Overview
The article examines the techniques for accurately analyzing ST elevation in leads V2 and V3 of an ECG, a critical factor in diagnosing conditions such as STEMI. It underscores the necessity of understanding specific ST elevation criteria and the utilization of advanced diagnostic tools. Notably, the MaxYield™ software is highlighted for its role in enhancing accuracy and efficiency in identifying ST changes. By improving these diagnostic processes, the platform ultimately contributes to better patient outcomes.
Introduction
Understanding ST elevation in leads V2 and V3 is essential for precise ECG analysis, as it frequently indicates acute myocardial infarction—a condition that requires immediate medical attention. This article explores the techniques necessary for identifying and interpreting ST elevation patterns, emphasizing the clinical implications and the critical need for timely diagnosis. Given that various conditions can mimic ST elevation, healthcare professionals must be equipped to ensure accurate interpretation and avoid common pitfalls in ECG analysis.
Define ST Elevation and Its Clinical Importance
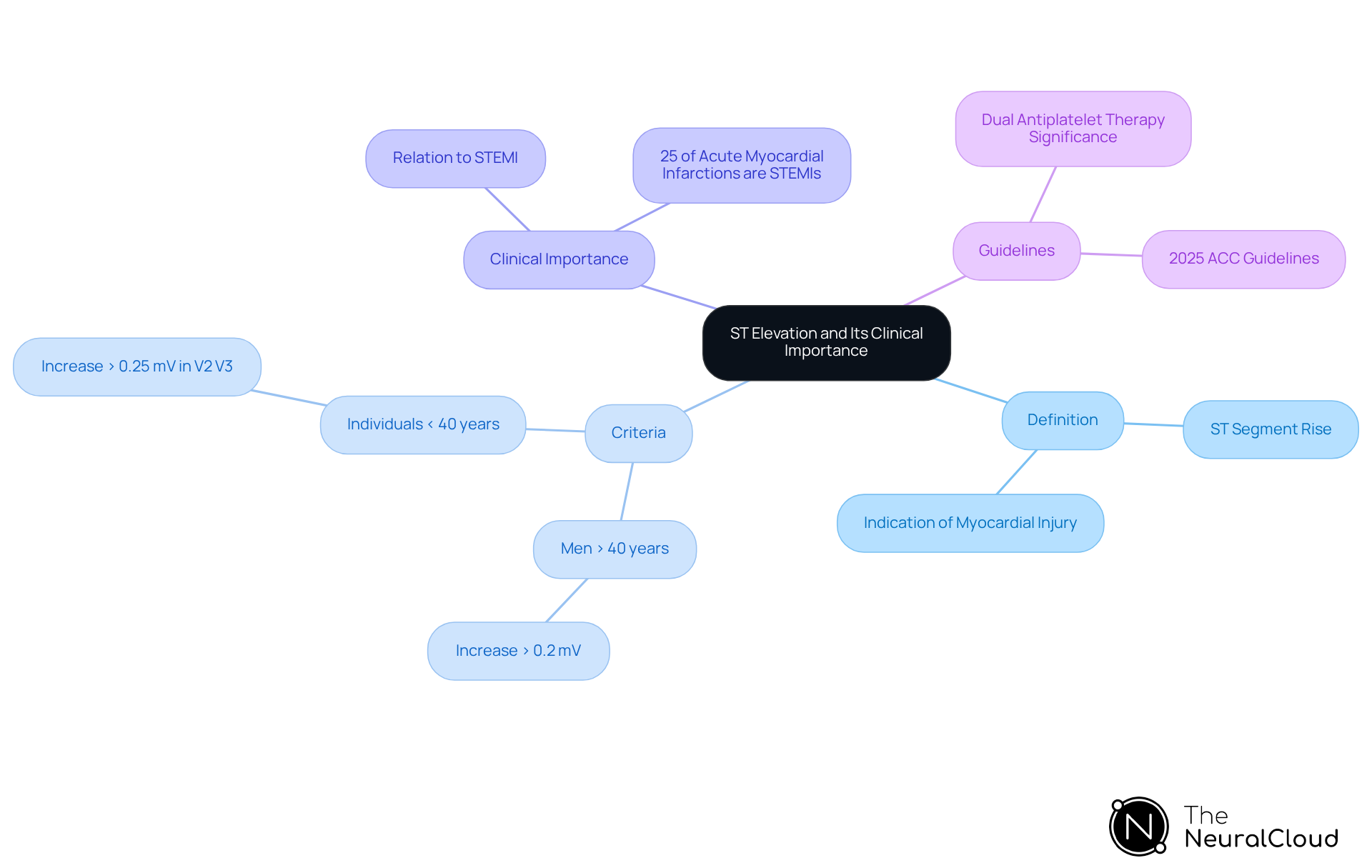
ST rise denotes an upward shift in the ST segment of an electrocardiogram (ECG), indicating potential myocardial injury. It is clinically described as a rise of the ST segment by more than 1 mm in two or more adjacent recordings, with specific thresholds differing by age and gender.
