Overview
The article addresses the clinical significance and management of ST elevation in leads V2 and V3, which are essential for diagnosing myocardial ischemia and myocardial infarction. It highlights the challenges in ECG analysis, particularly the need for accurate measurement and interpretation of ST segment changes.
The MaxYield™ platform is introduced as a key feature that enhances ECG analysis through advanced diagnostic tools. This platform not only improves the precision of readings but also facilitates timely interventions, ultimately leading to better patient outcomes.
By leveraging the capabilities of the MaxYield™ platform, healthcare professionals can significantly enhance their diagnostic accuracy and effectiveness in managing cardiovascular conditions.
Introduction
Understanding the nuances of ST elevation is essential in cardiac care, particularly concerning the timely diagnosis and treatment of myocardial infarction. This article explores the intricate details of V2 and V3 ST elevation, providing health tech developers with a comprehensive tutorial on utilizing advanced ECG analysis tools. As the stakes rise with each heartbeat, it is crucial to consider the challenges developers face in ensuring their algorithms accurately detect these critical changes. Ultimately, overcoming these challenges is vital for improving patient outcomes.
Clarify ST Elevation: Definitions and Clinical Significance
ST displacement refers to an upward shift of the ST segment on an electrocardiogram (ECG), indicating potential myocardial ischemia or infarction. Clinically, ST rise is significant as it often indicates acute conditions such as ST-Rise Myocardial Infarction (STEMI). Identifying ST changes is essential for prompt intervention, as delays can result in higher morbidity and mortality. For instance, approximately 550,000 new cases of heart attacks occur annually in the U.S., with a significant portion being STEMIs that require immediate attention.
The height of ST displacement is usually quantified in millimeters above the baseline and must be evident in two or more adjacent recordings to be deemed significant. Specifically, a threshold of ≥1 mm in two adjacent electrodes is generally accepted, although this can vary based on electrode location and patient demographics. For instance:
- Males under 40 years need ≥2.5 mm of ST-segment rise in anterior leads, indicating v2 v3 ST elevation.
- Females of any age need ≥1.5 mm in the same leads.
Additionally, ST-segment rise should be assessed 0.04 seconds after the J-point for accurate measurement.
Understanding these parameters is essential for developers creating ECG analysis tools that aim to enhance diagnostic accuracy and clinical decision-making. The MaxYield™ platform from Neural Cloud Solutions integrates advanced algorithms that significantly enhance the detection and interpretation of ST changes. By filtering out noise and artifacts, it provides clearer insights into cardiac events. MaxYield™ offers beat-by-beat analysis, enabling the output of detailed insights from noisy recordings, which is crucial for accurate interpretation.
Recent studies have indicated that precise interpretation of ST rise can significantly enhance outcomes for individuals, as timely reperfusion therapy can lower mortality rates linked with STEMI. Furthermore, the TIMI risk score, which predicts mortality rates for STEMI, underscores the importance of accurate ECG interpretation in assessing patient risk. Therefore, integrating robust algorithms that recognize these critical ECG changes is vital for advancing cardiac care.

