Overview
Inferior wall infarction (IWI) is a specific type of myocardial infarction that primarily affects the lower wall of the heart. This condition often arises from a blockage of the right coronary artery and is characterized by ST-segment elevation in specific ECG leads. Effective diagnosis and treatment of IWI necessitate a combination of ECG analysis and advanced imaging techniques.
Timely medical interventions, such as primary percutaneous coronary intervention, are crucial. Furthermore, careful management of potential right ventricular involvement is essential. These elements collectively contribute to improved patient outcomes.
Introduction
Understanding inferior wall infarction is crucial for healthcare professionals, as it signifies a major cardiac event that can lead to severe complications. This article explores the complexities involved in diagnosing and treating this condition, providing insights into the latest research and methodologies. Given the intricate nature of ECG interpretations and the possibility of right ventricular involvement, clinicians must consider how to deliver the most effective care. By examining these questions, we aim to illuminate the path toward mastering the management of inferior wall infarction and enhancing patient outcomes.
Define Inferior Wall Infarction: Key Concepts and Pathophysiology
Inferior wall infarction (IWI) is a specific type of myocardial infarction (MI) that primarily affects the lower wall of the heart, often resulting from a blockage of the right coronary artery (RCA). This condition is typically identified by ST-segment elevation in the lower leads (II, III, and aVF) on an electrocardiogram (ECG). The underlying pathophysiology involves a significant reduction in blood flow to the lower myocardium, leading to ischemia and subsequent necrosis of cardiac tissue.
Recent research indicates that approximately 30 to 50% of individuals with lower segment infarcts may also experience right ventricular involvement, complicating clinical outcomes. Risk factors for IWI include:
- Atherosclerosis
- Coronary artery disease
- Hypertension
- Diabetes mellitus
Notably, a study revealed that patients with a pulse pressure (PP) of ≤50 mmHg during hospitalization exhibited a higher incidence of heart failure and mortality compared to those with PP >50 mmHg, highlighting the importance of monitoring hemodynamic parameters in these patients.
Typical symptoms of inferior wall infarction encompass:
- Chest pain, often described as retrosternal and radiating to the back
- Shortness of breath
For instance, a 52-year-old man presenting with chest pain and sweating was diagnosed with an acute lower segment myocardial event, confirmed by ECG results and later coronary angiography, which indicated a 100% thrombotic blockage in the RCA. This case underscores the critical necessity for prompt diagnosis and intervention in effectively managing inferior wall infarction.
To improve the efficiency of ECG analysis in diagnosing IWI, integrating wearable technology with Neural Cloud Solutions' MaxYield™ platform can significantly streamline processes. The automated ECG labeling and data extraction capabilities of MaxYield™ not only reduce operational costs but also enhance the accuracy and reliability of ECG readings. By leveraging AI-powered algorithms, MaxYield™ ensures smooth signals when analyzing and annotating abnormal electrocardiograms, addressing challenges such as physiological variability and signal artifacts. This enables healthcare professionals to allocate their time and skills more effectively, ultimately leading to improved outcomes for individuals and maximizing return on investments. Understanding these crucial concepts and risk factors is essential for healthcare providers to develop for patients at risk of inferior wall infarction and lower myocardial damage.