For instance:
- Men older than 40 years necessitate an increase greater than 0.2 mV.
- Individuals younger than 40 require more than 0.25 mV in ST elevation V2 V3 leads.
Identifying ST elevation V2 V3 is essential, as it frequently indicates acute ST-segment rise myocardial infarction (STEMI), which requires prompt medical action to restore blood flow and reduce heart injury. Recent studies indicate that approximately 25% of acute myocardial infarctions are STEMIs, underscoring the need for prompt recognition and treatment.
Moreover, the American College of Cardiology's 2025 guidelines stress the significance of dual antiplatelet therapy for patients at risk, highlighting the evolving understanding of ST changes' clinical implications. Comprehending the clinical significance of ST change allows healthcare professionals to effectively prioritize their diagnostic and therapeutic strategies, ultimately enhancing patient outcomes.
Analyze ST Elevation Patterns in Leads V2 and V3
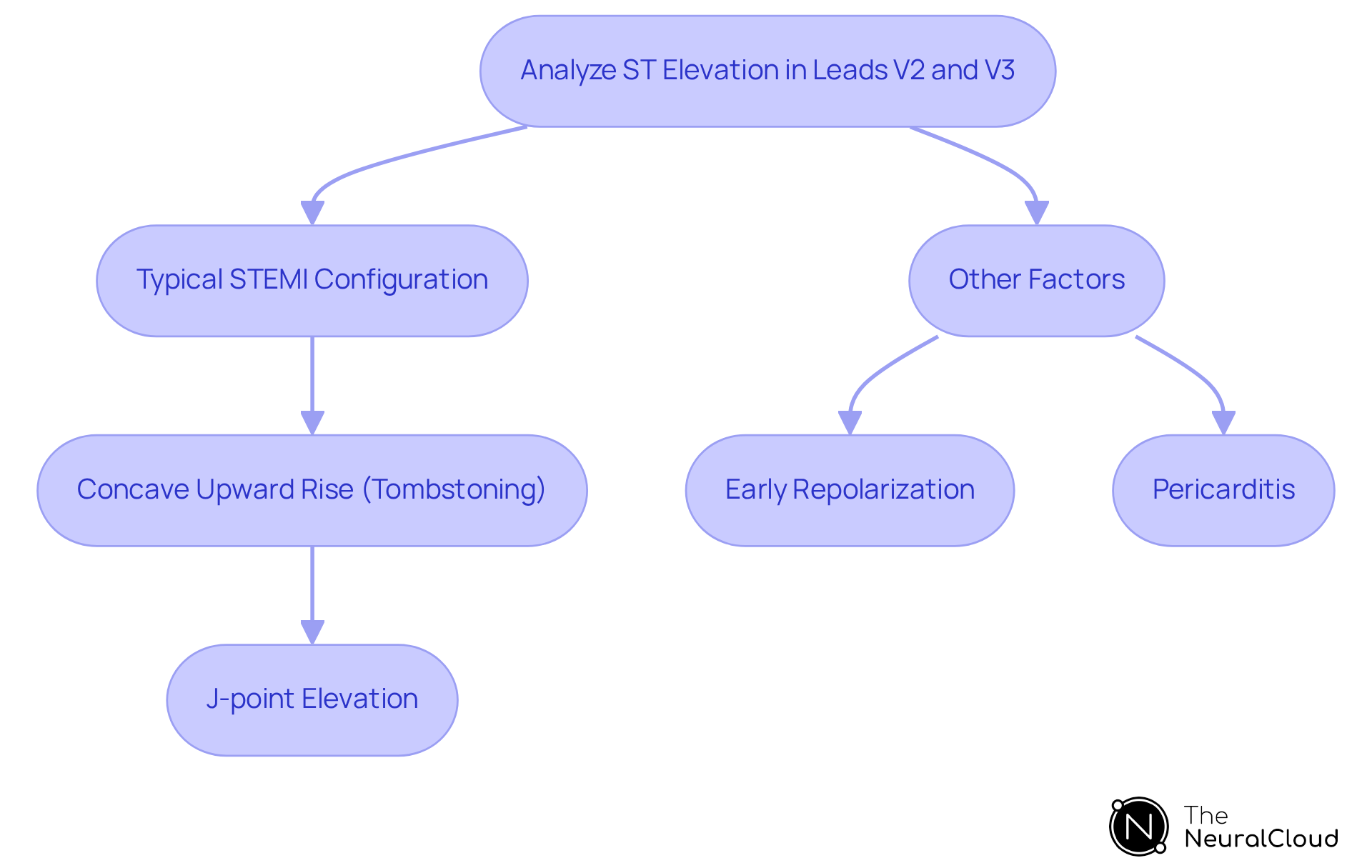
In leads V2 and V3, ST elevation V2 V3 can manifest in various forms, each indicating different underlying conditions. A typical STEMI configuration displays a concave upward rise, commonly known as 'tombstoning.' This configuration is marked by a significant elevation at the J-point, where the QRS complex intersects with the ST segment. Furthermore, the presence of reciprocal changes in inferior leads (II, III, and aVF) can further substantiate the diagnosis of STEMI.
