Overview
Junctional bradycardia is characterized by a heart rate of less than 40 beats per minute and originates from the AV junction. This condition can arise from various causes, including:
- Sinoatrial node dysfunction
- Medication effects
- Electrolyte imbalances
Accurate diagnosis is crucial and can be achieved through:
- ECG
- Thorough patient history
Tailored management strategies should be based on:
- Symptom severity
- Underlying conditions
Notably, many causes of junctional bradycardia are reversible, which can lead to significantly improved patient outcomes.
Introduction
Junctional bradycardia is a condition marked by an unusually slow heart rate that originates from the atrioventricular junction. This condition presents significant clinical challenges and implications for healthcare professionals. Understanding its causes, diagnosis, and management is crucial, as early recognition can greatly impact patient outcomes.
Clinicians can implement various strategies to effectively address junctional bradycardia, especially in patients with diverse underlying conditions. This article explores the complexities of junctional bradycardia, providing insights into its etiology, diagnostic methods, and tailored management approaches.
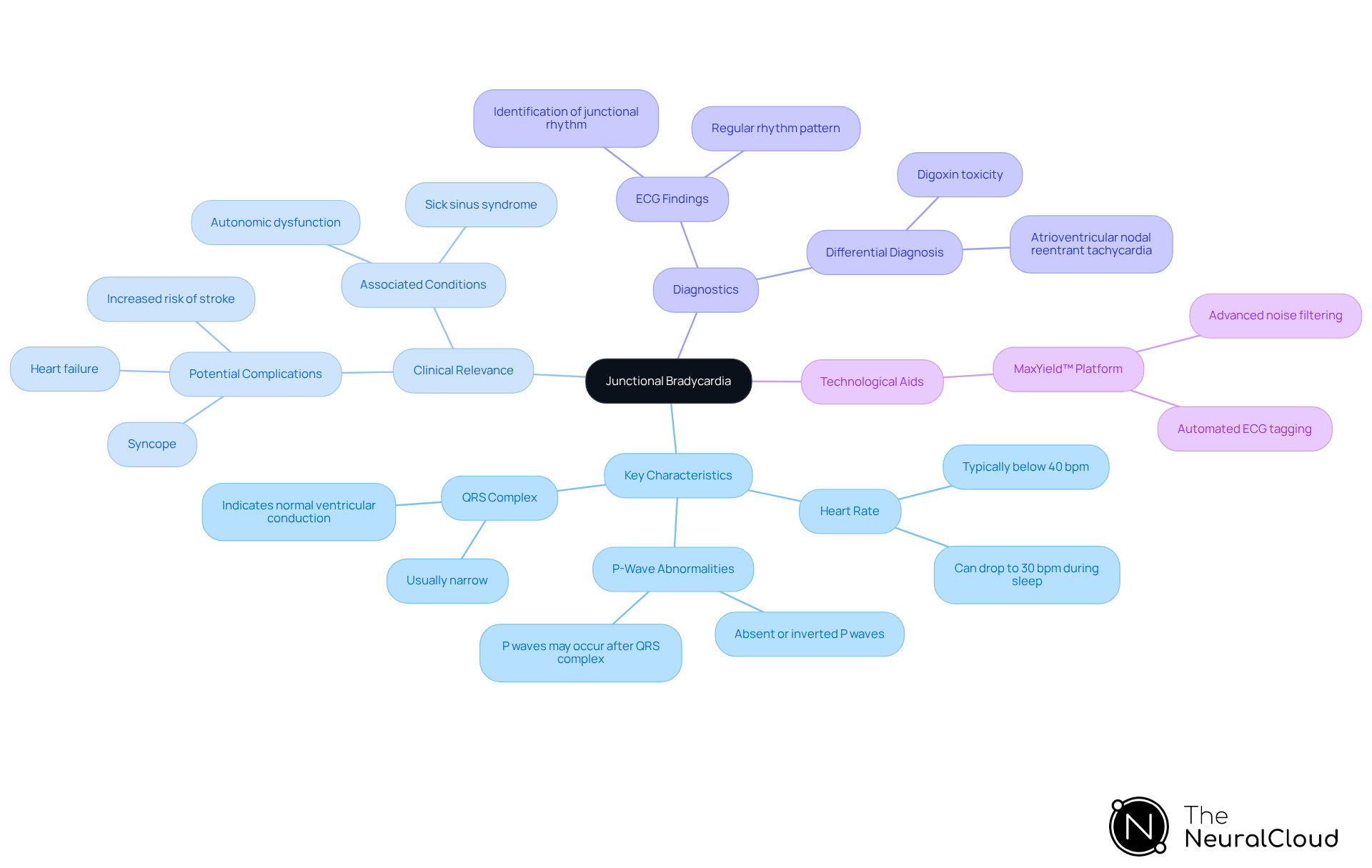
Define Junctional Bradycardia: Key Characteristics and Clinical Relevance
Junctional bradycardia is defined as a heart beat pattern that originates from the atrioventricular (AV) junction and is characterized by a heart rate of less than 40 beats per minute (bpm). Junctional bradycardia occurs when the sinoatrial (SA) node fails to initiate an impulse, resulting in the AV node acting as a backup pacemaker. Key characteristics include:
- Heart Rate: Typically below 40 bpm, with instances where it can drop as low as 30 bpm, particularly during sleep.