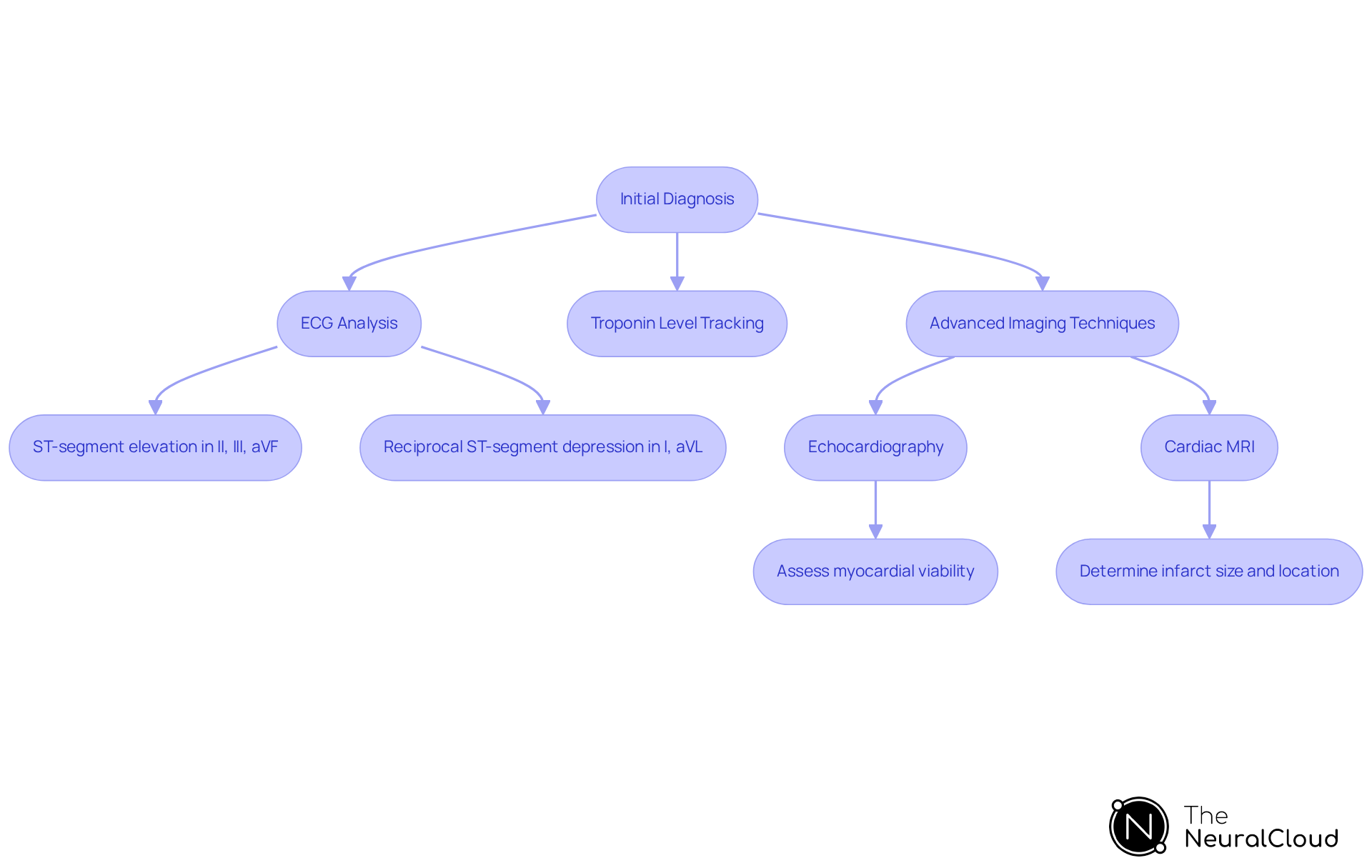
Diagnose Inferior Wall Infarction: ECG Interpretation and Imaging Techniques
Identifying lower myocardial damage requires a comprehensive strategy that combines ECG analysis with advanced imaging methods. Classic ECG findings typically include ST-segment elevation in leads II, III, and aVF, along with reciprocal ST-segment depression in lateral leads (I, aVL). These indicators are essential for detecting inferior wall infarction, which occurs in approximately 40% of all heart attacks and may also involve the right ventricle in up to 40% of cases.
The MaxYield™ platform significantly enhances this diagnostic process. It automates the mapping of ECG signals through noise, effectively isolating and labeling key features in every heartbeat. This functionality allows for beat-by-beat analysis, providing insights from 200,000 heartbeats in under 5 minutes. By delivering detailed information on P-wave, QRS complex, and T-wave onsets and offsets, MaxYield™ empowers healthcare professionals to identify cardiac events with greater accuracy and confidence.
Advanced imaging modalities, such as echocardiography and cardiac MRI, play a crucial role in assessing myocardial viability and the extent of damage. Echocardiography excels in evaluating motion abnormalities of the heart, offering real-time insights into cardiac function. In contrast, cardiac MRI provides detailed information regarding infarct size and location, which is vital for treatment planning. For instance, a case study demonstrated the effectiveness of cardiac MRI in guiding urgent interventions for an individual with a 100% proximal right coronary artery occlusion.
Tracking troponin levels is critical in identifying lower myocardial damage, as it helps detect increases in this heart protein in the blood, signaling myocardial injury. Utilizing these alongside clinical assessments enables healthcare professionals to conduct a thorough evaluation of the individual's condition. The integration of imaging methods not only enhances diagnostic precision but also informs subsequent management approaches, ultimately improving outcomes in cases of lower myocardial damage. Furthermore, urgent cardiac angiography should be performed within 90 minutes if ECG shows signs of ST elevation, underscoring the time-sensitive nature of treatment.
