Overview
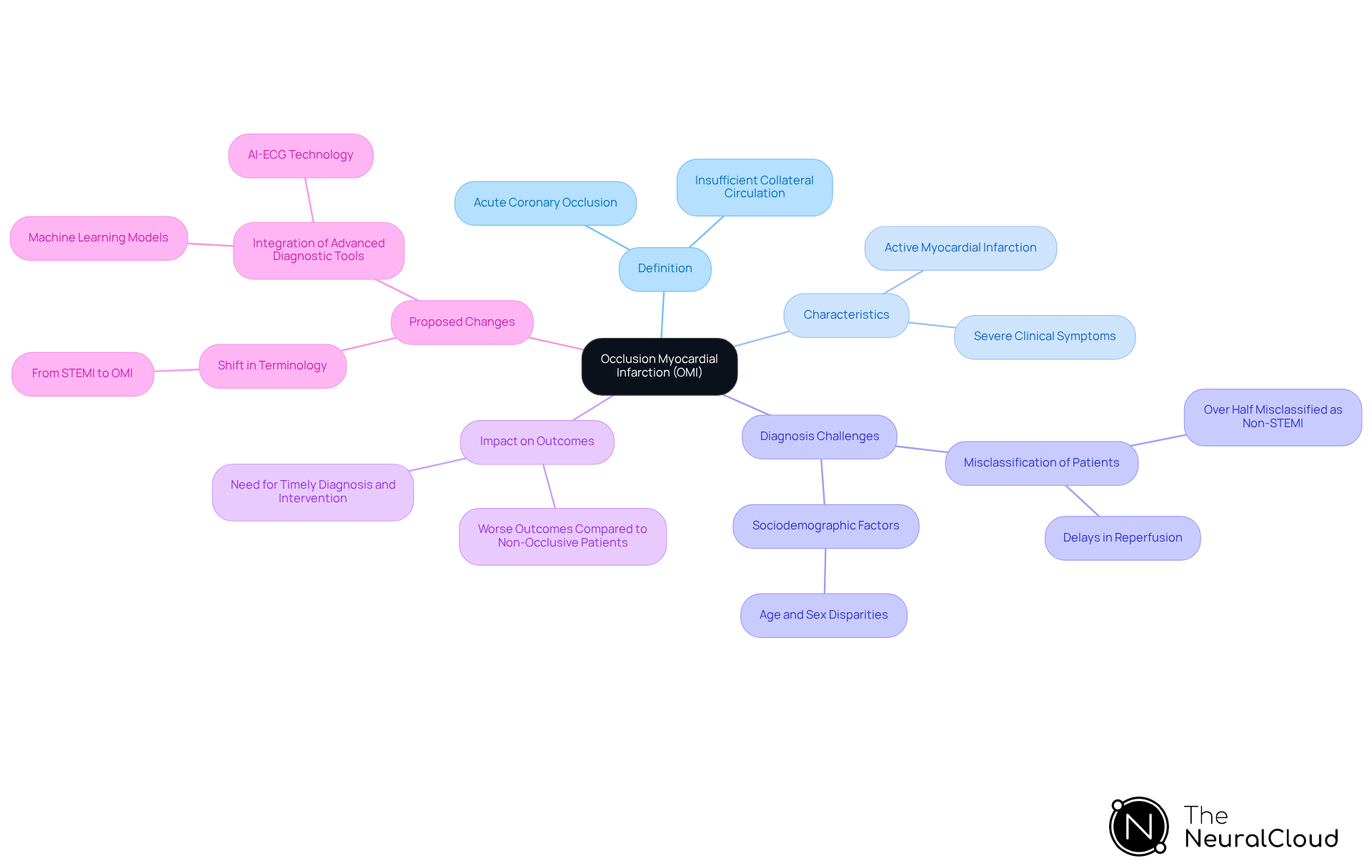
The article defines Occlusion Myocardial Infarction (OMI) as a critical condition characterized by acute coronary artery blockage that necessitates immediate medical intervention. It underscores the importance of accurate diagnosis in enhancing patient outcomes. The OMI framework shifts the focus from traditional ECG criteria to a more holistic understanding of myocardial infarction. This shift is supported by advanced diagnostic tools, including AI-driven platforms, which significantly improve the identification of occlusion cases and minimize the risk of misclassification.