- P-Wave Abnormalities: P-waves may be absent, inverted, or occur after the QRS complex, indicating that the rhythm's origin is junctional bradycardia.
- QRS Complex: Usually narrow, suggesting that the impulse is conducted normally through the ventricles, even in the context of junctional bradycardia.
Clinically, junctional bradycardia, a type of slow heart rate, holds significant implications, as it may signal underlying cardiac issues, such as sick sinus syndrome or autonomic dysfunction. Recent studies suggest that junctional bradycardia can occur in various groups, including healthy individuals and athletes, frequently without symptoms. However, it may also lead to complications such as syncope, heart failure, or junctional bradycardia, along with an increased risk of stroke, especially in those with additional risk factors. For instance, research indicated that junctional bradycardia was observed in 14.3% of individuals with acute myocardial infarction (AMI), emphasizing the necessity for vigilant observation and management in these cases.
Recognizing junctional bradycardia on telemetry is crucial, as early identification can facilitate timely interventions and improve patient outcomes. The integration of Neural Cloud Solutions' MaxYield™ platform enhances this process by utilizing and wave recognition, which allows for more accurate ECG analysis even in challenging conditions. Specifically, MaxYield™ assists in recognizing heart rate slowing at connections by offering clear signal analysis and automated tagging. This simplifies workflows and reduces operational expenses. Additionally, educating at-risk patients and ensuring effective communication with the healthcare team are essential for optimizing management.
The differential diagnosis of heart rate slowing, including junctional bradycardia, encompasses conditions like digoxin toxicity and atrioventricular nodal reentrant tachycardia, which should be considered during evaluation. Identifying the underlying etiology of junctional bradycardia before establishing a management plan is vital for effective treatment strategies.
