Introduction
Accurate cardiac analysis relies heavily on the precise placement of electrodes within the 12-lead ECG system, a vital tool for diagnosing heart conditions. Understanding the intricacies of this system allows healthcare professionals to gain valuable insights into a patient's cardiac health, ultimately leading to improved outcomes. However, studies indicate that a notable percentage of ECGs suffer from placement errors. This raises an important question: how can clinicians refine their skills in electrode placement to avoid diagnostic errors and utilize advanced technologies for greater accuracy?
The MaxYield™ platform addresses these challenges by offering features designed to enhance ECG analysis. By providing real-time feedback on electrode placement, it helps clinicians ensure accuracy from the outset. This not only minimizes the risk of errors but also streamlines the diagnostic process, allowing for quicker and more reliable assessments.
The advantages of using MaxYield™ are clear. Healthcare professionals can expect improved diagnostic accuracy, which translates to better patient outcomes. With the platform's user-friendly interface, both technical and non-technical users can navigate the system with ease, making it an invaluable tool in any clinical setting.
In summary, mastering electrode placement is crucial for effective cardiac analysis. By leveraging the capabilities of the MaxYield™ platform, clinicians can enhance their diagnostic precision, ultimately benefiting their patients.
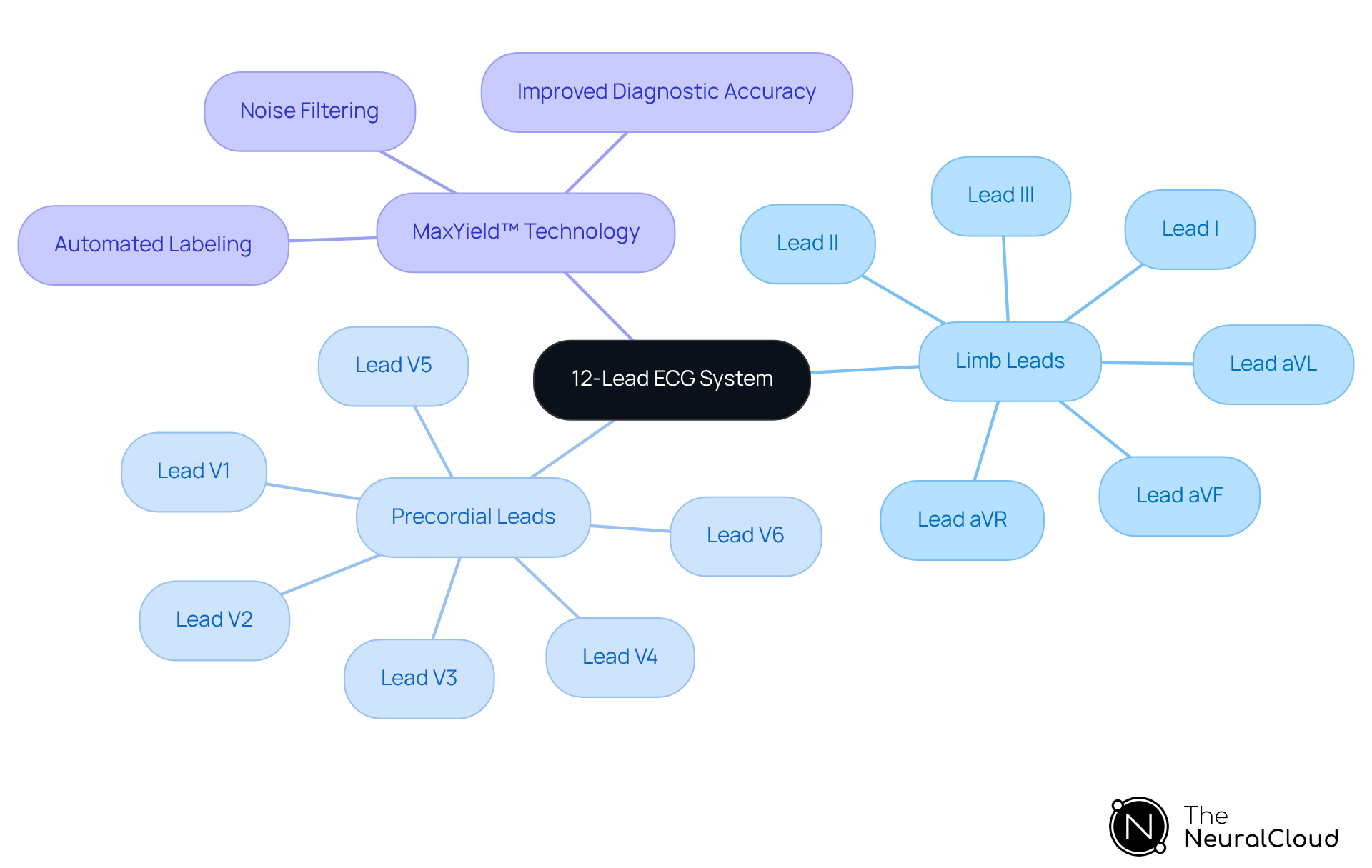