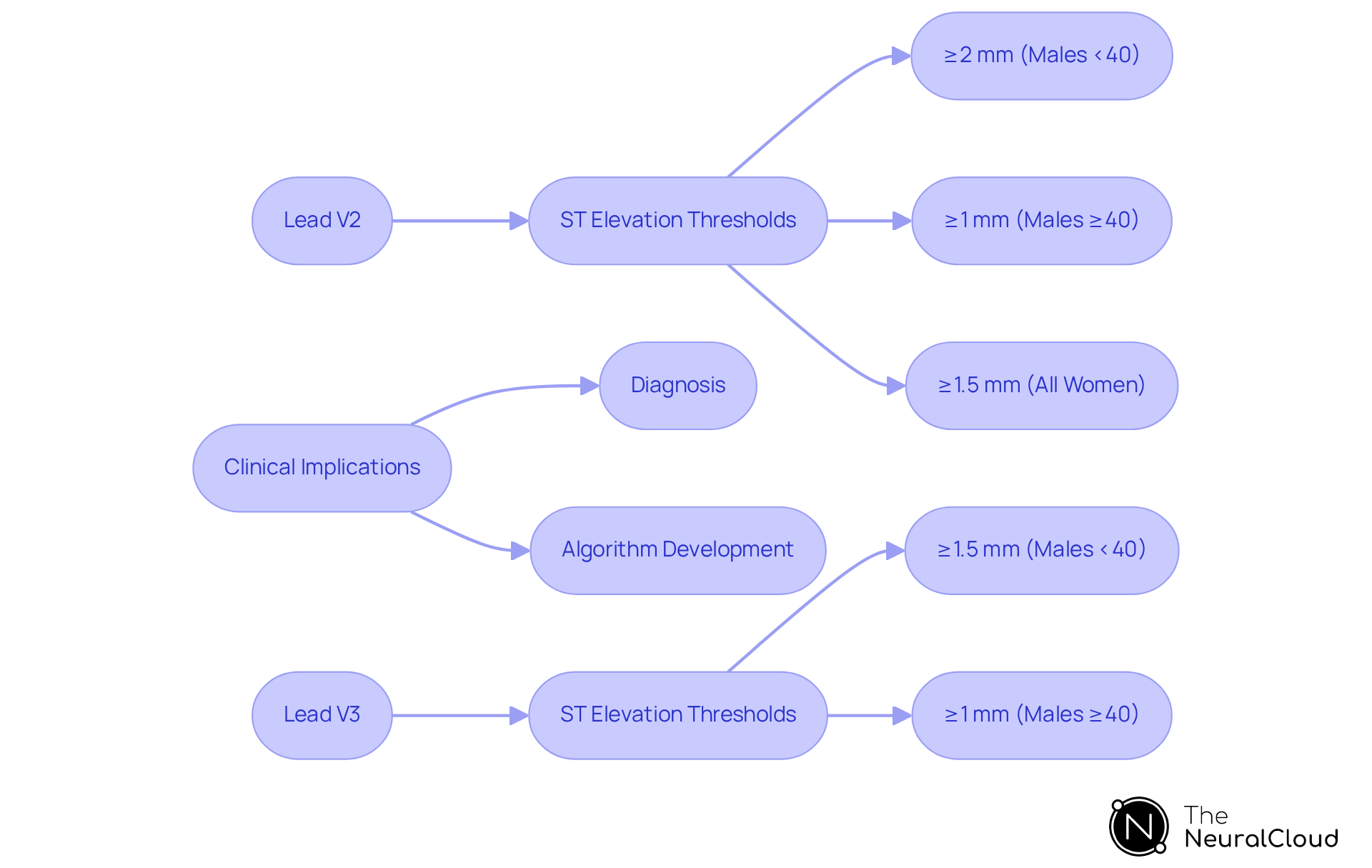
Differentiate v2 and v3 ST Elevation: Key Characteristics
In the context of ST segment rise, the V2 V3 ST elevation leads are critical for assessing anterior wall ischemia, each possessing distinct characteristics that influence diagnosis and treatment. MaxYield™ significantly enhances the evaluation of these leads by providing automated, noise-reduced ECG data, which facilitates clearer interpretation of ST segment rises.
- Lead V2: This lead typically requires a higher threshold for ST rise, with a ≥2 mm increase necessary for males under 40 years and ≥1 mm for older males. Women of any age need a ≥1.5 mm increase in ST-segment for this lead. Its sensitivity to anterior myocardial infarctions is vital for accurate diagnosis. MaxYield™ aids in isolating and labeling key features in the ECG signal, ensuring that clinicians can confidently identify significant increases and providing beat-by-beat analysis that enhances diagnostic yield.
- Lead V3: Conversely, V3 has a slightly lower elevation threshold, defined as ≥1.5 mm for men under 40 and ≥1 mm for older men. This electrode is often more reactive to changes in the anterior wall, making it an invaluable tool for detecting ischemic events. The advanced algorithms of MaxYield™ streamline the rapid analysis of these leads, offering detailed insights that bolster clinical decision-making.