Explore Etiology: Causes and Risk Factors of Junctional Bradycardia
Junctional bradycardia can arise from several underlying factors, each contributing to the disruption of normal cardiac patterns. The key factors include:
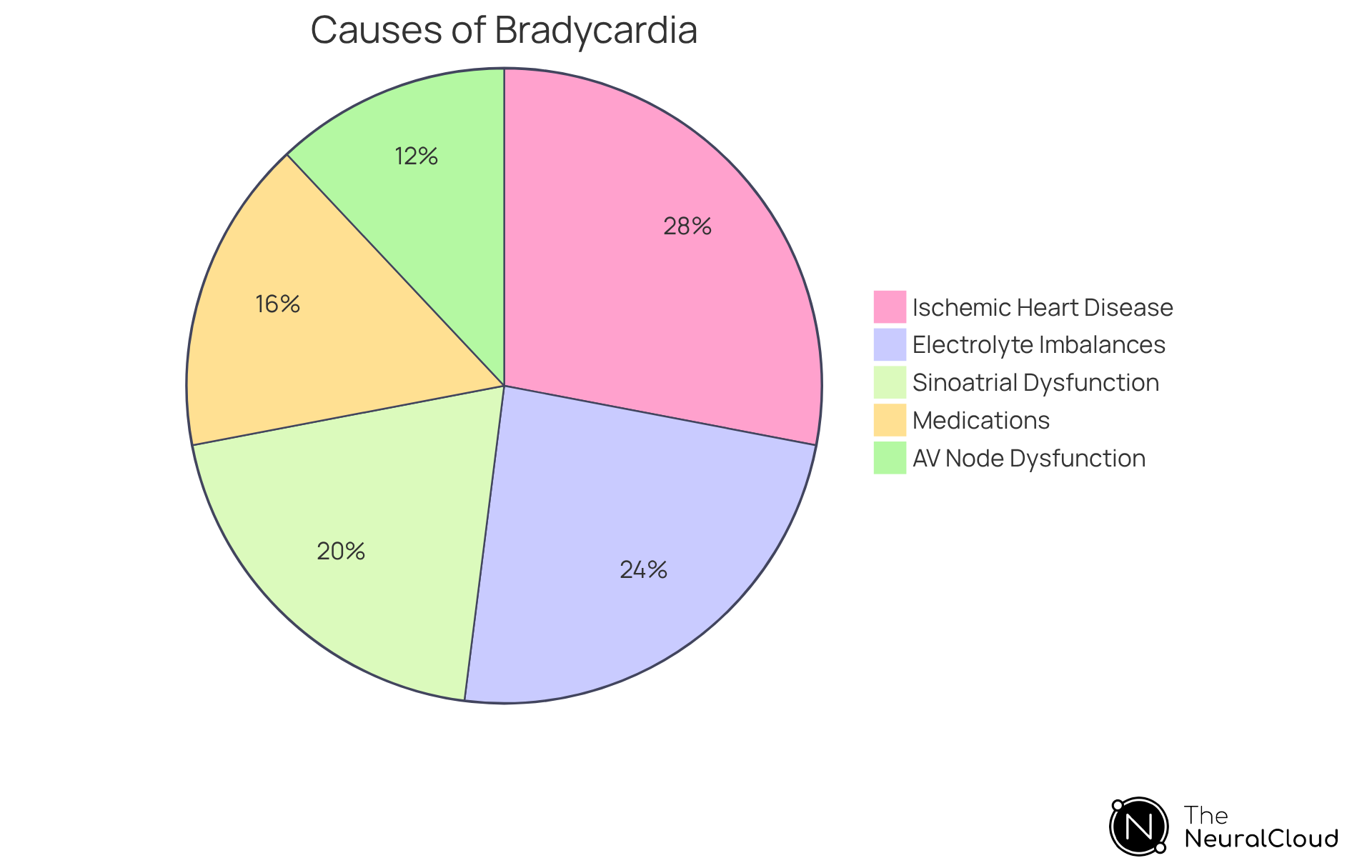
- Sinoatrial Node Dysfunction: Conditions like sick sinus syndrome significantly contribute to decreased impulse formation. This dysfunction is prevalent among individuals with slow heart rates, with research indicating it accounts for about 20% of connection pattern occurrences.
- AV Node Dysfunction: High-grade AV block can result in escape beats, where the heart depends on the connecting tissue for pacing.
- Medications: Certain drugs, including beta-blockers, calcium channel blockers, and digoxin, are known to induce bradycardia, particularly in individuals with pre-existing conditions. Notably, the use of pharmaceutical drugs has been identified as the cause of a specific heart pattern in 16% of individuals.
- Electrolyte Imbalances: Abnormal levels of potassium or calcium can severely impact cardiac conduction, with hyperkalemia recognized in 24% of individuals presenting with specific patterns.
- Ischemic Heart Disease: Reduced blood supply to the heart can disrupt electrical conduction, leading to the formation of connection patterns. In fact, coronary artery disease (CAD) has been found to be the underlying etiology in 28% of individuals with junctional bradycardia.
- Increased Vagal Tone: Situations such as sleep or relaxation can enhance vagal tone, resulting in a slower heart rate. This physiological response is often observed in individuals with a heart rate dropping to 25-35 beats per minute while remaining asymptomatic.
Understanding these elements is crucial for healthcare providers, as many underlying reasons for this type of slow heart rate are . By identifying these conditions, healthcare providers can tailor appropriate interventions, ultimately improving patient outcomes.
