Overview
This article provides an in-depth understanding of hypokalemia and its associated ECG changes, aiming to enhance the diagnosis and management of this condition. It highlights the importance of recognizing specific ECG alterations, such as T-wave flattening and prominent U waves, which are critical for identifying hypokalemia. These changes are linked to increased risks of arrhythmias, significantly impacting patient outcomes. Thus, there is a pressing need for effective monitoring and treatment strategies to address this condition.
Introduction
Understanding the intricacies of hypokalemia is crucial for healthcare professionals, as this condition can significantly impact cardiac health. Potassium plays a vital role in maintaining normal electrical activity in the heart, making it essential to recognize the ECG changes associated with low potassium levels for effective diagnosis and management. When these changes go unnoticed, there is a potential for severe complications, including life-threatening arrhythmias and cardiac arrest. This situation raises critical questions about the necessity for vigilant monitoring and timely intervention in patients at risk.
Define Hypokalemia and Its Clinical Relevance
Hypokalemia is defined by a serum potassium level below 3.5 mEq/L, a condition vital for cardiac health. Potassium plays a crucial role in normal cellular function, particularly in cardiac myocytes, where it aids in repolarization and electrical conduction. Clinically, low potassium levels can result from various causes, including:
- Excessive gastrointestinal losses (such as vomiting and diarrhea)
- Renal losses due to diuretics
- Inadequate dietary intake
Symptoms may range from mild manifestations like fatigue and muscle weakness to severe complications, including arrhythmias and paralysis.
The clinical significance of hypokalemia ECG changes is emphasized by their effects on cardiac function. Observational studies have linked low potassium levels to hypokalemia ECG changes, which increase the risks of arrhythmias, heart failure, and mortality. For instance, research presented at the National Kidney Foundation’s 2017 Spring Clinical Meetings established a notable connection between admission serum potassium concentrations and mortality rates among hospitalized patients, emphasizing the need for careful monitoring of these levels in clinical settings.
Moreover, a large-scale study involving over 10,000 adults indicated that every 1,000 mg increase in mineral excretion was associated with an 18% reduction in cardiovascular disease risk. This evidence reinforces the importance of maintaining to prevent hypokalemia ECG changes, which can lead to adverse cardiac events. Additionally, the POTCAST trial demonstrated a 24% reduced relative risk of negative outcomes for individuals with elevated potassium levels, further underscoring the importance of effective management in cardiac health.
Leading heart specialists have noted the significant effects of low potassium levels on cardiac well-being, particularly the hypokalemia ECG changes, stressing the necessity of this mineral in medical practice. As healthcare practitioners strive to improve patient outcomes, understanding the implications of low potassium levels and their management becomes increasingly critical. Dr. Henning Bundgaard, MD, DMSc, remarked, "The improvement in outcomes was both statistically and clinically significant," underscoring the essential role of potassium levels in patient care.

