Introduction
Early detection of hyperacute T-waves in ECG readings presents a significant opportunity for timely diagnosis of acute myocardial ischemia. This is particularly important in scenarios where conventional criteria may not suffice. These distinctive waveforms often act as precursors to more severe conditions, such as STEMI, making it essential for healthcare professionals to grasp their clinical significance.
However, accurately identifying these waves can be challenging due to various diagnostic hurdles. Clinicians must navigate these complexities to enhance their recognition of hyperacute T-waves. By employing targeted strategies, they can improve patient outcomes in emergency situations.
What methods can be implemented to facilitate this recognition and ensure timely intervention?
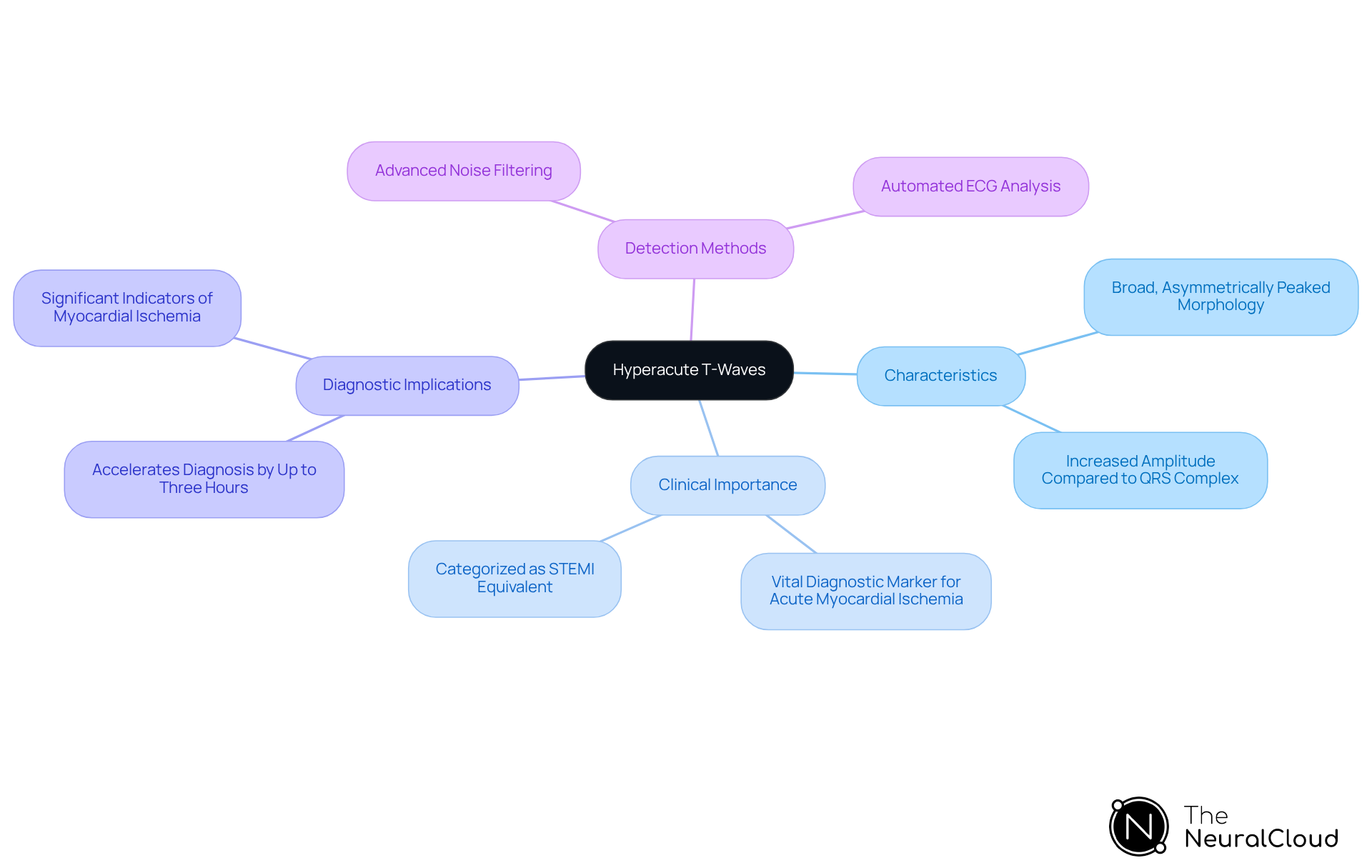
Define Hyperacute T-Waves and Their Clinical Importance
Hyperacute t-waves ECG are characterized by their broad, asymmetrically peaked morphology and increased amplitude compared to the QRS complex. Hyperacute t-waves ECG often emerge in the early stages of ST-elevation myocardial infarction (STEMI), serving as a vital diagnostic marker for acute myocardial ischemia. The ability to quickly identify rapid cardiac wave changes can lead to timely interventions, significantly improving patient outcomes through prompt reperfusion therapy. Their recognition is particularly important in cases where traditional STEMI criteria may not be met, effectively categorizing them as a 'STEMI equivalent' in clinical practice, especially when hyperacute t-waves ECG are present.