Understand the 12-Lead ECG System
The 12-lead ECG system employs 10 sensors strategically placed on the body to generate 12 distinct views of the heart's electrical activity, crucial for diagnosing various cardiac conditions. These leads are categorized into limb leads (I, II, III, aVR, aVL, aVF) and precordial leads (V1 to V6). Each lead provides a unique perspective, allowing healthcare professionals to detect abnormalities such as arrhythmias, ischemia, and other cardiac issues. Understanding how to place 12 lead ECG is essential, as accurate electrode placement is crucial; even minor deviations can significantly impact the quality of ECG readings and the reliability of diagnoses.
The MaxYield™ platform enhances ECG analysis efficiency by utilizing advanced noise filtering and automated labeling. This technology effectively addresses challenges like physiological variability and signal artifacts, ensuring that healthcare professionals can achieve clear interpretations and actionable insights, even with varying recordings. For example, case studies indicate that facilities using this platform have improved diagnostic accuracy and reduced report turnaround times, showcasing its effectiveness in real-world scenarios. As cardiologists stress, the accuracy of lead placement, combined with the capabilities of MaxYield™, can mean the difference between a correct diagnosis and a missed opportunity for timely intervention. This underscores the necessity of ongoing training and adherence to best practices in how to place 12 lead ECG for optimal performance.
