Introduction
Understanding the complexities of the heart's electrical activity is crucial for accurate ECG analysis, particularly as technology continues to evolve in the field of cardiac care. This article explores the key components of normal EKG results, equipping healthcare professionals with the necessary tools to enhance their diagnostic skills and improve patient outcomes. As reliance on automated systems increases, it raises an important question: How can clinicians effectively balance advanced technology with traditional interpretation skills to navigate the intricacies of ECG readings?
By addressing these challenges, we can better appreciate the features of the MaxYield™ platform, which streamlines ECG analysis. This platform not only simplifies the interpretation process but also enhances accuracy, ultimately benefiting healthcare providers and their patients. With MaxYield™, clinicians can leverage cutting-edge technology while retaining essential skills in ECG interpretation, ensuring comprehensive patient care.
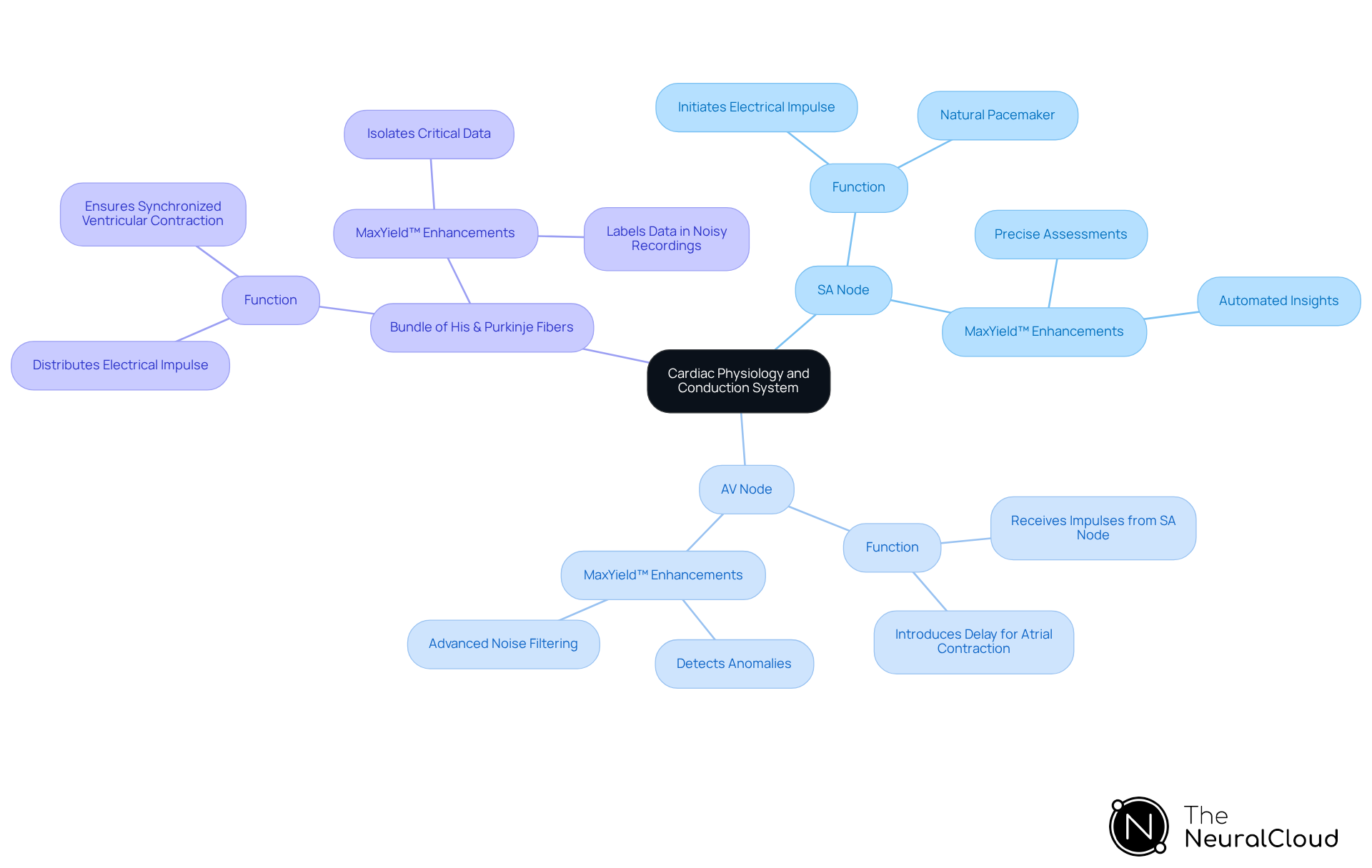
Explain Cardiac Physiology and Conduction System
The heart functions as a pump, driven by electrical impulses that coordinate its contractions. The cardiac conduction system consists of specialized cells that generate and propagate these impulses. Understanding its key components is essential for effective ECG analysis:
-
Sinoatrial (SA) Node: This is the heart's natural pacemaker, initiating the electrical impulse that triggers each heartbeat. Proper function of the SA node is crucial; any dysfunction can lead to arrhythmias, affecting overall cardiac health. The integration of the MaxYield™ system enhances the analysis of SA node function by providing automated insights into the heart's electrical activity, allowing for more precise assessments.