According to the American College of Cardiology, early waveforms are essential for diagnosing acute coronary blockage, underscoring their importance for cardiologists and emergency medicine professionals. Recent studies indicate that recognizing the hyperacute t-waves ECG can accelerate diagnosis by up to three hours compared to conventional methods. This is crucial, considering that around 70% of fatal acute myocardial infarction (AMI) cases stem from occlusions caused by atherosclerotic plaques. Furthermore, case studies reveal that hyperacute T-waves on an ECG often precede ST-segment elevation, marking them as significant indicators of myocardial ischemia.
With innovative solutions, cardiologists can leverage advanced noise filtering and automated ECG analysis to enhance the identification of these waves. This ensures early detection, which is vital for the effective management of acute coronary blockage. By strengthening their role in the electrocardiographic evaluation of patients presenting with chest pain, healthcare professionals can significantly improve patient care.
Establish Criteria for Identifying Hyperacute T-Waves
Clinicians face several challenges in ECG analysis to accurately identify hyperacute T-waves ECG. MaxYield™ addresses these challenges by enhancing the analysis process through its advanced features:
- Morphology: Hyperacute waves are characterized by their broad-based and symmetrical appearance. MaxYield™ aids in clearly distinguishing these features by filtering out noise, allowing for more accurate identification.
- Amplitude: These T deflections typically show a significant rise in amplitude compared to the preceding QRS complex, often exceeding the 95th percentile for their height. The advanced noise filtering of MaxYield™ ensures that this increase is accurately captured, providing reliable data for clinicians.
- Lead Localization: The most pronounced hyperacute T-waves ECG are found in the anterior leads (V2-V4), although they may also manifest in inferior leads depending on the ischemic area. MaxYield™ effectively isolates these leads, enhancing diagnostic clarity.
- Comparison with Baseline ECG: Reviewing prior ECGs is essential for detecting new changes in T-wave morphology. This platform facilitates this comparison by providing clearer visualizations of previous recordings, making it easier for clinicians to spot significant changes.
- Associated Changes: Clinicians should also look for accompanying ST-segment depression or elevation, as these changes can further indicate acute myocardial ischemia. MaxYield™'s capabilities in noise reduction support the identification of these critical associated changes.
In clinical practice, identifying extremely sharp waveforms is crucial as they act as early signs of acute ischemia, frequently occurring before ST-segment elevation. By utilizing MaxYield™, healthcare professionals can enhance their diagnostic accuracy and streamline the ECG analysis process, making it more efficient and reliable.