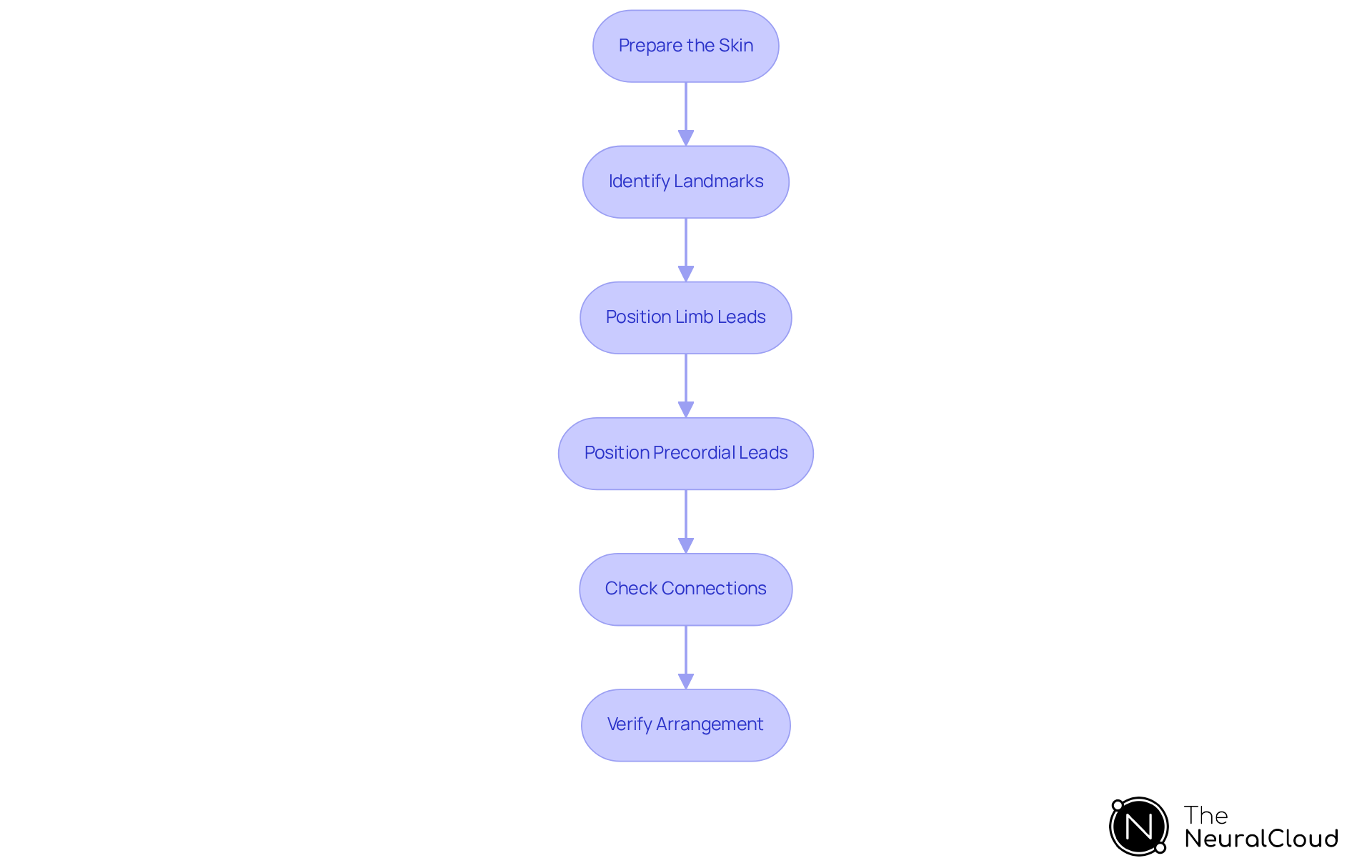
Execute Proper Electrode Placement Techniques
To achieve accurate electrode placement for a 12-lead ECG, follow these essential steps:
- Prepare the Skin: Clean the skin at contact points with alcohol wipes to remove oils and dirt, ensuring optimal adhesion and signal quality. Fresh conductive gel or adhesive pads are crucial for enhancing signal fidelity.
- Identify Landmarks: Locate anatomical landmarks for each lead accurately. For example, V1 should be positioned in the 4th intercostal space at the right sternal border, while V2 is placed in the 4th intercostal space at the left sternal border.
- Position Limb Leads: Connect the limb leads (RA, LA, RL, LL) to the appropriate limbs, ensuring symmetry and avoiding placement over large muscle masses to minimize artifacts.
- Position Precordial Leads: Place the precordial leads (V3, V4, V5, V6) in their designated positions. For instance, V4 should be positioned at the 5th intercostal space along the mid-clavicular line.
- Check Connections: Confirm that all terminals are securely attached and that connections to the ECG machine are intact to prevent signal loss or distortion during recording.
- Verify Arrangement: Before starting the ECG, double-check the positioning of all sensors against a standard arrangement guide to ensure accuracy. It is essential to understand how to place 12 lead ECG correctly by recording any variations from standard lead positioning, as this preserves the accuracy of ECG interpretations.