Clinical Implications:
- Diagnosis: Distinguishing between leads V2 and V3 is essential for accurately locating ischemia, which directly impacts treatment decisions. A precise interpretation of V2 V3 ST elevation in these leads can significantly affect patient outcomes. With MaxYield™, health tech developers can create tools that utilize automated analysis to enhance diagnostic accuracy and seamlessly integrate into clinical workflows.
- Algorithm Development: For health tech developers, grasping the intricacies of these leads is crucial when designing ECG analysis tools. Accurate interpretation of V2 V3 ST elevation patterns can enhance diagnostic capabilities and optimize clinical workflows, particularly when paired with the advanced features of MaxYield™.
Current Guidelines:
According to established guidelines, ST-segment elevation should be evaluated 0.04 seconds after the J-point for accurate measurement, ensuring clinicians can make informed decisions based on reliable data. Identifying the specific criteria for ST rise in these leads is essential for effective management of myocardial infarction, and MaxYield™ supports this by delivering detailed insights swiftly.
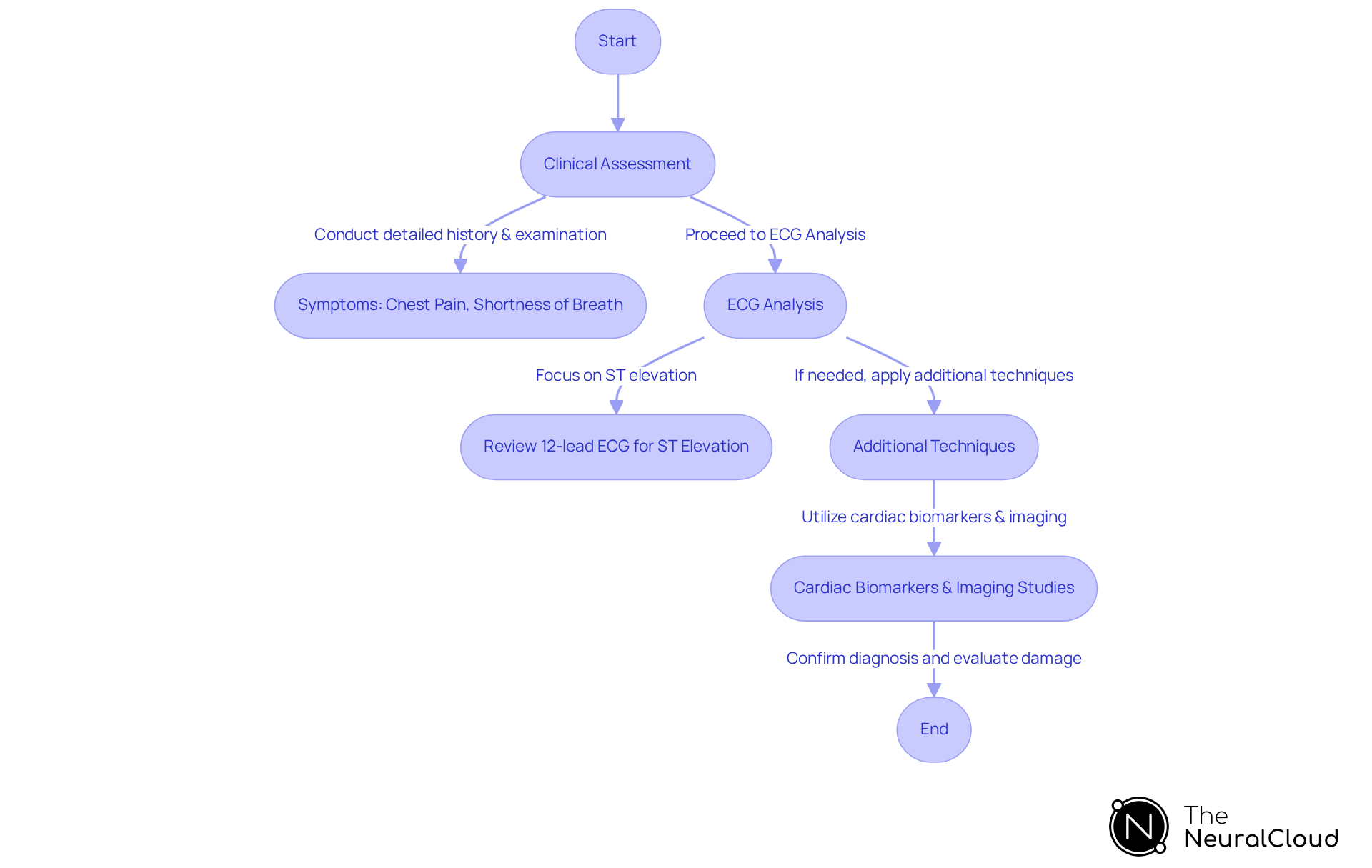
Evaluate ST Elevation: Diagnostic Approach and Techniques
Assessing ST rise necessitates a methodical approach that includes clinical evaluation, ECG analysis, and additional diagnostic methods.