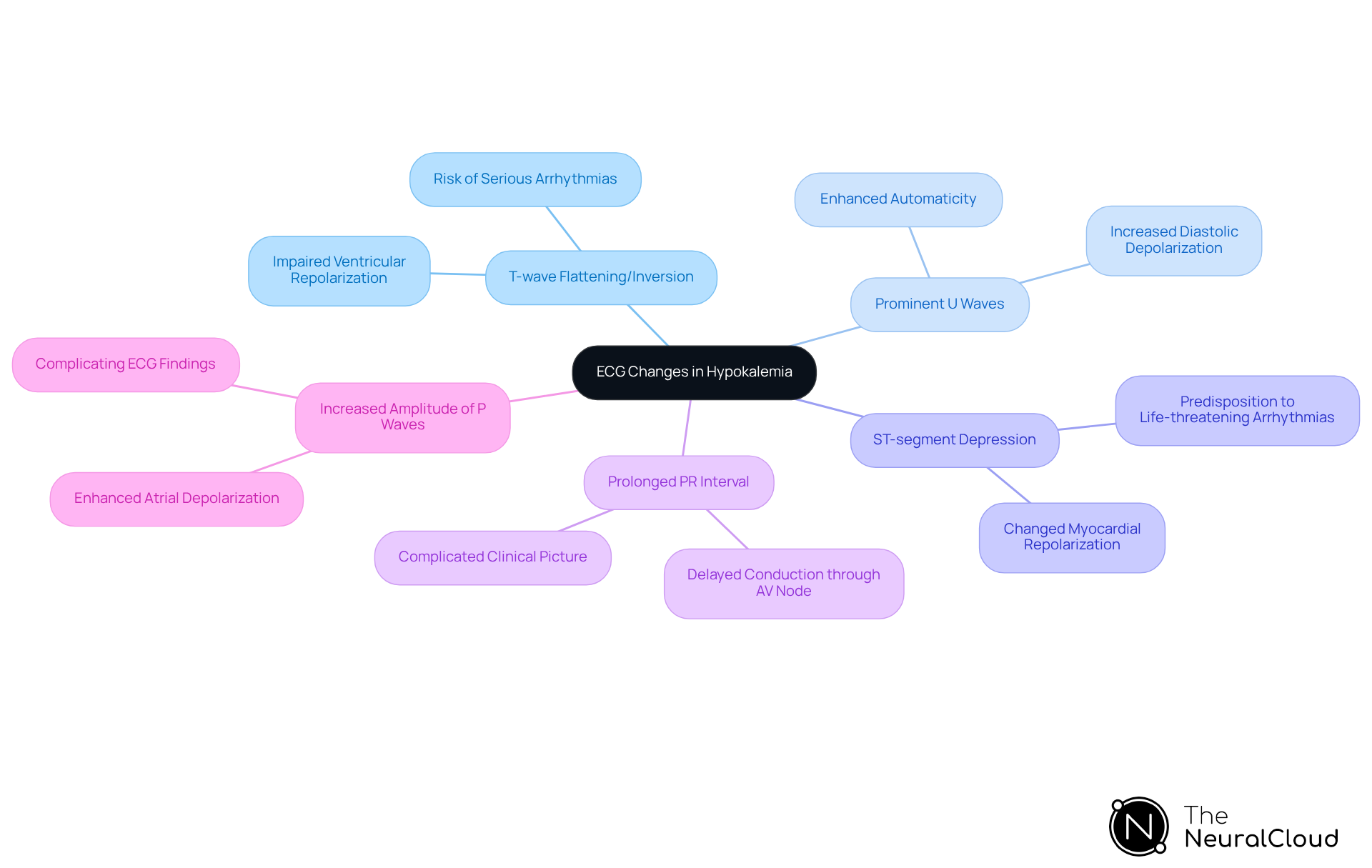
Identify ECG Changes in Hypokalemia
The precise diagnosis and management of conditions rely on hypokalemia ECG changes linked to low potassium levels. Key alterations include:
- T-wave flattening or inversion: Often the earliest change, this indicates impaired ventricular repolarization, which can lead to serious arrhythmias if not addressed promptly.
- Prominent U waves: These waves, appearing after the T wave, are a hallmark of low potassium levels and signify increased diastolic depolarization of Purkinje fibers, contributing to enhanced automaticity.
- ST-segment depression: This indicates changed myocardial repolarization and can predispose individuals to life-threatening arrhythmias, especially in severe instances where electrolyte levels decrease below 2.7 mmol/L.
- Prolonged PR interval: This change may indicate delayed conduction through the atrioventricular node, which can complicate the clinical picture.
- Increased amplitude of P waves: Enhanced atrial depolarization can occur, further complicating the ECG findings.