The importance of adhering to established guidelines is underscored by the fact that improper placement of sensors, including how to place 12 lead ecg, can lead to significant diagnostic errors. For instance, a study revealed that only 5.8% of participants accurately placed all chest electrodes, highlighting the critical need for proper training and adherence to anatomical landmarks. Healthcare professionals emphasize that meticulous skin preparation is foundational for achieving reliable ECG results, as it directly impacts the quality of the recorded signals.
With the integration of Neural Cloud Solutions' platform, which excels in noise filtering and distinct wave recognition, clinicians can salvage previously obscured sections of lengthy recordings. This ensures that even in challenging conditions, the diagnostic yield is maximized. As noted by Intco Medical, "Electrode placement is not a trivial detail - it is the foundation upon which ECG accuracy rests." By following these techniques and leveraging advanced technologies like MaxYield™, clinicians can enhance the accuracy of their ECG interpretations and improve patient outcomes.
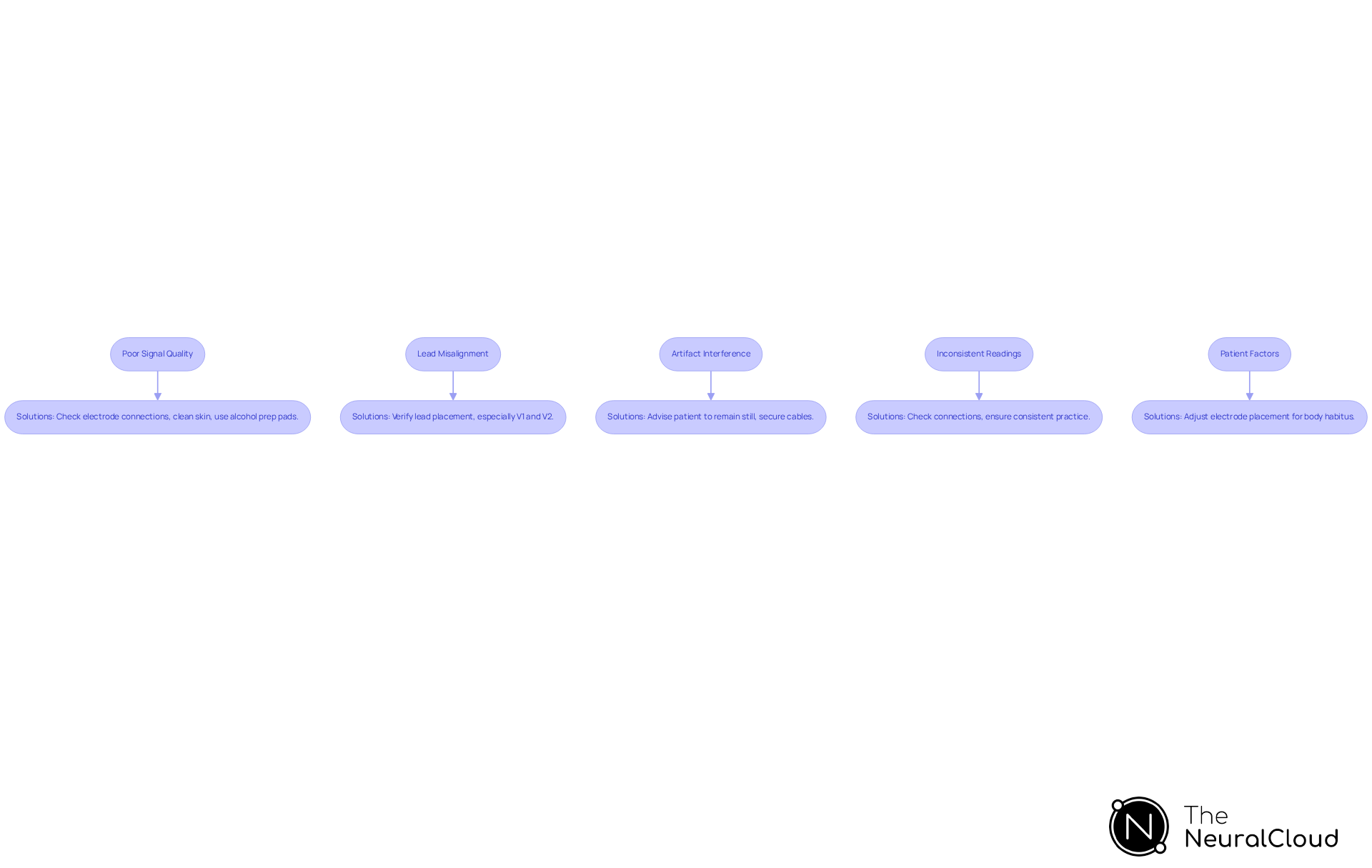
Troubleshoot Common ECG Placement Issues
When performing a 12-lead ECG, several common issues can arise that significantly impact the accuracy of cardiac analysis:
-
Poor Signal Quality: An unclear ECG tracing or excessive noise can compromise results. First, learn how to place 12 lead ECG by checking the electrode connections to ensure they are securely attached. The skin must be clean and free of oils; using alcohol prep pads can enhance adhesion and signal quality. Research indicates that 30-50% of ECGs contain at least one significant positioning error, often due to insufficient skin preparation when understanding how to place 12 lead ecg. Additionally, 30-50% of substandard MIs engage the right ventricle, underscoring the importance of accurate positioning in clinical situations. The MaxYield™ platform from Neural Cloud Solutions addresses this challenge with advanced noise filtering and highlighting of P, QRS, and T Waves, ensuring a clean, "neuralized" signal that enhances the clarity of the ECG tracing.
-
