Overview
The article serves as a comprehensive guide for analyzing junctional rhythm strips, detailing their definitions, types, key ECG features, and a systematic analysis process. It highlights the critical importance of accurately identifying junctional rhythms through a structured approach. Additionally, it addresses common troubleshooting issues, supported by clinical observations and advanced tools such as MaxYield™, which enhance effective ECG interpretation for healthcare professionals.
Introduction
Understanding the intricacies of junctional rhythms is essential for any healthcare professional involved in cardiac monitoring. These rhythms, originating from the atrioventricular junction, play a crucial role when the primary pacemaker, the sinoatrial node, fails. This article provides a comprehensive step-by-step guide to mastering the analysis of junctional rhythm strips. It equips readers with the knowledge to identify key ECG features and troubleshoot common issues. However, given the various types of junctional rhythms and their subtle differences, ensuring accurate interpretation in a fast-paced clinical environment poses a significant challenge.
Understand Junctional Rhythms: Definition and Types
Junctional patterns represent cardiac rhythms that originate from the atrioventricular (AV) junction, situated between the atria and ventricles. These patterns typically emerge when the sinoatrial (SA) node, which serves as the heart's primary pacemaker, fails to generate impulses. Understanding the main types of junctional rhythm strips is crucial for effective ECG analysis.
-
Junctional Escape Rhythm occurs when the SA node is inactive, allowing the AV junction to take over pacemaker responsibilities, usually at a rate of 40-60 beats per minute. This rhythm is particularly prevalent among younger and athletic individuals during periods of heightened vagal tone, such as sleep.
-
Accelerated Junctional Rhythm (AJR) is characterized by a firing rate of 60-100 beats per minute and often arises in response to increased vagal tone or other stimuli. Notably, the QRS duration in AJR is generally less than 120 milliseconds unless pre-existing conduction abnormalities are present.
-
Junctional Tachycardia features a rate exceeding 100 beats per minute and may be triggered by various factors, including increased sympathetic activity or digoxin toxicity. Junctional tachycardia can range from 120 to 220 beats per minute and may exhibit specific ECG characteristics, such as inverted retrograde P waves in inferior leads.
Understanding these definitions and categories is vital for recognizing the clinical significance of specific patterns in ECG analysis. For instance, a junctional rhythm strip can often show that junctional escape rhythms are benign and serve as a backup mechanism during bradycardia, particularly in patients with complete heart block or sick sinus syndrome. Clinical observations indicate that approximately 40-60% of patients may experience escape beats, emphasizing their prevalence and importance in cardiac monitoring.

Identify Key ECG Features of Junctional Rhythms
When analyzing a junctional rhythm strip on an ECG, several key features should be identified. Leveraging advanced tools like MaxYield™ can significantly enhance this process.
In junctional rhythm strips, P waves may be absent, inverted, or occur after the QRS complex. This variation arises because the electrical impulse originates from the atrioventricular (AV) junction rather than the sinoatrial (SA) node. Research shows that approximately 30-50% of connection patterns display absent P waves, emphasizing the necessity for thorough examination. Symptoms such as syncope, fatigue, or dizziness may emerge when certain heart patterns are not quickly recognized, highlighting the significance of identifying these characteristics in clinical practice. MaxYield™ assists in isolating and labeling these key features, transforming noisy recordings into detailed insights.
QRS Complex: The QRS complex is typically narrow (less than 0.12 seconds), indicating normal conduction through the ventricles unless a bundle branch block is present. This trait is essential for distinguishing specific patterns from other arrhythmias. MaxYield™ provides beat-by-beat analysis, facilitating rapid identification of the QRS complex characteristics.