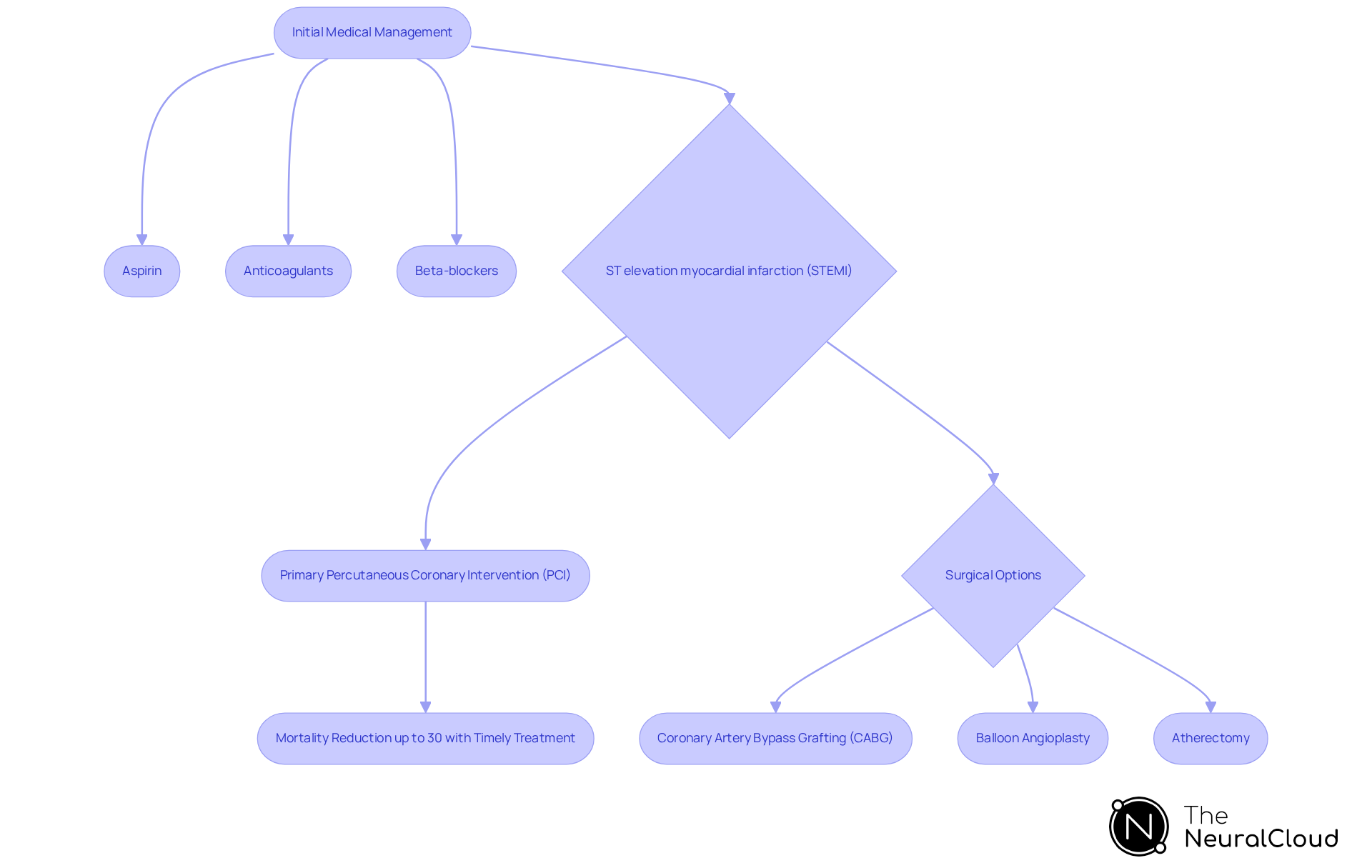
Treat Inferior Wall Infarction: Medical Management and Surgical Options
The management of inferior wall infarction encompasses a combination of medical care and surgical interventions. Initial medical strategies generally include the administration of aspirin, anticoagulants, and beta-blockers. These medications work to decrease myocardial oxygen demand and prevent further clot formation. For individuals experiencing ST-elevation myocardial infarction (STEMI), primary percutaneous coronary intervention (PCI) is recognized as the gold standard for restoring blood flow, demonstrating significant effectiveness in enhancing patient outcomes. Research indicates that timely PCI can substantially reduce mortality rates in STEMI patients, with some studies showing a mortality decrease of up to 30% when performed within the first 90 minutes of symptom onset, underscoring its critical role in acute care.