These modifications are generally most evident in the mid-precordial leads (V2-V4) and represent hypokalemia ECG changes, acting as crucial markers for clinicians evaluating individuals with suspected low potassium levels. Recent studies have highlighted the prevalence of hypokalemia ECG changes, emphasizing the importance of recognizing these changes in clinical practice. For instance, a case study involving a 57-year-old man with severe hypokalemia demonstrated significant T-wave inversion and prominent U waves, which normalized following potassium supplementation. Such findings emphasize the importance for healthcare professionals to be attentive in monitoring ECG changes, particularly hypokalemia ECG changes, linked to electrolyte imbalances, especially in individuals showing symptoms such as muscle weakness and arrhythmias.
Leveraging advanced platforms like MaxYield™ can significantly enhance this process. MaxYield™ automates the analysis of ECG signals, rapidly labeling P, QRS, and T wave onsets, offsets, and time-series intervals. This beat-by-beat tabulation allows for the , enabling healthcare professionals to make informed clinical decisions. By transforming noisy recordings into clear insights, MaxYield™ supports the detection of these vital ECG alterations, ultimately improving patient outcomes. As mentioned by Christopher Cardillo, DO, it is essential to consider low potassium levels if EKG findings include premature atrial contractions, premature ventricular contractions, sinus bradycardia, atrioventricular blocks, ventricular tachycardia, or ventricular fibrillation.
Interpret Clinical Implications of ECG Findings
The hypokalemia ECG changes associated with this condition carry significant clinical implications, especially when analyzed using advanced technologies like MaxYield™.
Increased risk of arrhythmias: Hypokalemia ECG changes can cause alterations in repolarization that lead to life-threatening arrhythmias, including premature ventricular contractions, ventricular tachycardia, and torsade de pointes. These arrhythmias are particularly concerning as they can escalate rapidly, necessitating immediate intervention. MaxYield™ enhances the detection of these critical changes through its advanced noise filtering and distinct wave recognition capabilities, ensuring that clinicians can respond swiftly.
- Potential for cardiac arrest: Severe potassium deficiency, defined as potassium levels falling below 2.5 mEq/L, can precipitate critical cardiac events. Data indicates that untreated severe potassium deficiency can lead to sudden cardiac death within minutes, underscoring the need for prompt medical attention. The advanced noise filtering capabilities of MaxYield™ allow for the salvage of previously obscured sections of ECG recordings, providing clearer insights into patient conditions.
Guidance for treatment: Recognizing specific ECG changes that indicate hypokalemia is crucial for clinicians to understand hypokalemia ECG changes. These changes can inform the urgency of mineral replacement therapy and other necessary interventions, allowing for timely and effective treatment strategies. According to specialists, "Raising low levels of this mineral enhances clinical results among individuals with cardiovascular disease and a high risk for ventricular arrhythmias." The automated labeling features of MaxYield™ streamline this process, enhancing compliance and scalability in cardiac data processing.
Monitoring requirements: Patients exhibiting significant ECG changes due to hypokalemia should be closely monitored for further deterioration, particularly in acute care settings, due to the hypokalemia ECG changes. Continuous ECG monitoring can help detect the onset of arrhythmias early, facilitating rapid response and management. The results from the POTCAST trial underscore the significance of optimizing minerals as an effective approach in individuals at high risk, stressing the necessity for careful monitoring and prompt intervention. With MaxYield™, healthcare professionals can leverage to revolutionize ECG analysis, ensuring enhanced clarity and efficiency in patient care.

