Only 26% of individuals with TTE-LVH are on antihypertensive medications, highlighting a critical treatment gap.
What are the Sokolow-Lyon criteria for diagnosing LVH?
The Sokolow-Lyon criteria indicate that LVH is present when the sum of the S wave in position V1 and the tallest R wave in position V5 or V6 exceeds 35 mm.
What are the Cornell voltage criteria for diagnosing LVH?
According to the Cornell voltage criteria, LVH is indicated when the total of the R wave in aVL and the S wave in V3 surpasses 28 mm in males and 20 mm in females.
How does the Romhilt-Estes point score system assist in diagnosing LVH?
The Romhilt-Estes point score system aids in diagnosing LVH by assigning points based on various ECG findings, enhancing diagnostic accuracy.
What recent updates emphasize the diagnosis of LVH?
Recent updates for 2025 emphasize the need for clinicians to integrate established criteria with non-voltage indicators, such as increased R wave peak time and ST segment abnormalities, to improve diagnostic sensitivity.
Why is accurate diagnosis of LVH important?
Accurate diagnosis of LVH is critical because it is the most common STEMI mimic, accounting for 25% of cases. Understanding and distinguishing LVH from other conditions like myocardial ischemia is essential for effective patient management.