Surgical options, such as (CABG), may be required for patients with extensive coronary artery disease or those who do not respond adequately to PCI. Additionally, minimally invasive techniques, including balloon angioplasty and atherectomy, represent practical alternatives for restoring blood flow and can be tailored to the individual's specific condition. Continuous monitoring and follow-up care are vital for managing potential post-operative complications and ensuring optimal recovery. Current best practices advocate for a multidisciplinary approach, uniting cardiologists, surgeons, and rehabilitation specialists to enhance outcomes for individuals following an inferior wall infarction. It is equally important to address the emotional aspects of recovery, as many individuals may encounter feelings of weakness, depression, or anxiety after a heart attack, necessitating supportive care and counseling.
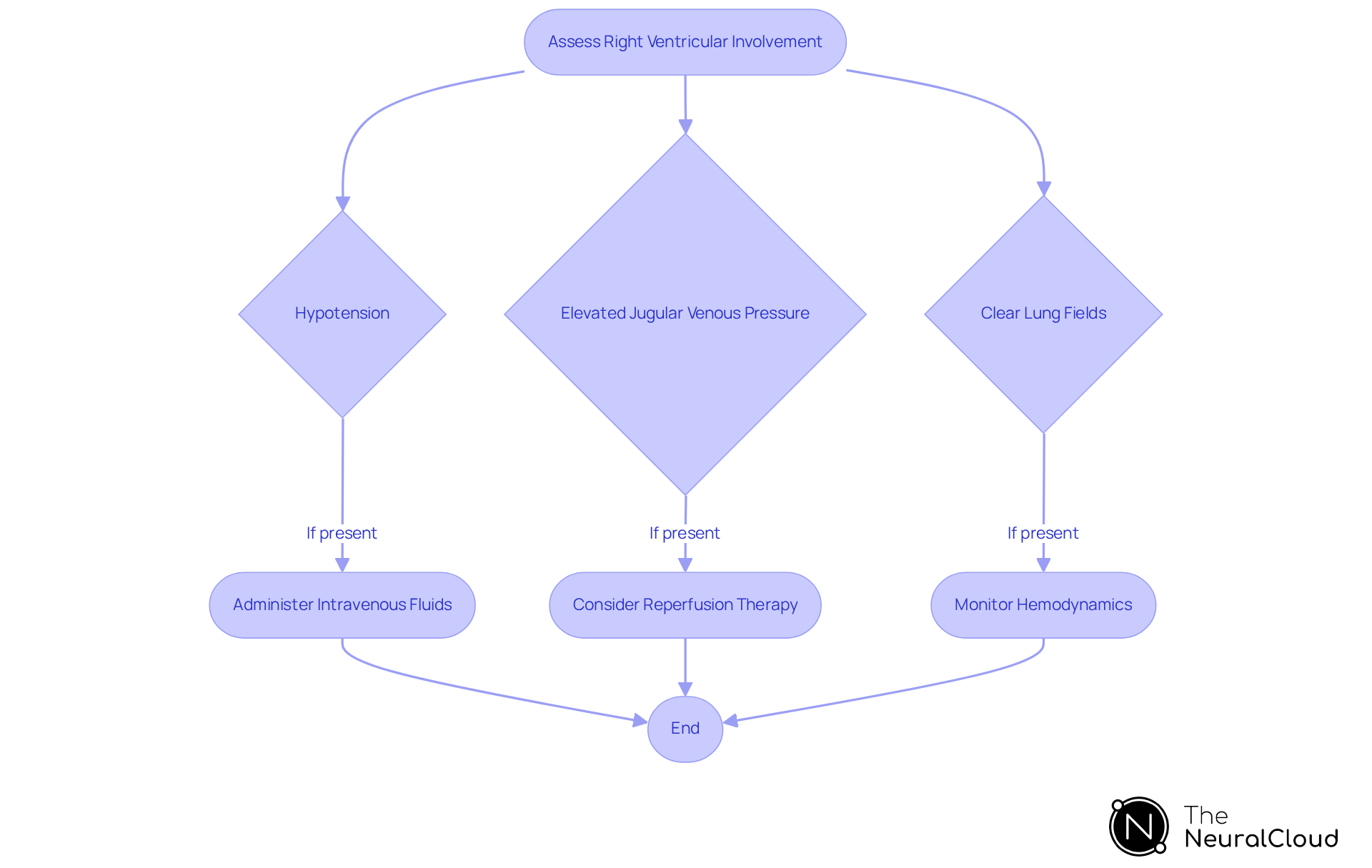
Assess Right Ventricular Involvement: Impact on Management and Prognosis
Evaluating right ventricular engagement in individuals with lower myocardial damage is essential, as it can complicate the clinical situation and significantly worsen prognosis. Right ventricular myocardial damage (RVMI) often occurs alongside lower section damage, particularly in cases of right coronary artery (RCA) blockage, which happens at a rate of 43%. Clinical signs indicative of RVMI include:
- Hypotension
- Elevated jugular venous pressure
- Clear lung fields
These are crucial for accurate diagnosis. The presence of RVMI necessitates specific management adjustments, such as administering intravenous fluids to maintain optimal right-sided filling pressures, typically recommended at 500-1000 mL.