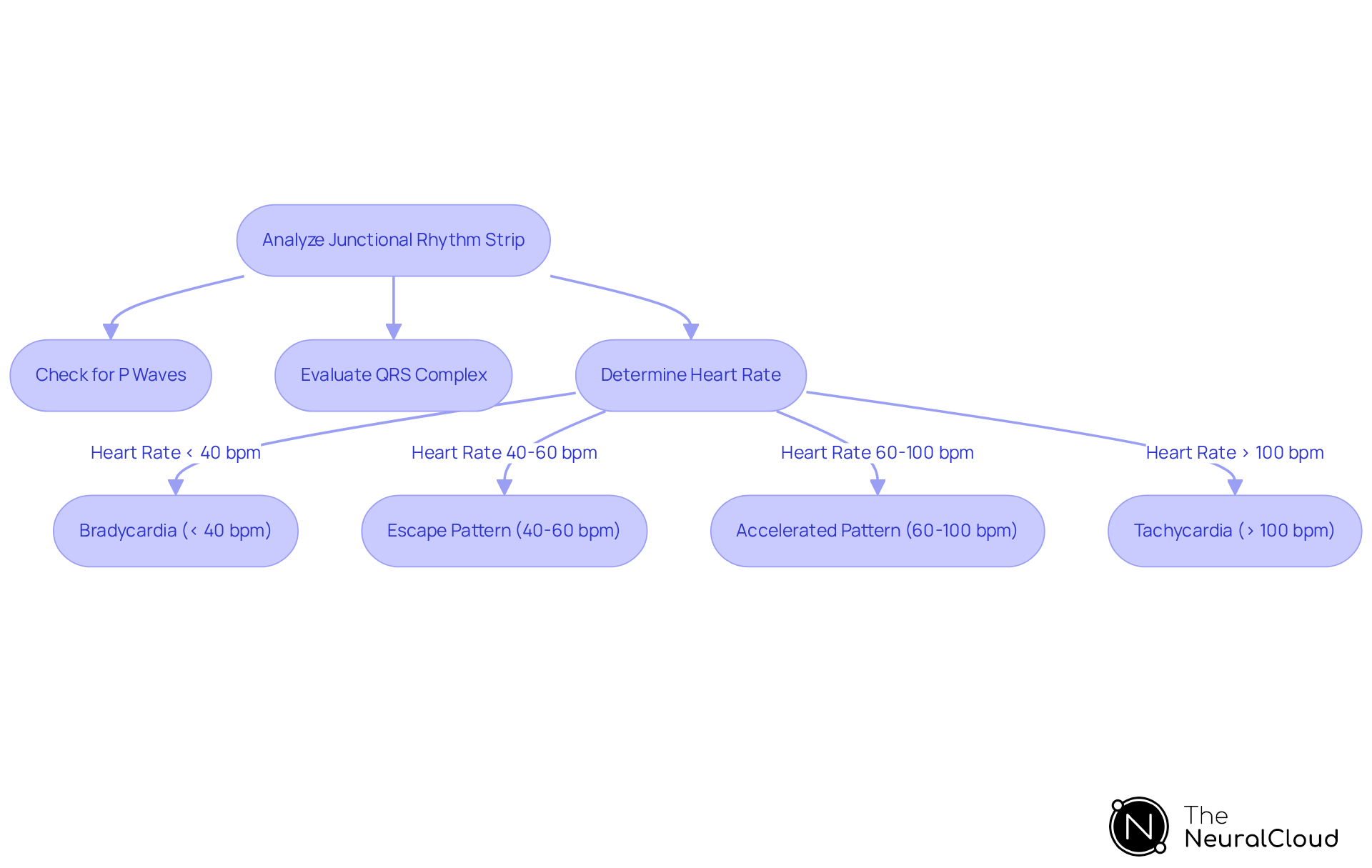
Heart Rate: The heart rate in connection patterns can vary significantly, categorized into:
- Connection bradycardia (below 40 bpm)
- Escape pattern (40-60 bpm)
- Accelerated connection pattern (60-100 bpm)
- Tachycardia (above 100 bpm)
Junctional bradycardia is defined by a junctional rhythm strip that displays a heart rate below 40 beats per minute. Precise measurement of the heart rate is crucial for identifying the particular type of connection pattern. With MaxYield™, you can analyze up to 200,000 heartbeats in under 5 minutes, ensuring prompt and precise evaluations.
Regularity: Connection patterns are typically steady, but fluctuations can arise, especially in escape patterns, where the pattern may be less consistent. This system supports confident clinical decisions by presenting smooth waveforms and clear data throughout your entire workflow.
By getting acquainted with these features and using MaxYield™, you will be better prepared to effectively analyze the junctional rhythm strip in ECG strips for junction patterns. Recent discoveries highlight that combining clinical history with targeted diagnostic assessments can accelerate management and enhance results for patients, especially in situations where certain heart patterns may result in complications if not quickly recognized. As one healthcare expert remarked, 'Timely recognition and management of the pattern and its underlying cause are crucial for enhancing results.