Diagnostic Approach:
- Clinical Assessment: Initiate with a detailed patient history and physical examination, emphasizing symptoms such as chest pain, shortness of breath, and risk factors for coronary artery disease.
- ECG Analysis: Review the 12-lead ECG for v2 v3 ST elevation, focusing on the particular connectors involved and the degree of rise. Reciprocal changes in other leads can offer additional diagnostic insights.
- Additional Techniques: Utilize adjunctive tests like cardiac biomarkers (e.g., troponin levels) and imaging studies (e.g., echocardiography) to confirm the diagnosis and evaluate the extent of myocardial damage.
Techniques:
- Automated ECG Analysis: Employ Neural Cloud Solutions' MaxYield™ platform, which utilizes AI algorithms to improve the accuracy of ST elevation detection, significantly reducing interpretation time. Research shows that machine learning-based ECG systems can improve sensitivity for identifying ST segment myocardial infarction (STEMI) to as high as 90%. Notably, the pooled sensitivity of ST-segment rise for detecting acute coronary occlusion (ACO) is reported at 43.6%, highlighting the limitations of current diagnostic criteria. Furthermore, the OMI-NOMI strategy has shown improved sensitivity at 78.1% while maintaining a specificity of 94.4%, suggesting a more effective diagnostic approach.
- Continuous Monitoring: Implement continuous ECG monitoring for individuals at high risk using MaxYield™ to detect ST elevation in real-time, facilitating timely interventions. This proactive strategy can result in improved outcomes for individuals, as early diagnosis is associated with lower mortality rates in cases of v2 v3 ST elevation myocardial infarction.
The integration of advanced technologies in ECG analysis not only streamlines the diagnostic process but also empowers healthcare professionals to make informed decisions swiftly, ultimately enhancing patient care.