Evaluate Junctional Bradycardia: Diagnostic Approaches and Tools
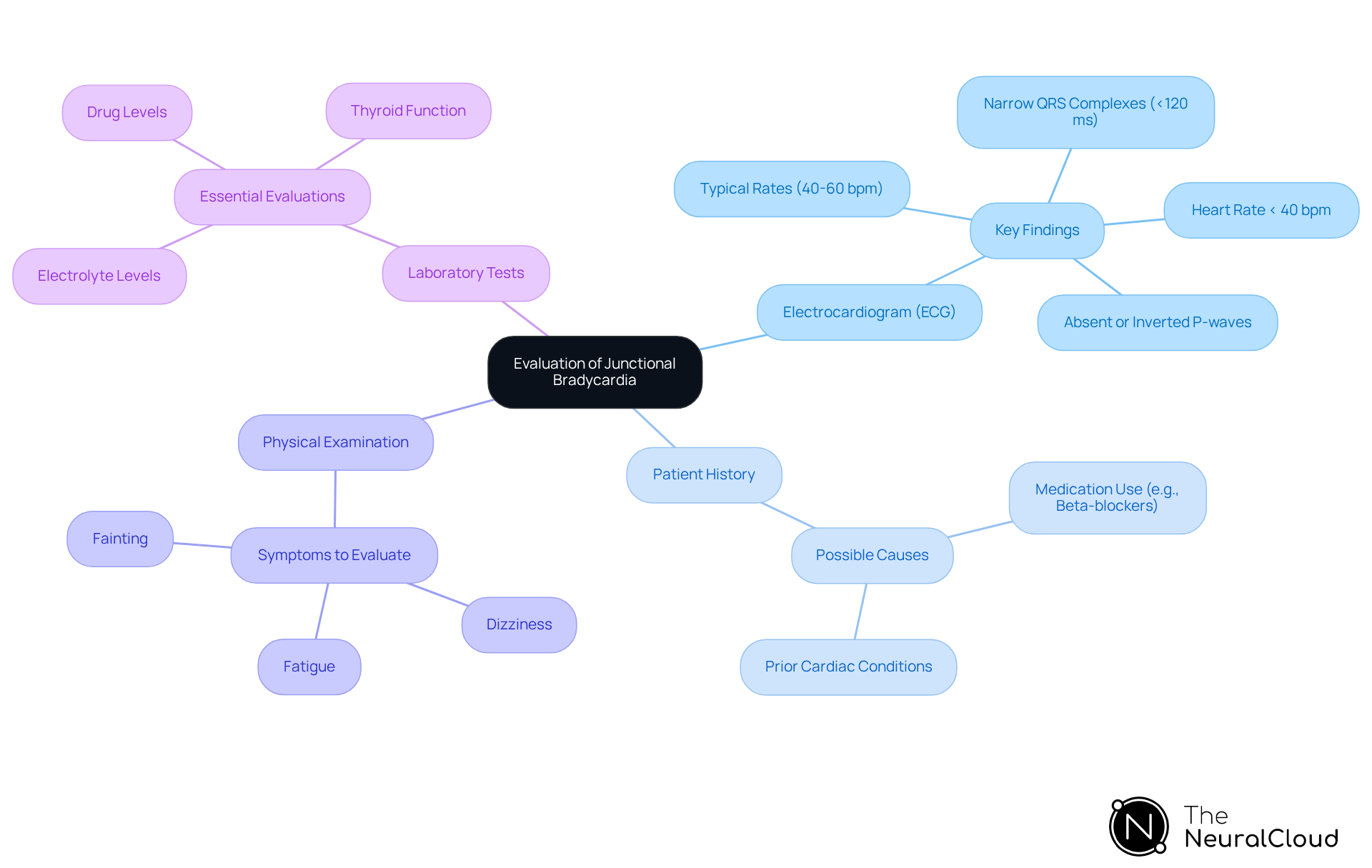
The evaluation of includes several key diagnostic approaches.
- Electrocardiogram (ECG): A 12-lead ECG is essential for the diagnosis of junctional bradycardia. Key findings include absent or inverted P-waves, which may indicate retrograde conduction, narrow QRS complexes typically less than 120 milliseconds, and a heart rate often below 40 bpm, with junctional bradycardia presenting rates that can vary from 40 to 60 bpm.
- Patient History: A comprehensive patient history can reveal possible causes, such as medication use (e.g., beta-blockers) or prior cardiac conditions that may lead to a slow heart rate.
- Physical Examination: Evaluating for indications such as dizziness, fatigue, or fainting offers context for the slow heart rate and aids in determining its severity.