MaxYield™ enhances automated ECG analysis by effectively identifying these patterns. It isolates and labels key features in every heartbeat, enabling rapid analysis of 200,000 heartbeats in under 5 minutes. Importantly, it is crucial to differentiate between ST elevation V2 V3 due to ischemia and other factors, such as early repolarization or pericarditis. For example, in pericarditis cases, ST elevation is typically diffuse and may be accompanied by PR segment depression.
By leveraging MaxYield™'s advanced algorithms, clinicians can adeptly manage physiological variability and noise, ensuring that the analysis remains both accurate and reliable. Understanding these patterns is essential for clinicians to make informed decisions regarding patient management. The integration of MaxYield™ not only streamlines the ECG analysis process but also empowers healthcare professionals to enhance patient care.
Evaluate Diagnostic Techniques for ST Elevation
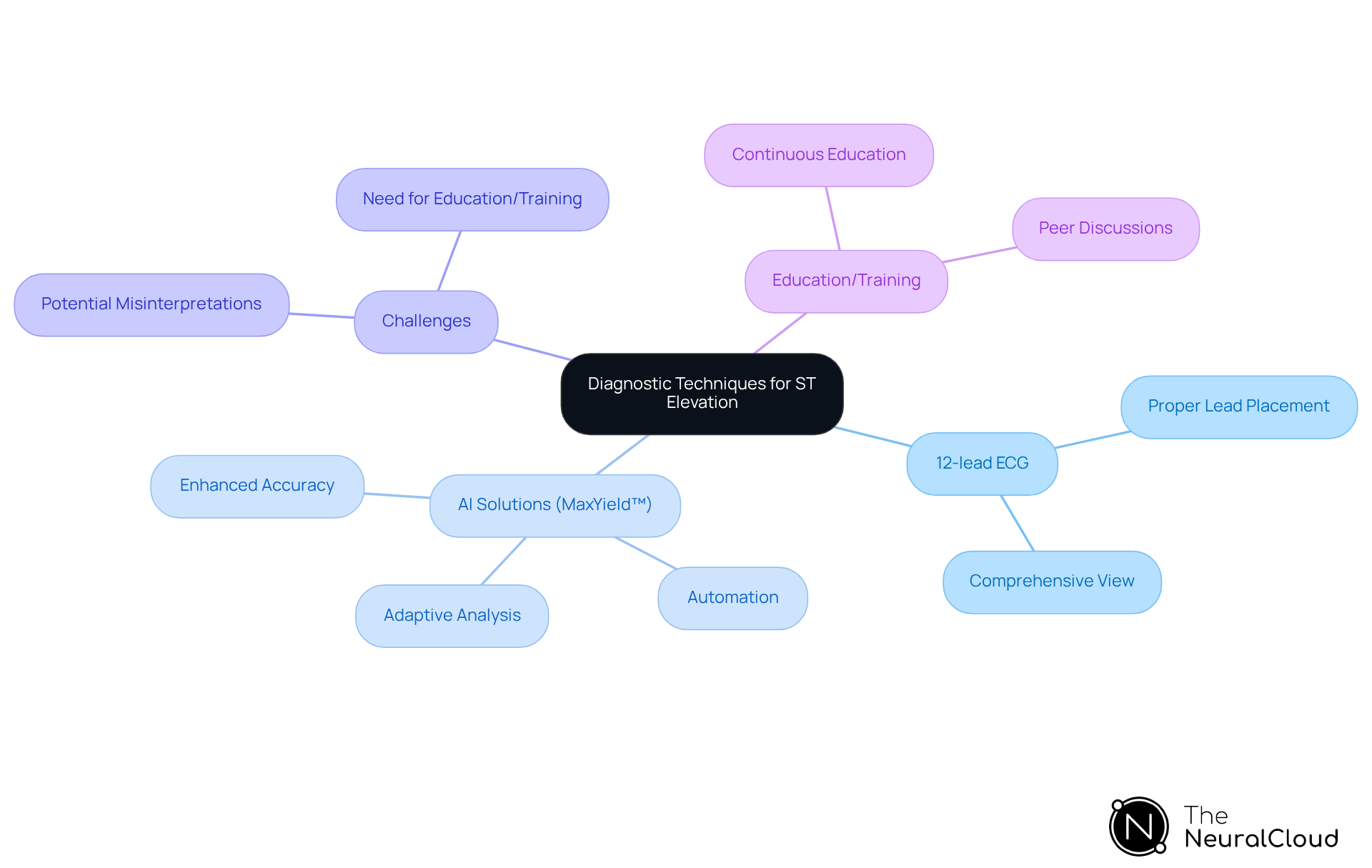
Accurately diagnosing ST rise presents several challenges, primarily addressed through the 12-lead ECG, which offers a comprehensive view of the heart's electrical activity. Clinicians must ensure proper lead placement to prevent misinterpretation caused by artifacts or lead misplacement. Advanced solutions, such as the automated ECG analysis software MaxYield™ by Neural Cloud Solutions, significantly enhance the precision and efficiency of identifying ST changes. This platform utilizes cutting-edge AI technology that evolves with each use, improving diagnostic yield and reducing workload through automation.