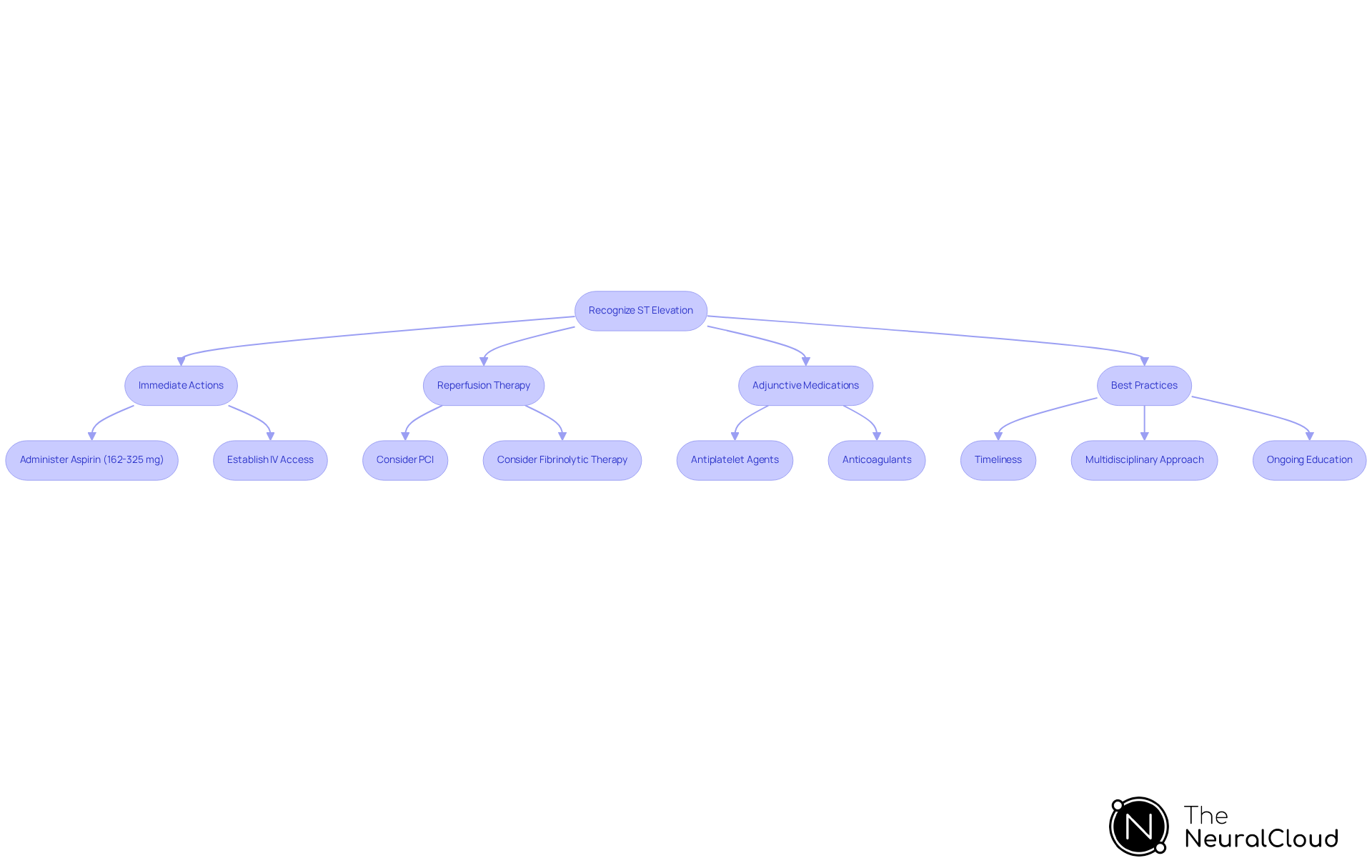
Manage ST Elevation: Treatment Protocols and Best Practices
Effectively managing v2 v3 st elevation necessitates a systematic method that emphasizes swift action and evidence-based treatment guidelines.
Treatment Protocols:
- Immediate Actions: Upon recognizing the v2 v3 st elevation, initiate the acute management protocol. This includes administering aspirin (162 to 325 mg) and establishing intravenous access.
- Reperfusion Therapy: Depending on the clinical scenario, consider primary percutaneous coronary intervention (PCI) or fibrinolytic therapy to restore blood flow to the affected myocardial tissue in cases of v2 v3 st elevation. PCI is highly recommended within the first 120 minutes following ischemic insult to minimize myocardial damage.
- Adjunctive Medications: Utilize antiplatelet agents such as clopidogrel (600 mg loading dose, 75 mg maintenance) or ticagrelor (180 mg loading dose, 90 mg twice daily maintenance), along with anticoagulants, to prevent further thrombus formation and effectively manage the individual's risk factors.
Best Practices:
- Timeliness: Treatment should be initiated as quickly as possible, ideally within the first hour of symptom onset. Delays can lead to significant myocardial damage and increased mortality risk. Restoring blood flow to the heart within 20 minutes is crucial to prevent serious damage or death during a heart attack.