Lead Misalignment: Abnormal readings may suggest incorrect electrode positioning. Misplacement of leads, particularly V1 and V2, is common, highlighting the need for understanding how to place 12 lead ECG correctly, as less than 20% of cardiologists do it accurately. A mere 2 cm error in V1-V2 placement can create ST elevations that mimic anterior STEMI, which underscores the importance of learning how to place 12 lead ECG to prevent unnecessary interventions. As noted by Maggie Berkey, understanding how to place 12 lead ecg is critical, as factors like dry skin and body hair can affect connectivity. The MaxYield™ platform streamlines this process by consolidating workflow and providing clear, beat-by-beat data, reducing the likelihood of misplacement.
-
Artifact Interference: Muscle movement or electrical interference can introduce artifacts into the ECG. Advise the patient to remain still during the recording and ensure that all cables are properly secured and distanced from electrical sources. Regular quality checks can help identify recurring issues related to artifacts. It's also essential to verify how to place 12 lead ECG settings correctly for the patient type and setup, as this can significantly impact signal quality. With MaxYield™, automated signal processing minimizes the impact of artifacts, allowing for more reliable readings.
-
Inconsistent Readings: Significant variations in readings between attempts may indicate loose connections or irregular positioning. Consistency is vital; research shows that more accurate connections relate to classroom training and regular practice. The MaxYield™ platform assists in achieving reliable outcomes by offering a data wall that handles a larger volume of information in a shorter duration, allowing healthcare professionals to focus on precise assignments.
-
Patient Factors: Physiological factors such as body habitus or skin conditions can influence adhesion and signal quality. Adjust electrode placement as necessary to accommodate these factors, ensuring you understand how to place 12 lead ecg for optimal contact. For instance, patients with tremors may require special attention to maintain signal integrity. By utilizing the capabilities of this advanced system, healthcare professionals can better address these patient-specific challenges, enhancing overall ECG performance.
By addressing these common issues with the support of Neural Cloud Solutions' platform, healthcare professionals can enhance the reliability of ECG results, ultimately improving patient care.