Analyze Diagnostic Challenges and Solutions for Hyperacute T-Waves
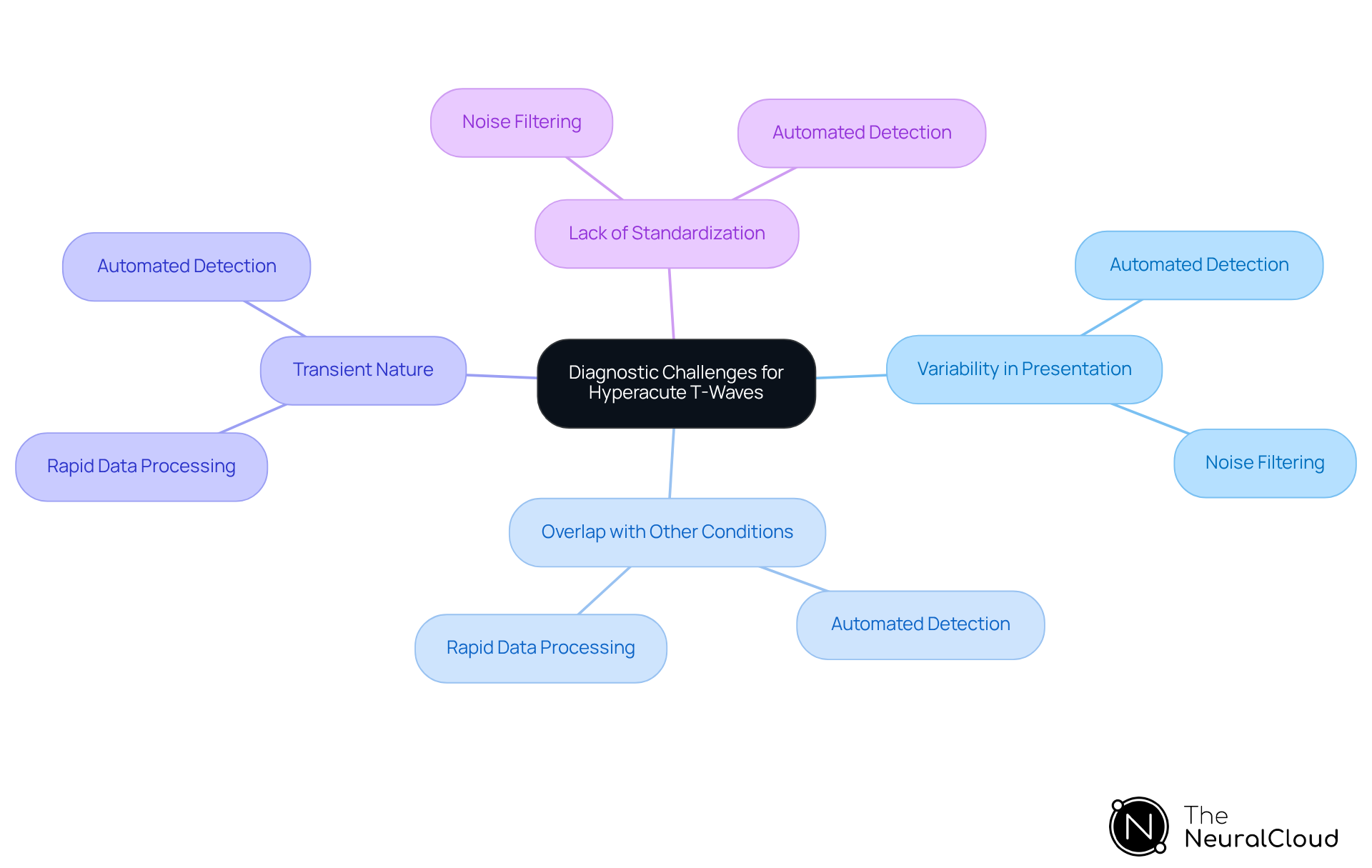
Diagnosing hyperacute T-waves presents several significant challenges:
- Variability in Presentation: Hyperacute waveforms can exhibit considerable differences among patients, complicating their recognition.
- Overlap with Other Conditions: Conditions such as hyperkalemia and early repolarization can closely resemble sharp upward deflections on an electrocardiogram, increasing the risk of misdiagnosis.
- Transient Nature: These cardiac waves may be fleeting, often disappearing as myocardial injury progresses, complicating diagnosis if not captured on the ECG.
- Lack of Standardization: The absence of a universally accepted definition for rapid cardiac waves leads to inconsistent interpretations across clinical environments.
To effectively address these challenges, clinicians can leverage advanced ECG analysis tools like Neural Cloud Solutions' MaxYield™ platform. This innovative platform automates the detection and labeling of hyperacute T-waves ECG, enhancing diagnostic accuracy through its advanced noise filtering and rapid data processing capabilities.
Features of MaxYield™:
- Automated Detection: Quickly identifies hyperacute T-waves, reducing the time needed for manual analysis.
- Noise Filtering: Enhances signal clarity, allowing for more accurate readings.
- Rapid Data Processing: Provides immediate feedback, facilitating timely clinical decisions.
Advantages for Healthcare Professionals:
- Improved Diagnostic Accuracy: By automating detection, the platform minimizes the risk of human error.
- Enhanced Patient Outcomes: Faster diagnosis leads to timely interventions, improving overall patient care.
- Continuous Education: Engaging with tools like MaxYield™ helps clinicians stay updated on the latest assessment standards and methodologies.