Introduction
Understanding Occlusion Myocardial Infarction (OMI) is essential in the dynamic field of cardiology, where prompt diagnosis can significantly impact patient survival. This article examines the importance of OMI, defining it and discussing its clinical implications. Additionally, it explores how advanced technologies, particularly artificial intelligence, are transforming diagnostic practices. As healthcare professionals adapt to this evolving landscape, a critical question arises: how can they ensure that no patient with OMI is missed, ultimately enhancing outcomes in acute coronary syndromes?
Define Occlusion Myocardial Infarction (OMI)
Occlusion Myocardial Infarction (OMI) is characterized by an acute coronary occlusion or near-occlusion of a culprit coronary artery, which leads to insufficient collateral circulation and results in active myocardial infarction. This condition presents an immediate risk of myocardial damage due to inadequate blood flow. Unlike traditional definitions of myocardial infarction, the definition of OMI emphasizes the critical need to identify occlusion as a key factor in managing patients and treatment strategies. By concentrating on the underlying pathophysiology rather than solely on electrocardiogram (ECG) findings, the OMI framework seeks to improve diagnostic accuracy and therapeutic interventions.
Real-world examples underscore the importance of this paradigm shift. For instance, a study indicated that over half of OMI patients were misclassified as non-STEMI, resulting in significant delays in reperfusion, particularly among older individuals and those with atypical symptoms. Such delays can adversely affect outcomes, highlighting the necessity for clinicians to adopt a more nuanced understanding of myocardial infarction.
The recognition of OMI significantly impacts individual outcomes. Research shows that individuals with occlusion myocardial infarction who meet STEMI criteria frequently encounter inequitable delays in care due to sociodemographic factors such as age and sex. This underscores the importance of prompt diagnosis and intervention, as patients with OMI often exhibit more severe clinical symptoms and worse outcomes compared to those with non-occlusive culprit arteries.
Experts advocate for a shift in terminology and understanding, asserting that the OMI paradigm can substantially enhance the quality of care. As one expert stated, "Until now, clinicians never had sensitive or highly specific tools that would allow the ultra-early identification of OMI in the absence of a STEMI pattern." The integration of advanced technologies, such as Neural Cloud Solutions' MaxYield™ platform, which provides automated ECG analysis with superior noise filtering and wave recognition, has the potential to revolutionize the diagnostic process. By quickly isolating and labeling essential ECG data, MaxYield™ not only enhances clinical decision-making but also addresses the misclassification of OMI patients, ensuring they receive appropriate and timely treatment.