Follow a Step-by-Step Process for Analyzing Junctional Rhythm Strips
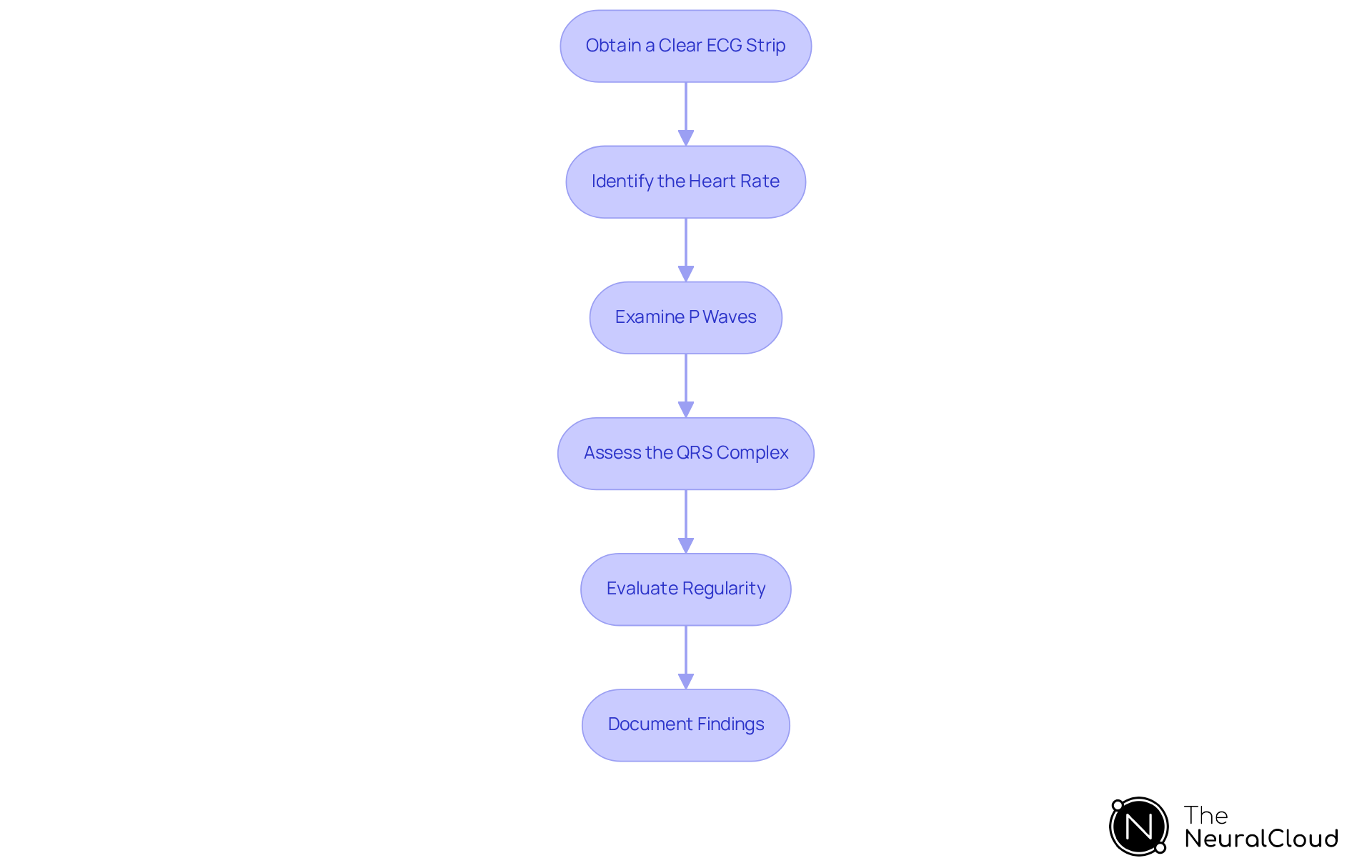
To effectively analyze junctional rhythm strips, adhere to the following structured steps:
-
Obtain a Clear ECG Strip: Ensure the ECG strip is of high quality, minimizing noise and artifacts to facilitate accurate analysis. Proper patient preparation and lead placement are crucial for achieving this clarity. Studies indicate that lead placement variability can alter diagnostic outcomes, so it is essential to position electrodes correctly to avoid common errors, such as placing V1 and V2 too high.
-
Identify the Heart Rate: Count the number of QRS complexes in a 6-second interval and multiply by 10 to determine the heart rate. This categorization is crucial for recognizing the type of heartbeat, which can vary from bradycardia (less than 40 BPM) to tachycardia (over 100 BPM).
-
Examine P Waves: Assess the presence, absence, or inversion of P waves. Their connection to the QRS complexes is crucial for identifying the specific type of junctional pattern, as inverted P waves are characteristic of this condition.
-
Assess the QRS Complex: Measure the width of the QRS complex. A normal width (0.04 to 0.10 seconds) indicates normal conduction, while a wider QRS may suggest a conduction delay or other underlying issues.
-
Evaluate Regularity: Determine if the beat is regular or irregular. Consistent patterns simplify analysis and interpretation, allowing for more straightforward clinical decisions.