-
Atrioventricular (AV) Node: The AV node receives impulses from the SA node and introduces a slight delay, enabling the atria to contract fully before the ventricles respond. This timing is vital for efficient blood circulation. MaxYield™ assists in detecting anomalies in this process through its advanced noise filtering capabilities.
-
Bundle of His and Purkinje Fibers: These structures distribute the electrical impulse throughout the ventricles, ensuring synchronized contraction. Abnormalities in these pathways can lead to conditions like bundle branch block, characterized by wide QRS complexes on an ECG. Recognizing these complexes is crucial for diagnosing ventricular rhythms and blocks, as they may indicate significant cardiac conditions. MaxYield™ enhances this diagnostic process by rapidly isolating and labeling critical data, even in recordings with high levels of noise and artifact.
Understanding these components is vital for interpreting ECGs, as they directly influence the waveform patterns observed in an EKG strip. For example, the presence of a Q wave is permanent after myocardial infarction and does not indicate the age of the infarction, underscoring the need for context in evaluations. Recent studies emphasize that identifying the rhythm set by the SA node is essential for diagnosing potential abnormalities, reinforcing the importance of a systematic approach in ECG evaluation. Familiarity with normal EKG results numbers and abnormal patterns enhances diagnostic capabilities, empowering healthcare professionals to make informed decisions based on accurate cardiac insights. With MaxYield™, health tech developers can leverage automated ECG analysis to improve workflow efficiency and enhance clinical decision-making.
Identify Normal EKG Intervals and Waveforms
The accurate interpretation of cardiac function relies on normal EKG results numbers and waveforms. Understanding these components not only aids in diagnosis but also enhances clinical decision-making and patient outcomes. Here’s a breakdown of the key features:
- P Wave: Represents atrial depolarization, with a normal duration of less than 120 milliseconds and an amplitude of less than 2.5 mm. Variations in P morphology, such as notched or biphasic shapes, can indicate underlying atrial conditions, which is vital for early detection.
- PR Interval: Measures the time from the onset of the P deflection to the beginning of the QRS complex, with a normal range of 120-200 milliseconds. Prolongation may suggest conduction delays, while a shortened interval could indicate pre-excitation syndromes, highlighting the importance of monitoring this interval.
- QRS Complex: Reflects ventricular depolarization, with a normal duration of 80-100 milliseconds. Narrow QRS complexes are typically seen in healthy individuals, while wider complexes may indicate ventricular hypertrophy or conduction abnormalities, which can significantly impact patient care.
- T Wave: Indicates ventricular repolarization and is typically upright in leads I, II, V3-V6. T inversions can be indicative of ischemia or other cardiac conditions, making their recognition essential for timely intervention.
- QT Interval: Spans from the start of the Q wave to the end of the T wave, with a normal range of 350-450 milliseconds. Prolonged QT intervals can increase the risk of arrhythmias, underscoring the necessity for clinicians to monitor this parameter closely.
By grasping these values, healthcare professionals can swiftly evaluate the heart's electrical activity, compare it with normal EKG results numbers, and detect potential abnormalities, ultimately leading to improved patient outcomes.

Utilize Advanced Technology for Enhanced EKG Analysis
Advanced technologies, particularly AI-driven platforms like Neural Cloud Solutions' MaxYield™, are revolutionizing ECG evaluation. The challenges in ECG analysis often stem from the vast amounts of data and the need for accurate interpretation. MaxYield™ addresses these challenges through its innovative features, which significantly enhance the diagnostic process for healthcare professionals.
-
Automated Analysis: MaxYield™ employs advanced algorithms to efficiently process extensive ECG data. It accurately identifies critical features and abnormalities, even in recordings affected by noise and artifacts. This capability allows for the analysis of 200,000 heartbeats in under 5 minutes, greatly improving detection rates for conditions such as arrhythmias and myocardial infarction.
-
Real-Time Feedback: The platform provides clinicians with immediate insights, facilitating timely decision-making in critical situations. Notably, it reduces false positive rates dramatically-from nearly 42% to about 8%-which enhances patient outcomes and treatment efficiency.
-
Integration with Clinical Workflows: MaxYield™ seamlessly integrates with existing systems, boosting operational efficiency without disrupting established practices. This adaptability allows healthcare providers to incorporate advanced evaluation into their routine workflows, optimizing resource allocation. However, experts highlight ongoing challenges in effectively integrating these systems into clinical settings.