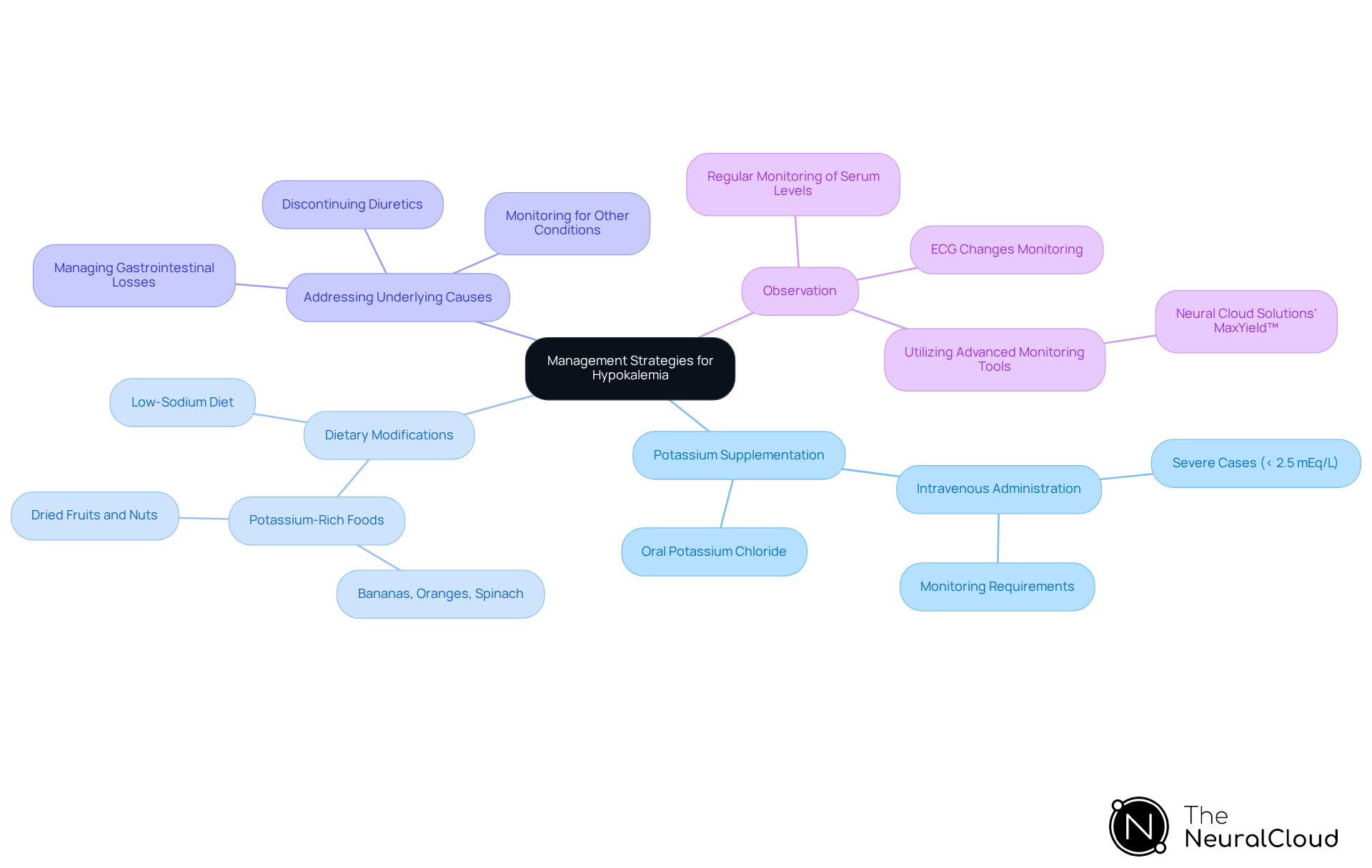
Outline Management Strategies for Hypokalemia
Effective management of hypokalemia necessitates a multifaceted approach that encompasses several strategies:
- Potassium Supplementation: Oral potassium chloride serves as the standard first-line treatment for mild to moderate hypokalemia. In cases of severe low potassium concentration, intravenous administration of potassium may be required, particularly when serum levels drop below 2.5 mEq/L, which poses risks of serious complications such as cardiac arrhythmias.
- Dietary Modifications: Encouraging patients to boost their intake of potassium-rich foods—such as bananas, oranges, spinach, and dried fruits—can significantly aid in maintaining adequate mineral levels. Research indicates that a high consumption of potassium-rich foods correlates with lower blood pressure and reduced cardiovascular risk, underscoring the importance of dietary changes in managing low potassium levels.