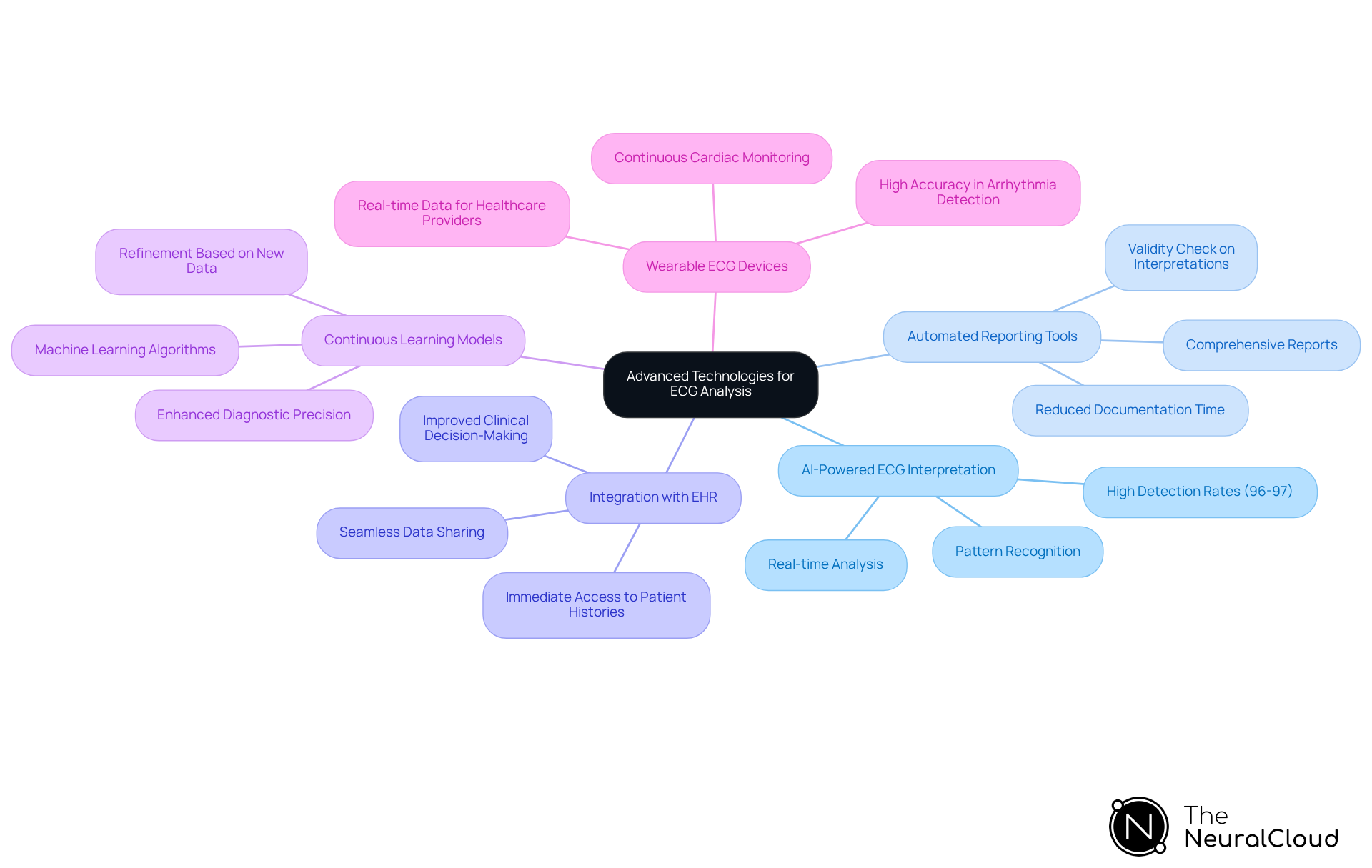
Incorporate Advanced Technology for Enhanced Analysis
To enhance ECG analysis, consider the following advanced technologies:
-
AI-Powered ECG Interpretation: Implement AI algorithms capable of real-time analysis of ECG data, identifying patterns and anomalies that may elude human detection. This approach has been shown to improve diagnostic accuracy significantly, with AI achieving detection rates of 96-97% for irregular heart rhythms, as noted in recent studies.