-
Continuous Learning: The platform continually enhances its diagnostic capabilities by learning from new data. This dynamic evolution ensures that healthcare professionals benefit from the latest advancements in ECG evaluation, ultimately maximizing diagnostic yield.
Healthcare leaders, including Manuel Martínez-Sellés, emphasize the growing importance of AI in ECG diagnosis and management. As more data becomes available and algorithms evolve, leveraging these advanced technologies will significantly enhance diagnostic capabilities and optimize resource allocation, leading to improved patient care.

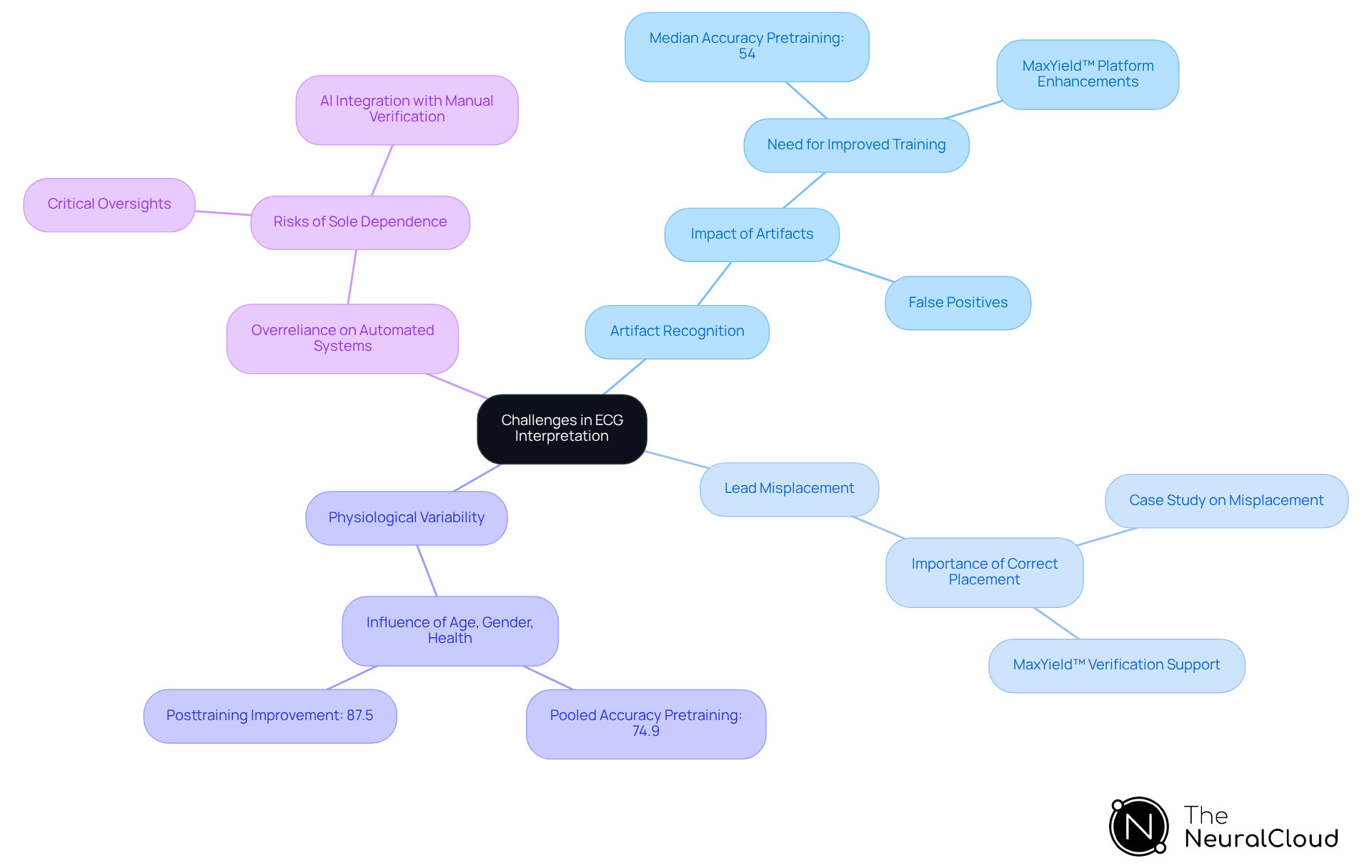
Address Challenges in ECG Interpretation
ECG interpretation presents several challenges that can significantly impact diagnostic accuracy. Key issues include:
-
Artifact Recognition: External factors, such as muscle tremors or electrical interference, can distort ECG readings. Clinicians must be adept at identifying these artifacts to differentiate them from genuine cardiac events. Recent studies indicate that misinterpretations due to artifacts can lead to false positives, complicating clinical decision-making. For instance, a systematic review found that the median accuracy for pretraining assessments was only 54%, highlighting the critical need for improved training in artifact recognition. The MaxYield™ platform enhances this process by utilizing advanced noise filtering and distinct wave recognition, allowing for the rapid isolation of ECG waves even in recordings with high levels of noise and artifact.