- Laboratory Tests: Evaluating electrolyte levels, thyroid function, and drug levels is essential to identify reversible causes of slow heart rate, such as hyperkalemia or hypothyroidism.
Employing these diagnostic tools effectively allows clinicians to verify the diagnosis of a specific heart rhythm disorder and comprehend its underlying causes, aiding in suitable management strategies.
Manage Junctional Bradycardia: Treatment Strategies and Clinical Guidelines
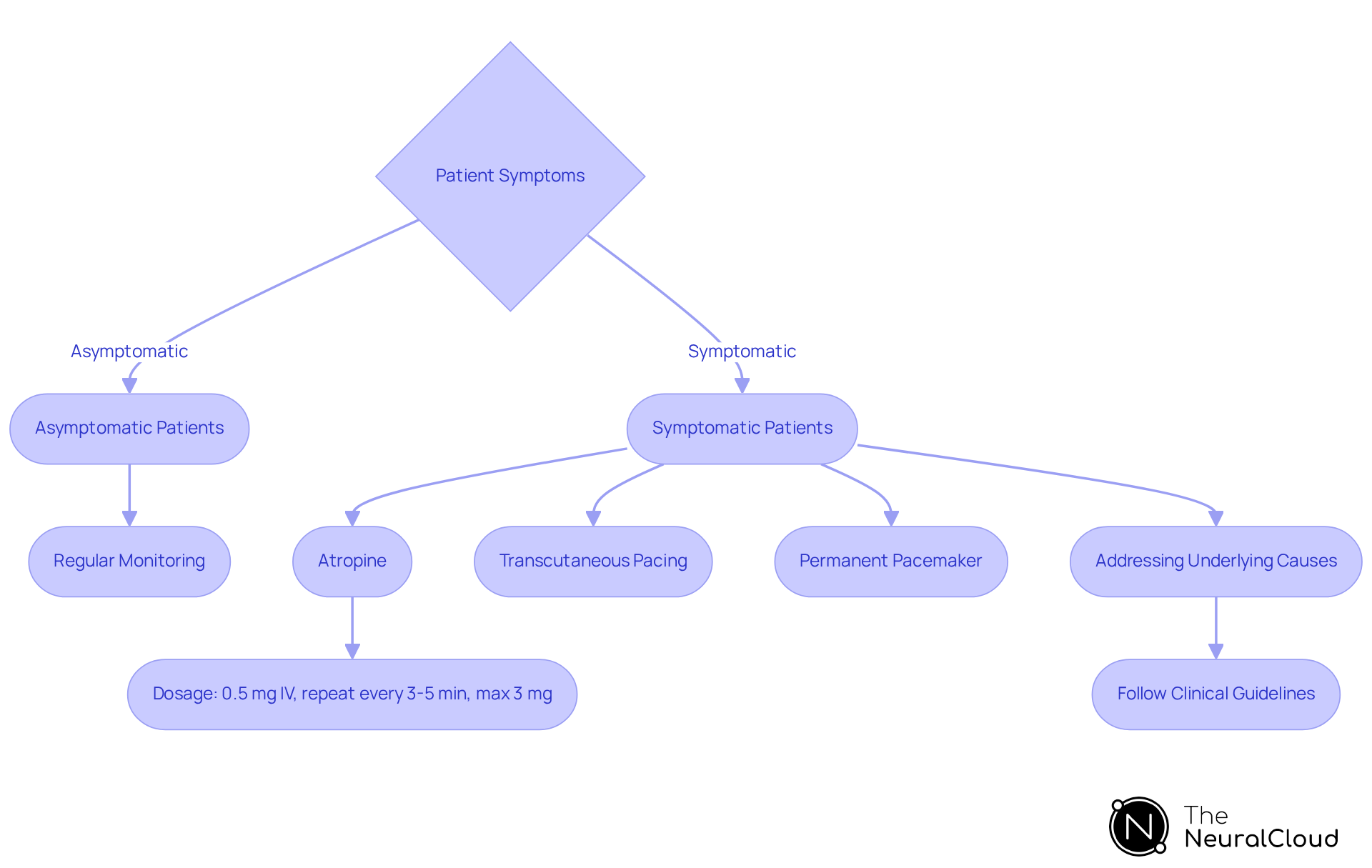
The management of junctional bradycardia is customized based on the patient's symptoms and underlying causes.