Additionally, fostering collaboration within multidisciplinary teams ensures thorough patient evaluations, thereby improving diagnostic outcomes and reducing the prevalence of misdiagnosis.
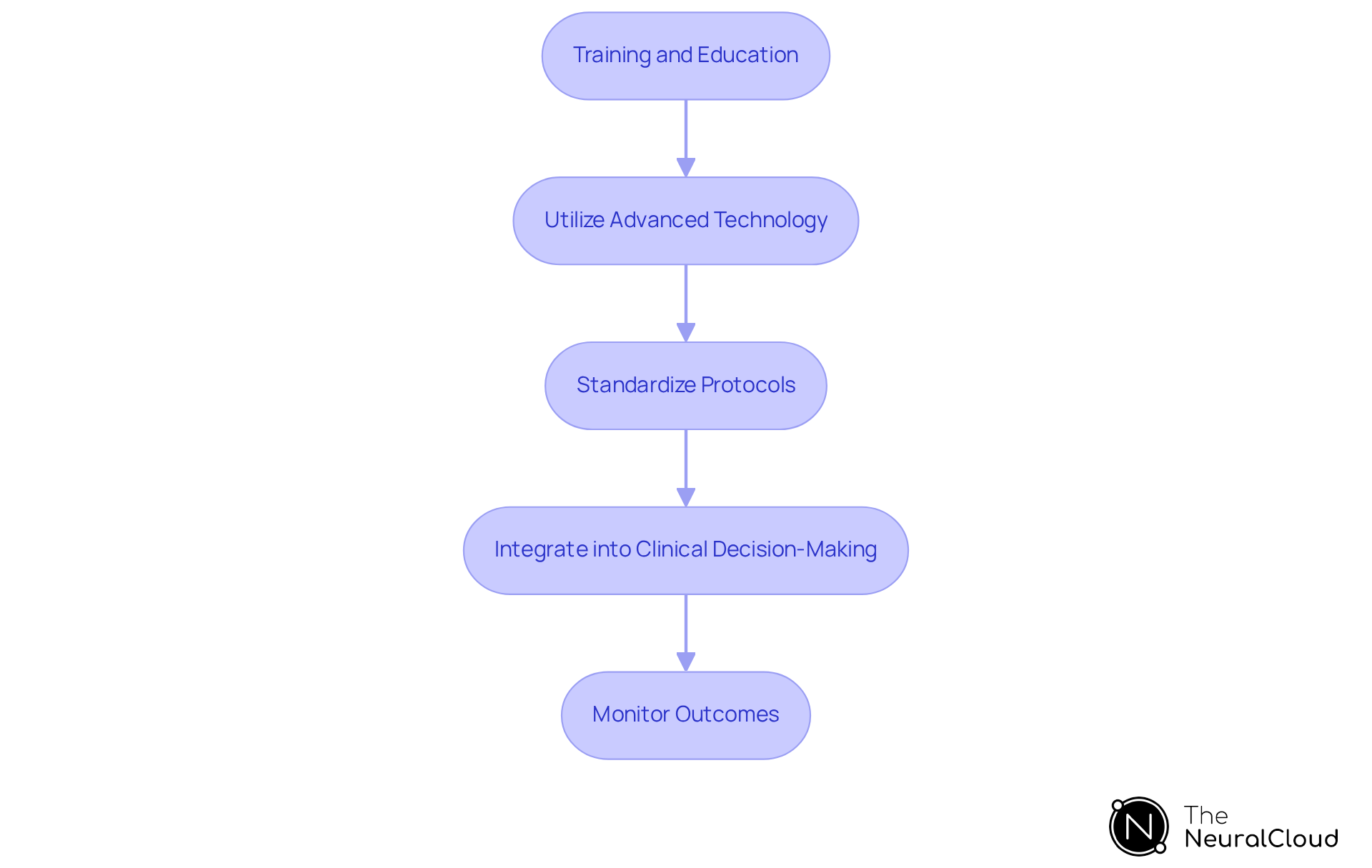
Implement Hyperacute T-Wave Analysis in Clinical Practice
To effectively implement hyperacute T-wave analysis in clinical practice, consider the following steps:
-
Training and Education: All healthcare professionals engaged in ECG analysis must receive thorough instruction on identifying abnormal T morphology and its clinical significance. This training should encompass case studies demonstrating the swift development of acute waves into serious conditions such as ST-segment elevation myocardial infarction (STEMI).