-
Lead Misplacement: Incorrect electrode placement is a common source of misinterpretation. Clinicians should always confirm lead placement before evaluation to ensure accurate readings. A case study demonstrated that misplacement can lead to significant diagnostic errors, underscoring the importance of proper technique. The MaxYield™ platform assists in verifying lead placement, reducing the risk of misinterpretation.
-
Physiological Variability: Factors such as age, gender, and overall health can influence ECG results. A thorough understanding of these variations is crucial for accurate interpretation, as they can mask underlying conditions. For example, the accuracy of ECG interpretation varied widely across studies, with cardiologists achieving a pooled accuracy of 74.9% pretraining, which improved to 87.5% posttraining. The MaxYield™ system continuously evolves its algorithms with each use, enhancing accuracy and efficiency in recognizing these physiological variabilities.
-
Overreliance on Automated Systems: While AI technologies can enhance ECG analysis, clinicians should not depend solely on automated interpretations. Manual verification remains essential to confirm accuracy, especially in borderline cases where algorithms may falter. As noted by experts, relying solely on automated systems can lead to critical oversights in patient care. However, with MaxYield™, the integration of AI-driven automation supports clinicians by providing a more reliable diagnostic yield, addressing inefficiencies and improving overall patient outcomes.
By recognizing these challenges and implementing effective strategies, healthcare professionals can enhance their ECG interpretation skills, ultimately leading to improved patient outcomes.
Conclusion
Mastering EKG results numbers is essential for accurate ECG analysis, equipping healthcare professionals with the knowledge needed to interpret cardiac function effectively. A thorough understanding of the cardiac conduction system, normal EKG intervals, and the integration of advanced technologies like MaxYield™ ensures that clinicians can identify abnormalities with precision and confidence. This foundational knowledge not only enhances diagnostic capabilities but also plays a crucial role in improving patient outcomes.
Key insights from the article highlight the importance of recognizing the components of the cardiac conduction system, such as the SA and AV nodes, as well as understanding normal EKG waveforms and intervals. The article emphasizes the role of advanced technology in streamlining ECG analysis, addressing common challenges like artifact recognition and lead misplacement. By leveraging these insights and tools, healthcare professionals can enhance their interpretation skills, leading to more accurate diagnoses and timely interventions.
Ultimately, mastering normal EKG results numbers contributes to the broader goal of improving cardiac care. As the field of ECG analysis continues to evolve with technological advancements, embracing these changes while honing interpretation skills will empower clinicians to provide the highest standard of care. This not only benefits patients but also strengthens healthcare systems as a whole.
Frequently Asked Questions
What is the primary function of the heart?
The heart functions as a pump, driven by electrical impulses that coordinate its contractions.
What are the key components of the cardiac conduction system?
The key components of the cardiac conduction system include the Sinoatrial (SA) Node, Atrioventricular (AV) Node, Bundle of His, and Purkinje Fibers.
What role does the Sinoatrial (SA) Node play in the heart?
The SA Node is the heart's natural pacemaker, initiating the electrical impulse that triggers each heartbeat. Proper function of the SA node is crucial for maintaining cardiac health.
How does the Atrioventricular (AV) Node contribute to heart function?
The AV Node receives impulses from the SA Node and introduces a slight delay, allowing the atria to contract fully before the ventricles respond, which is vital for efficient blood circulation.
What is the function of the Bundle of His and Purkinje Fibers?
The Bundle of His and Purkinje Fibers distribute the electrical impulse throughout the ventricles, ensuring synchronized contraction.
What is a bundle branch block, and how is it identified on an ECG?
A bundle branch block is characterized by wide QRS complexes on an ECG, indicating abnormalities in the electrical pathways. Recognizing these complexes is crucial for diagnosing ventricular rhythms and blocks.
How does the MaxYield™ system enhance cardiac analysis?
The MaxYield™ system provides automated insights into the heart's electrical activity, enhances the detection of anomalies, and improves diagnostic processes by rapidly isolating and labeling critical data, even in noisy recordings.
Why is understanding ECG waveform patterns important?
Understanding ECG waveform patterns is vital for interpreting EKG strips, as they directly influence diagnosis and can indicate significant cardiac conditions.
What is the significance of the Q wave in an ECG?
The presence of a Q wave is permanent after a myocardial infarction and does not indicate the age of the infarction, highlighting the importance of context in evaluations.
How does familiarity with normal and abnormal EKG results benefit healthcare professionals?
Familiarity with normal EKG results and abnormal patterns enhances diagnostic capabilities, empowering healthcare professionals to make informed decisions based on accurate cardiac insights.