However, caution is warranted, as automated systems may struggle to differentiate between STEMI and other conditions, such as early repolarization or Brugada syndrome. Continuous education and training in ECG interpretation are essential for healthcare professionals to remain current with the latest diagnostic criteria and methodologies. Regularly reviewing case studies and engaging in peer discussions can further enhance diagnostic accuracy and clinical confidence.
Notably, effective utilization of the 12-lead ECG, particularly when integrated with advanced AI solutions like MaxYield™, significantly improves the timely diagnosis of ST elevation V2 V3. This ultimately leads to enhanced patient outcomes. The features of MaxYield™ include:
- Advanced AI-driven analysis that adapts to user input.
- Automation that streamlines the diagnostic process.
- Enhanced accuracy in identifying ST changes.
The advantages for healthcare professionals are clear: improved diagnostic precision, reduced workload, and increased confidence in clinical decision-making.
Conclusion
Understanding ST elevation in leads V2 and V3 is crucial for the timely and accurate diagnosis of myocardial injury, particularly in cases of STEMI. This article emphasizes the importance of recognizing specific ST elevation patterns and their clinical implications, which are essential for effective patient management. By leveraging advanced diagnostic techniques and technologies, healthcare professionals can enhance their ability to interpret ECG results accurately, ultimately improving patient outcomes.
Key insights discussed include:
- The definition and clinical significance of ST elevation
- The various patterns observed in leads V2 and V3
- The role of automated analysis tools like MaxYield™
These elements underscore the necessity for continuous education and the integration of advanced technology in ECG interpretation. Accurate identification of ST elevation not only aids in diagnosis but also informs treatment decisions, thereby significantly impacting patient care.
Reflecting on the significance of mastering ST elevation analysis, it becomes clear that improving diagnostic capabilities is paramount in the fast-paced medical environment. Healthcare professionals are encouraged to embrace ongoing training and utilize innovative tools to refine their skills in ECG interpretation. By doing so, they can ensure that they are prepared to respond effectively to acute cardiac events, ultimately leading to better patient outcomes and a higher standard of care in the field of cardiology.
Frequently Asked Questions
What does ST elevation indicate on an electrocardiogram (ECG)?
ST elevation indicates a potential myocardial injury, characterized by an upward shift in the ST segment of an ECG.
How is ST elevation clinically defined?
ST elevation is clinically defined as a rise of the ST segment by more than 1 mm in two or more adjacent recordings, with specific thresholds differing by age and gender.
What are the ST elevation thresholds for men older than 40 years?
Men older than 40 years require an increase greater than 0.2 mV to be considered ST elevation.
What are the ST elevation thresholds for individuals younger than 40 years?
Individuals younger than 40 years require more than 0.25 mV in ST elevation in the V2 V3 leads.
Why is identifying ST elevation in leads V2 V3 important?
Identifying ST elevation in leads V2 V3 is essential because it frequently indicates acute ST-segment rise myocardial infarction (STEMI), which requires immediate medical action to restore blood flow and minimize heart injury.
What percentage of acute myocardial infarctions are STEMIs?
Approximately 25% of acute myocardial infarctions are classified as STEMIs.
What do the American College of Cardiology's 2025 guidelines emphasize regarding ST changes?
The guidelines emphasize the significance of dual antiplatelet therapy for patients at risk, reflecting the evolving understanding of the clinical implications of ST changes.
How does understanding ST changes impact healthcare professionals?
Understanding the clinical significance of ST changes allows healthcare professionals to prioritize their diagnostic and therapeutic strategies, ultimately enhancing patient outcomes.