Timely intervention is critical; individuals presenting within six hours of inferior wall infarction with RV involvement may benefit from pharmacologic or mechanical reperfusion therapy, which can enhance survival rates. In contrast, those presenting later than twelve hours may require a more conservative management approach. Understanding the is vital for improving treatment strategies and outcomes for individuals, especially since severe RVMI is associated with increased mortality rates. Notably, in females, the proportional mortality rate can reach 67%, underscoring the importance of careful clinical examination and echocardiographic assessment in guiding treatment decisions.
Furthermore, hemodynamic monitoring with a pulmonary artery catheter may be necessary if hypotension persists, particularly in individuals with extensive right ventricular necrosis. The use of inhaled nitric oxide has also been investigated as a treatment option for patients with RVMI complicated by cardiogenic shock, highlighting the need for a comprehensive management approach.
Conclusion
Inferior wall infarction (IWI) is a significant cardiovascular condition that requires immediate recognition and management. This article has delved into the complexities of IWI, covering its pathophysiology, diagnostic methodologies, and treatment strategies. Grasping the intricacies of this type of myocardial infarction is crucial for healthcare professionals aiming to enhance patient outcomes and effectively manage related complications.
Key insights discussed encompass:
- The necessity of precise ECG interpretation
- The contribution of advanced imaging techniques
- The importance of timely interventions such as primary percutaneous coronary intervention (PCI)
Furthermore, the potential effects of right ventricular involvement on prognosis and management highlight the need for a holistic treatment approach. By utilizing innovative technologies like Neural Cloud Solutions’ MaxYield™ platform, healthcare providers can improve diagnostic accuracy and streamline patient care processes.
Ultimately, mastering the complexities of inferior wall infarction is vital for enhancing survival rates and quality of life for those affected. As the field of cardiovascular care continues to progress, remaining updated on the latest research and treatment guidelines will empower healthcare professionals to make informed decisions and deliver optimal care to their patients.
Frequently Asked Questions
What is inferior wall infarction (IWI)?
Inferior wall infarction (IWI) is a type of myocardial infarction that primarily affects the lower wall of the heart, often due to a blockage of the right coronary artery (RCA).
How is inferior wall infarction identified?
IWI is typically identified by ST-segment elevation in the lower leads (II, III, and aVF) on an electrocardiogram (ECG).
What causes inferior wall infarction?
The condition is caused by a significant reduction in blood flow to the lower myocardium, leading to ischemia and necrosis of cardiac tissue.
What are the risk factors associated with inferior wall infarction?
Risk factors include atherosclerosis, coronary artery disease, hypertension, and diabetes mellitus.
How does pulse pressure affect outcomes in patients with IWI?
A study showed that patients with a pulse pressure (PP) of ≤50 mmHg during hospitalization had a higher incidence of heart failure and mortality compared to those with PP >50 mmHg.
What are the typical symptoms of inferior wall infarction?
Symptoms include chest pain, often described as retrosternal and radiating to the back, and shortness of breath.
Can you provide an example of a case involving inferior wall infarction?
A 52-year-old man presented with chest pain and sweating, diagnosed with an acute lower segment myocardial event, confirmed by ECG and coronary angiography, which showed a 100% thrombotic blockage in the RCA.
How can technology improve the diagnosis of inferior wall infarction?
Integrating wearable technology with Neural Cloud Solutions' MaxYield™ platform can streamline ECG analysis, enhancing accuracy and reliability through automated labeling and data extraction.
What benefits does the MaxYield™ platform offer for ECG analysis?
The platform reduces operational costs, improves the accuracy of ECG readings, and helps healthcare professionals allocate their time and skills more effectively, ultimately leading to better patient outcomes.