-
Document Findings: Note your observations, including heart rate, pattern type, and any abnormalities observed. This documentation is crucial for clinical decision-making and ongoing patient management. Routine examinations and subsequent appointments with a provider are also crucial for managing the heart's electrical activity effectively.
By following these steps, you will improve your ability to analyze junctional rhythm strips with greater precision and assurance. Utilizing advanced solutions that offer beat-by-beat tabulation in CSV format and employ neural network models for complex signal processing can further enhance your ECG analysis. These features enable automated, scalable insights that improve clarity and efficiency in healthcare, ultimately leading to better patient outcomes.
Troubleshoot Common Issues in Junctional Rhythm Analysis
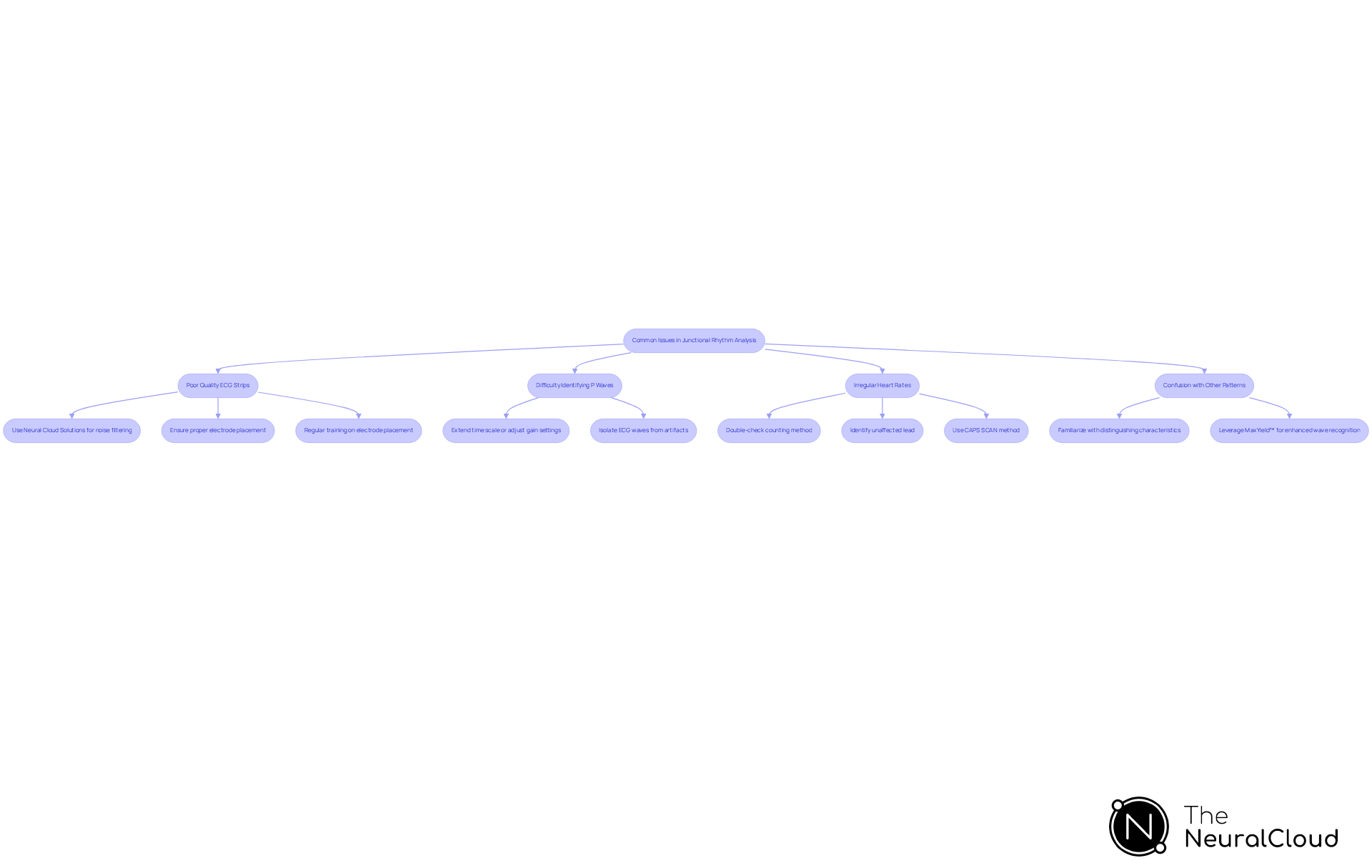
When analyzing a junctional rhythm strip, several common issues may arise. Here are some effective troubleshooting tips:
-
Poor Quality ECG Strips: Noisy ECG strips or those with artifacts can obscure critical data. To improve clarity, utilize Neural Cloud Solutions' platform, which employs advanced noise filtering to enhance ECG recordings. Additionally, ensure proper electrode placement and check for any loose connections. Regular training on electrode placement is crucial; studies indicate that only 10% of healthcare providers consistently place all leads correctly, highlighting the need for ongoing education to reduce errors.