Asymptomatic Patients: Typically do not require immediate treatment; regular monitoring is often sufficient.
Symptomatic Patients: Treatment options include:
- Atropine: Administer 0.5 mg IV for symptomatic bradycardia, with the option to repeat every 3-5 minutes as needed, up to a maximum of 3 mg. Atropine has shown effectiveness in improving heart rate in many cases of symptomatic bradycardia, particularly when rapid intervention is necessary.
- Transcutaneous Pacing: This should be considered if the individual is unstable or if atropine fails to achieve the desired effect.
- Permanent Pacemaker: Recommended for individuals experiencing ongoing symptomatic slow heart rate or significant junctional bradycardia, ensuring effective long-term management of heart rhythm.
Addressing Underlying Causes: Identifying and treating reversible factors, such as adjusting medications or correcting electrolyte imbalances, is crucial for effective management. For instance, in situations where bradycardia is worsened by medication side effects, a thorough review and adjustment can significantly enhance outcomes for individuals.
Following established clinical guidelines, such as those from the American College of Cardiology (ACC) and the American Heart Association (AHA), ensures that treatment strategies align with best practices in cardiology. These guidelines emphasize the importance of and the need for ongoing assessment to adapt treatment plans as necessary.
Conclusion
Junctional bradycardia represents a critical aspect of cardiac health, characterized by a heart rate below 40 beats per minute due to the failure of the sinoatrial node and reliance on the AV junction as a pacemaker. Understanding its clinical implications is essential, as it can indicate serious underlying conditions and may lead to significant complications if not appropriately managed.
The multifaceted nature of junctional bradycardia includes key characteristics and potential causes, such as:
- Sinoatrial node dysfunction
- Medication effects
- Electrolyte imbalances
Accurate diagnosis is crucial and can be achieved through tools like ECG and patient history. Management strategies are tailored to individual patient needs, focusing on symptomatology and underlying causes, ensuring that both asymptomatic and symptomatic patients receive the appropriate level of care.
Awareness and understanding of junctional bradycardia are vital for healthcare professionals. By recognizing the signs, employing effective diagnostic methods, and implementing tailored management strategies, patient outcomes can be significantly improved. Continuous education and adherence to clinical guidelines will empower practitioners to navigate the complexities of junctional bradycardia, ultimately enhancing cardiac care and patient safety.
Frequently Asked Questions
What is junctional bradycardia?
Junctional bradycardia is a heart beat pattern that originates from the atrioventricular (AV) junction and is characterized by a heart rate of less than 40 beats per minute (bpm).
What causes junctional bradycardia?
Junctional bradycardia occurs when the sinoatrial (SA) node fails to initiate an impulse, leading the AV node to act as a backup pacemaker.
What are the key characteristics of junctional bradycardia?
Key characteristics include a heart rate typically below 40 bpm (sometimes dropping to 30 bpm during sleep), P-wave abnormalities (which may be absent, inverted, or occur after the QRS complex), and a usually narrow QRS complex indicating normal conduction through the ventricles.
What are the clinical implications of junctional bradycardia?
Junctional bradycardia can signal underlying cardiac issues, such as sick sinus syndrome or autonomic dysfunction, and may lead to complications like syncope, heart failure, or an increased risk of stroke, especially in individuals with additional risk factors.
In which populations can junctional bradycardia occur?
Junctional bradycardia can occur in various groups, including healthy individuals and athletes, often without symptoms.
How is junctional bradycardia recognized and managed?
Recognizing junctional bradycardia on telemetry is crucial for timely interventions. Tools like Neural Cloud Solutions' MaxYield™ platform enhance ECG analysis by using advanced noise filtering and wave recognition.
What is the significance of early identification of junctional bradycardia?
Early identification of junctional bradycardia can facilitate timely interventions and improve patient outcomes.
What should be considered in the differential diagnosis of heart rate slowing?
Conditions such as digoxin toxicity and atrioventricular nodal reentrant tachycardia should be considered during the evaluation of heart rate slowing, including junctional bradycardia.
Why is it important to identify the underlying etiology of junctional bradycardia?
Identifying the underlying etiology is vital for establishing an effective management plan and treatment strategies.