- Addressing Underlying Causes: It is vital to identify and treat the underlying causes of low potassium levels. This may involve discontinuing diuretics, managing gastrointestinal losses, or addressing other medical conditions that contribute to electrolyte depletion. For instance, individuals on non-potassium-sparing diuretics face a heightened risk for hypokalemia and should be monitored closely.
- Observation: Regular monitoring of serum electrolyte concentrations and the hypokalemia ECG changes is crucial to prevent recurrence and manage ongoing treatment effectively. Utilizing Neural Cloud Solutions' , which features advanced noise filtering and rapid labeling of P, QRS, and T Wave onsets and offsets, enhances the accuracy and efficiency of monitoring. This enables healthcare providers to make informed decisions based on clear, real-time data.
Integrating these strategies not only improves outcomes for patients but also aligns with the latest recommendations emphasizing the importance of managing mineral levels to avert severe health issues. For patients with chronic conditions or those undergoing long-term diuretic therapy, periodic monitoring of potassium levels is essential to ensure safety and efficacy in treatment.
Conclusion
Understanding the intricacies of hypokalemia and its associated ECG changes is essential for accurate diagnosis and effective patient management. Low potassium levels can significantly impact cardiac function, leading to critical complications such as arrhythmias and even cardiac arrest. Recognizing the importance of maintaining adequate potassium levels is crucial for healthcare practitioners, as it directly correlates with patient outcomes and overall cardiac health.
Key insights discussed include the various ECG changes indicative of hypokalemia, such as:
- T-wave flattening
- Prominent U waves
- ST-segment depression
These alterations serve as vital markers for clinicians, emphasizing the need for continuous monitoring and timely intervention. Effective management strategies, including potassium supplementation, dietary adjustments, and addressing underlying causes, are critical in preventing severe health issues related to hypokalemia.
Ultimately, the significance of understanding hypokalemia and its ECG manifestations cannot be overstated. As healthcare professionals navigate the complexities of cardiac care, prioritizing potassium management and leveraging advanced technologies like MaxYield™ can enhance diagnostic accuracy and patient outcomes. By staying informed and proactive, clinicians can ensure that they are equipped to address the challenges posed by hypokalemia, ultimately safeguarding their patients' health and well-being.
Frequently Asked Questions
What is hypokalemia?
Hypokalemia is defined as a serum potassium level below 3.5 mEq/L, which is crucial for maintaining cardiac health.
What role does potassium play in the body?
Potassium is essential for normal cellular function, particularly in cardiac myocytes, where it aids in repolarization and electrical conduction.
What are the common causes of hypokalemia?
Common causes include excessive gastrointestinal losses (such as vomiting and diarrhea), renal losses due to diuretics, and inadequate dietary intake.
What symptoms are associated with hypokalemia?
Symptoms can range from mild manifestations like fatigue and muscle weakness to severe complications, including arrhythmias and paralysis.
How does hypokalemia affect cardiac function?
Low potassium levels can lead to hypokalemia ECG changes, increasing the risks of arrhythmias, heart failure, and mortality.
What research highlights the significance of potassium levels in hospitalized patients?
Research presented at the National Kidney Foundation’s 2017 Spring Clinical Meetings established a connection between admission serum potassium concentrations and mortality rates among hospitalized patients.
What is the relationship between potassium excretion and cardiovascular disease risk?
A large-scale study involving over 10,000 adults indicated that every 1,000 mg increase in mineral excretion was associated with an 18% reduction in cardiovascular disease risk.
What did the POTCAST trial reveal about potassium levels?
The POTCAST trial demonstrated a 24% reduced relative risk of negative outcomes for individuals with elevated potassium levels, highlighting the importance of potassium management in cardiac health.
Why is it important for healthcare practitioners to monitor potassium levels?
Understanding the implications of low potassium levels and their management is critical for improving patient outcomes and preventing adverse cardiac events.