-
Difficulty Identifying P Waves: If P waves are challenging to identify, consider extending the time scale or adjusting the gain settings on the ECG machine. Research shows that a biphasic P wave in lead V2 can indicate misplacement, complicating identification. The system can assist in isolating ECG waves from recordings with baseline wander and movement artifacts, thereby enhancing the identification process.
-
Irregular Heart Rates: For irregular heart rates, double-check your counting method. Measure over a consistent time frame and consider repeating the analysis if necessary. Artifact can mimic tachyarrhythmias, so identifying an unaffected lead can help clarify the pattern. Dr. Brooks Walsh suggests using a method he calls "CAPS SCAN" to evaluate ECGs, which includes checking for artifacts that interfere with waveform identification. The MaxYield™ platform's ability to salvage previously obscured sections of recordings can be invaluable in these situations.
Confusion with other patterns may arise when a junctional rhythm strip is mistaken for other arrhythmias. Acquaint yourself with the distinguishing characteristics of connecting patterns in comparison to atrial fibrillation or other supraventricular patterns to avoid misinterpretation. Misplacement of leads can create misleading patterns, such as a pseudo-infarct appearance, underscoring the importance of accurate lead placement. Leveraging MaxYield™ can help clarify these distinctions by providing enhanced wave recognition capabilities.
By recognizing these common issues and understanding how to address them, you can significantly enhance your proficiency in analyzing the junctional rhythm strip.
Conclusion
Mastering the analysis of junctional rhythm strips is essential for effective cardiac monitoring and diagnosis. Understanding the fundamental characteristics of junctional rhythms enables healthcare professionals to interpret ECGs more accurately and make informed clinical decisions. This article has outlined the definitions and types of junctional rhythms, key ECG features for identification, a structured step-by-step analysis process, and troubleshooting tips for common issues encountered during analysis.
Key insights discussed include:
- The importance of recognizing junctional escape rhythms
- Accelerated junctional rhythms
- Junctional tachycardia, each possessing distinct ECG characteristics
The article emphasizes the necessity of accurate heart rate measurement, P wave assessment, and QRS complex evaluation to differentiate these rhythms effectively. Furthermore, utilizing advanced tools like MaxYield™ can significantly enhance the accuracy of ECG interpretations, ensuring timely recognition and management of potential complications.
The significance of proficient junctional rhythm analysis extends beyond academic knowledge; it is a vital skill that can lead to improved patient outcomes. Healthcare professionals are encouraged to continuously refine their analysis techniques, stay updated on best practices, and utilize innovative solutions to enhance their diagnostic capabilities. By doing so, they contribute to better cardiac care and ultimately save lives.
Frequently Asked Questions
What are junctional rhythms?
Junctional rhythms are cardiac rhythms that originate from the atrioventricular (AV) junction, occurring when the sinoatrial (SA) node fails to generate impulses.
What is a Junctional Escape Rhythm?
A Junctional Escape Rhythm occurs when the SA node is inactive, allowing the AV junction to take over as the pacemaker, typically at a rate of 40-60 beats per minute. It is common among younger and athletic individuals during periods of heightened vagal tone, such as sleep.
What characterizes an Accelerated Junctional Rhythm (AJR)?
An Accelerated Junctional Rhythm is characterized by a firing rate of 60-100 beats per minute and often occurs in response to increased vagal tone or other stimuli. The QRS duration in AJR is usually less than 120 milliseconds unless there are pre-existing conduction abnormalities.
What is Junctional Tachycardia?
Junctional Tachycardia features a heart rate exceeding 100 beats per minute and may be triggered by factors such as increased sympathetic activity or digoxin toxicity. It can range from 120 to 220 beats per minute and may show inverted retrograde P waves in inferior leads on an ECG.
Why is understanding junctional rhythms important for ECG analysis?
Understanding junctional rhythms is vital for recognizing their clinical significance in ECG analysis, as they can indicate different cardiac conditions. For example, junctional escape rhythms are generally benign and serve as a backup mechanism during bradycardia, especially in patients with complete heart block or sick sinus syndrome.
How common are escape beats related to junctional rhythms?
Clinical observations indicate that approximately 40-60% of patients may experience escape beats, highlighting their prevalence and importance in cardiac monitoring.