-
Utilize advanced technology by leveraging platforms like MaxYield™ to automate the detection of hyperacute t-waves ECG. This technology reduces the burden of manual analysis and improves evaluation efficiency, enabling clinicians to concentrate on critical decision-making. Notably, leads aVR, V1, and III have shown positive likelihood ratios of 4.3, 2.0, and 3.8, respectively, indicating their diagnostic value. The solution quickly labels P, QRS, and T Wave onsets, offsets, and time-series intervals, allowing users to analyze more data in less time with clear data sets and clean signals. Additionally, MaxYield™ processes data in CSV format for seamless integration into existing workflows.
-
Standardize Protocols: Create and execute uniform protocols for ECG interpretation that include specific guidelines for recognizing prominent T-waves. Consistency across the clinical team is essential for accurate diagnosis and treatment.
-
Integrate into Clinical Decision-Making: Ensure that acute T-wave findings are incorporated into clinical decision-making processes. These findings should be considered alongside other diagnostic information when evaluating patients presenting with chest pain or suspected myocardial ischemia, as they can indicate early cardiac ischemia. As noted by expert Christopher Poyorena, pronounced T waves can represent early cardiac ischemia and may rapidly evolve into classic STEMI findings on ECG.
-
Monitor Outcomes: Regularly review patient outcomes related to hyperacute t-waves ECG diagnoses to evaluate the effectiveness of the implemented protocols. This ongoing assessment will allow for necessary adjustments based on clinical feedback, ultimately improving patient care and outcomes.
Conclusion
Hyperacute T-waves in ECG readings are vital for the early detection of acute myocardial ischemia, especially in ST-elevation myocardial infarction (STEMI). Recognizing these waves can significantly improve diagnostic accuracy and enable timely interventions, ultimately enhancing patient outcomes. For healthcare professionals, understanding the characteristics and clinical significance of hyperacute T-waves is essential for delivering optimal cardiac care.
This article emphasizes the importance of identifying hyperacute T-waves as a 'STEMI equivalent' and outlines the criteria for their recognition, including:
- Morphology
- Amplitude
- Lead localization
However, challenges such as variability in presentation, overlap with other conditions, and the transient nature of these waves can complicate diagnosis. Advanced tools like MaxYield™ address these challenges by automating detection and improving signal clarity, allowing clinicians to make informed decisions swiftly.
Incorporating hyperacute T-wave analysis into clinical practice is crucial for enhancing patient care. By prioritizing training for healthcare professionals, standardizing protocols, and leveraging advanced technology, the healthcare community can boost diagnostic accuracy and improve patient outcomes. Highlighting the significance of hyperacute T-waves not only promotes better clinical practices but also underscores the necessity for ongoing education and collaboration among medical teams.
Frequently Asked Questions
What are hyperacute T-waves in an ECG?
Hyperacute T-waves are characterized by their broad, asymmetrically peaked morphology and increased amplitude compared to the QRS complex. They often appear in the early stages of ST-elevation myocardial infarction (STEMI).
Why are hyperacute T-waves clinically important?
Hyperacute T-waves serve as a vital diagnostic marker for acute myocardial ischemia, allowing for timely interventions that can significantly improve patient outcomes through prompt reperfusion therapy.
How do hyperacute T-waves relate to traditional STEMI criteria?
Hyperacute T-waves can indicate a 'STEMI equivalent' in clinical practice, especially in cases where traditional STEMI criteria may not be met, thus aiding in the diagnosis of acute coronary blockage.
What is the significance of early waveform recognition in diagnosing acute coronary blockage?
Recognizing hyperacute T-waves can accelerate the diagnosis of acute coronary blockage by up to three hours compared to conventional methods, which is crucial given that 70% of fatal acute myocardial infarction cases are caused by atherosclerotic plaque occlusions.
How do hyperacute T-waves relate to ST-segment elevation?
Hyperacute T-waves often precede ST-segment elevation on an ECG, marking them as significant indicators of myocardial ischemia.
What advancements can help in identifying hyperacute T-waves?
Advanced noise filtering and automated ECG analysis can enhance the identification of hyperacute T-waves, ensuring early detection for effective management of acute coronary blockage.
How can recognizing hyperacute T-waves improve patient care?
By strengthening their role in the electrocardiographic evaluation of patients presenting with chest pain, healthcare professionals can significantly improve patient care and outcomes.