-
Automated Reporting Tools: Utilize software that automatically generates comprehensive reports based on ECG findings. This automation reduces the time clinicians spend on manual documentation, allowing them to concentrate on patient care and decision-making. As Dr. Thomas Maddox emphasizes, AI tools serve as a valuable validity check on interpretations, enhancing clinical practice.
-
Integration with Electronic Health Records (EHR): Ensure compatibility between ECG systems and EHR platforms to facilitate seamless data sharing. This integration enhances clinical decision-making by providing healthcare professionals with immediate access to patient histories and ECG results, ultimately improving patient outcomes.
-
Continuous Learning Models: Leverage platforms that employ machine learning to refine their algorithms continuously based on new data. This capability enhances the accuracy of ECG interpretations over time, adapting to emerging patterns and improving diagnostic precision.
-
Wearable ECG Devices: Explore the potential of wearable technology for continuous cardiac monitoring. These devices provide real-time data to healthcare providers, enabling proactive management of cardiac conditions and improving patient outcomes. For instance, AI-enhanced wearables can detect arrhythmias with high accuracy, supporting timely interventions. Notably, AI has reduced false-positive results by 98.0% in arrhythmia classification, showcasing its effectiveness.
By incorporating these advanced technologies, healthcare providers can significantly enhance the quality and efficiency of ECG analysis, ultimately leading to better patient care. Given that cardiovascular disease (CVD) is responsible for 17 million annual fatalities worldwide, the importance of accurate ECG analysis cannot be overstated.
Conclusion
Mastering the placement of a 12-lead ECG is crucial for accurate cardiac analysis, providing a comprehensive view of the heart's electrical activity essential for diagnosing various conditions. Proper electrode placement, along with advanced technologies, enables healthcare professionals to interpret ECG readings effectively and make timely interventions.
This article discussed key techniques for achieving accurate electrode placement, emphasizing the importance of skin preparation, anatomical landmarks, and the systematic arrangement of leads. Common issues, such as poor signal quality and lead misalignment, were also addressed, along with solutions to troubleshoot these challenges. The integration of advanced technologies, including AI-powered interpretation and automated reporting tools, enhances ECG analysis and improves patient outcomes.
In conclusion, the importance of accurate 12-lead ECG placement cannot be overstated. By adhering to best practices and leveraging technological advancements, healthcare providers can enhance the reliability of ECG results, ultimately leading to better patient care. Embracing these techniques and innovations is vital for any professional aiming to improve their cardiac assessment capabilities and ensure optimal patient safety and outcomes.
Frequently Asked Questions
What is the purpose of the 12-lead ECG system?
The 12-lead ECG system is used to generate 12 distinct views of the heart's electrical activity, which is crucial for diagnosing various cardiac conditions.
How many sensors are used in the 12-lead ECG system, and where are they placed?
The 12-lead ECG system employs 10 sensors that are strategically placed on the body.
What are the categories of leads in the 12-lead ECG system?
The leads are categorized into limb leads (I, II, III, aVR, aVL, aVF) and precordial leads (V1 to V6).
Why is accurate electrode placement important in a 12-lead ECG?
Accurate electrode placement is crucial because even minor deviations can significantly impact the quality of ECG readings and the reliability of diagnoses.
What challenges does the MaxYield™ platform address in ECG analysis?
The MaxYield™ platform addresses challenges such as physiological variability and signal artifacts through advanced noise filtering and automated labeling.
What benefits have facilities experienced by using the MaxYield™ platform?
Facilities using the MaxYield™ platform have improved diagnostic accuracy and reduced report turnaround times, showcasing its effectiveness in real-world scenarios.
What is the significance of ongoing training in ECG lead placement?
Ongoing training is necessary to ensure adherence to best practices in how to place a 12-lead ECG, which can make the difference between a correct diagnosis and a missed opportunity for timely intervention.