- Multidisciplinary Approach: Collaborate with cardiologists, emergency medicine doctors, and nursing personnel to enhance care and simplify treatment protocols, ensuring a unified response to ST rise.
- Ongoing Education: Stay updated on the newest guidelines and developments in ST segment management to ensure clinical practices conform with current evidence, ultimately improving outcomes for individuals.
Real-world examples illustrate the effectiveness of reperfusion therapy in the management of v2 v3 st elevation. For instance, studies indicate that timely PCI significantly reduces mortality rates and enhances recovery outcomes in individuals experiencing v2 v3 st elevation myocardial infarction (STEMI). As A Maziar Zafari, MD, emphasizes, immediate transport to a PCI-capable hospital is recommended for those with suspected STEMI to ensure optimal outcomes. By adhering to these protocols and best practices, healthcare professionals can enhance the quality of care provided to patients facing this critical condition.
Conclusion
Understanding ST elevation is crucial for health tech developers aiming to enhance cardiac care through advanced diagnostic tools. This article has explored the definitions, clinical significance, and diagnostic approaches associated with ST elevation, particularly focusing on the v2 and v3 leads. By grasping the nuances of these parameters, developers can create more effective ECG analysis tools that improve the accuracy and speed of diagnosis, ultimately leading to better patient outcomes.
Key points emphasized include:
- Recognizing specific ST elevation thresholds for different demographics
- The role of advanced algorithms like those in the MaxYield™ platform
- The necessity of a systematic approach to diagnosis and treatment
Timely intervention can significantly reduce mortality rates associated with ST elevation myocardial infarction (STEMI), reinforcing the need for health tech innovations that support clinicians in real-time decision-making.
In conclusion, integrating cutting-edge technology in the evaluation and management of ST elevation streamlines clinical workflows and empowers healthcare professionals to act swiftly in critical situations. As advancements continue to emerge, it is imperative for developers and clinicians alike to stay informed and adapt to the evolving landscape of cardiac care, ensuring that every patient receives the timely and effective treatment they deserve.
Frequently Asked Questions
What does ST elevation refer to in an electrocardiogram (ECG)?
ST elevation refers to an upward shift of the ST segment on an ECG, which may indicate potential myocardial ischemia or infarction.
Why is ST elevation clinically significant?
ST elevation is significant because it often indicates acute conditions such as ST-Rise Myocardial Infarction (STEMI), and timely identification is crucial for prompt intervention to reduce morbidity and mortality.
How many new cases of heart attacks occur annually in the U.S.?
Approximately 550,000 new cases of heart attacks occur annually in the U.S., with a significant portion being STEMIs that require immediate attention.
How is the height of ST displacement quantified?
The height of ST displacement is quantified in millimeters above the baseline and must be evident in two or more adjacent recordings to be considered significant.
What is the general threshold for ST-segment rise to be deemed significant?
A threshold of ≥1 mm in two adjacent electrodes is generally accepted, although this may vary based on electrode location and patient demographics.
What are the specific ST elevation requirements for males and females under certain conditions?
Males under 40 years need ≥2.5 mm of ST-segment rise in anterior leads, while females of any age need ≥1.5 mm in the same leads.
When should ST-segment rise be assessed for accurate measurement?
ST-segment rise should be assessed 0.04 seconds after the J-point for accurate measurement.
How does the MaxYield™ platform enhance ECG analysis?
The MaxYield™ platform integrates advanced algorithms that improve the detection and interpretation of ST changes by filtering out noise and artifacts and providing beat-by-beat analysis for clearer insights.
What is the impact of precise interpretation of ST rise on patient outcomes?
Precise interpretation of ST rise can significantly enhance outcomes for individuals, as timely reperfusion therapy can lower mortality rates linked with STEMI.
Why is accurate ECG interpretation important in assessing patient risk?
Accurate ECG interpretation is vital for assessing patient risk, as demonstrated by the TIMI risk score, which predicts mortality rates for STEMI. Integrating robust algorithms that recognize critical ECG changes is essential for advancing cardiac care.