Trace the Evolution from STEMI to OMI
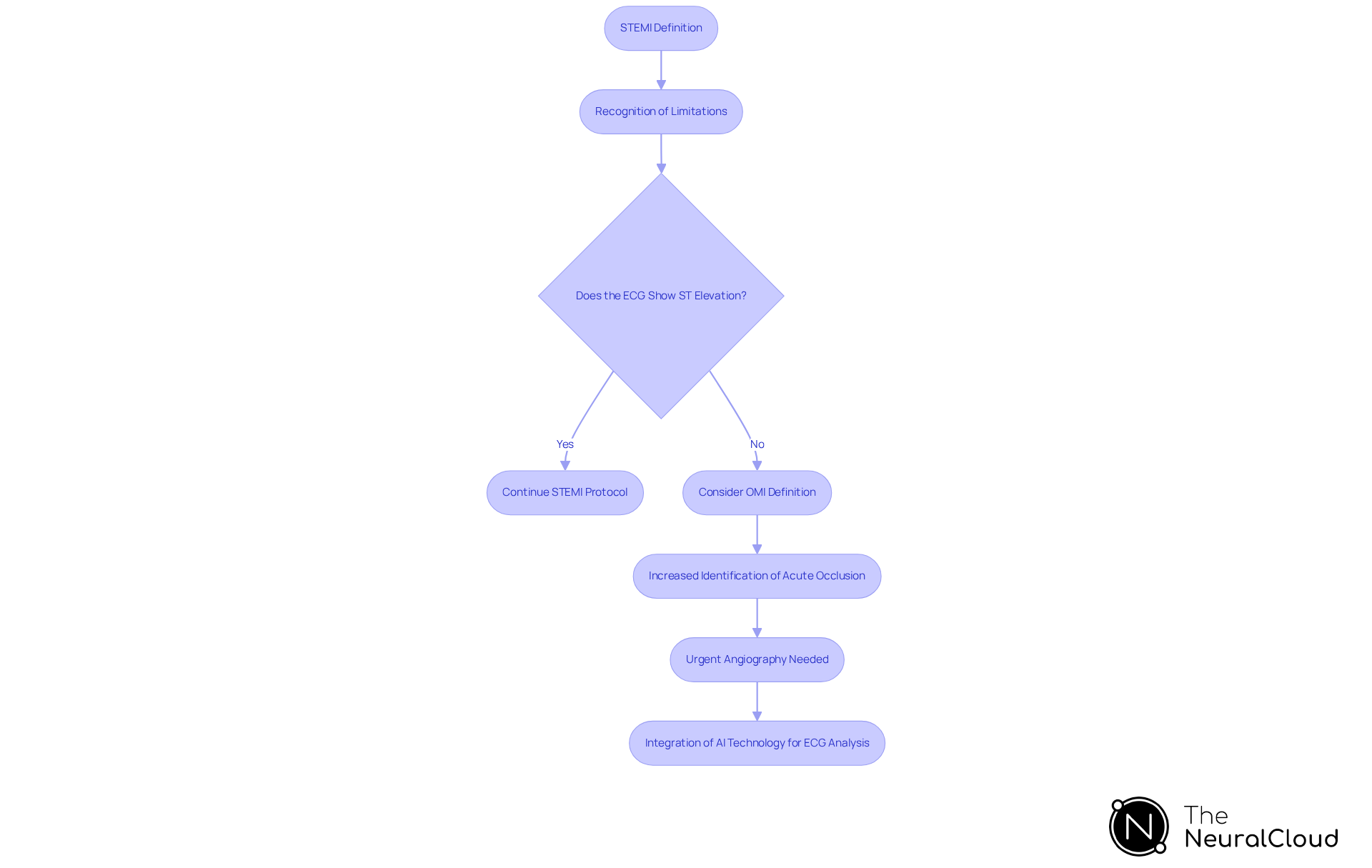
The transition from ST-Elevation Myocardial Infarction (STEMI) to Occlusion Myocardial Infarction (OMI) provides a clearer definition of OMI and marks a significant advancement in our understanding of acute coronary syndromes. Traditionally, STEMI has been defined by ST-segment elevation on the ECG, indicating a complete blockage of a coronary artery. However, recent research indicates that many individuals with acute coronary occlusion may not exhibit the classic STEMI criteria on their ECGs. This revelation has led to the acknowledgment of the definition of OMI as a more comprehensive category, which encompasses cases of acute occlusion that require urgent intervention despite the absence of ST elevation.
The definition of OMI highlights a paradigm that seeks to improve the identification of individuals at risk for myocardial damage, thereby enhancing treatment outcomes. Recent studies underscore this shift, highlighting the need for prompt angiography and potential revascularization in individuals, as per the definition of OMI, to improve clinical outcomes. A case study of an individual experiencing cardiac arrest due to anterior-inferior STEMI illustrates the critical importance of timely intervention and the role of high-sensitivity troponin I testing in emergency settings. This evolution in definitions not only reflects a deeper understanding of myocardial infarction but also emphasizes the necessity for healthcare professionals to adapt their diagnostic approaches to ensure that all individuals receive appropriate and timely care.
In this context, the integration of advanced ECG analysis technologies, such as Neural Cloud Solutions' MaxYield™, is essential. MaxYield™ leverages AI-driven automation and continuous learning models to enhance ECG analysis efficiency. This platform facilitates automated labeling and improves accuracy in identifying critical data, even amidst noise and artifacts. Such capabilities are vital for addressing the challenges posed by physiological variability and signal artifacts, ultimately aiding healthcare professionals in making timely and informed decisions, which relate to the definition of OMI.
Despite guideline recommendations for immediate and early PCI in very high-risk and high-risk NSTEMI individuals, many do not receive timely procedures. Notably, 44% of high-risk individuals underwent less than 24-hour angiography despite guideline indications, underscoring the urgent need for improved adherence to these protocols. The ECG Insights Newsletter provides valuable resources and expert insights, further assisting healthcare professionals in navigating these critical developments in cardiac care.
Explore Clinical Implications and Diagnostic Criteria of OMI
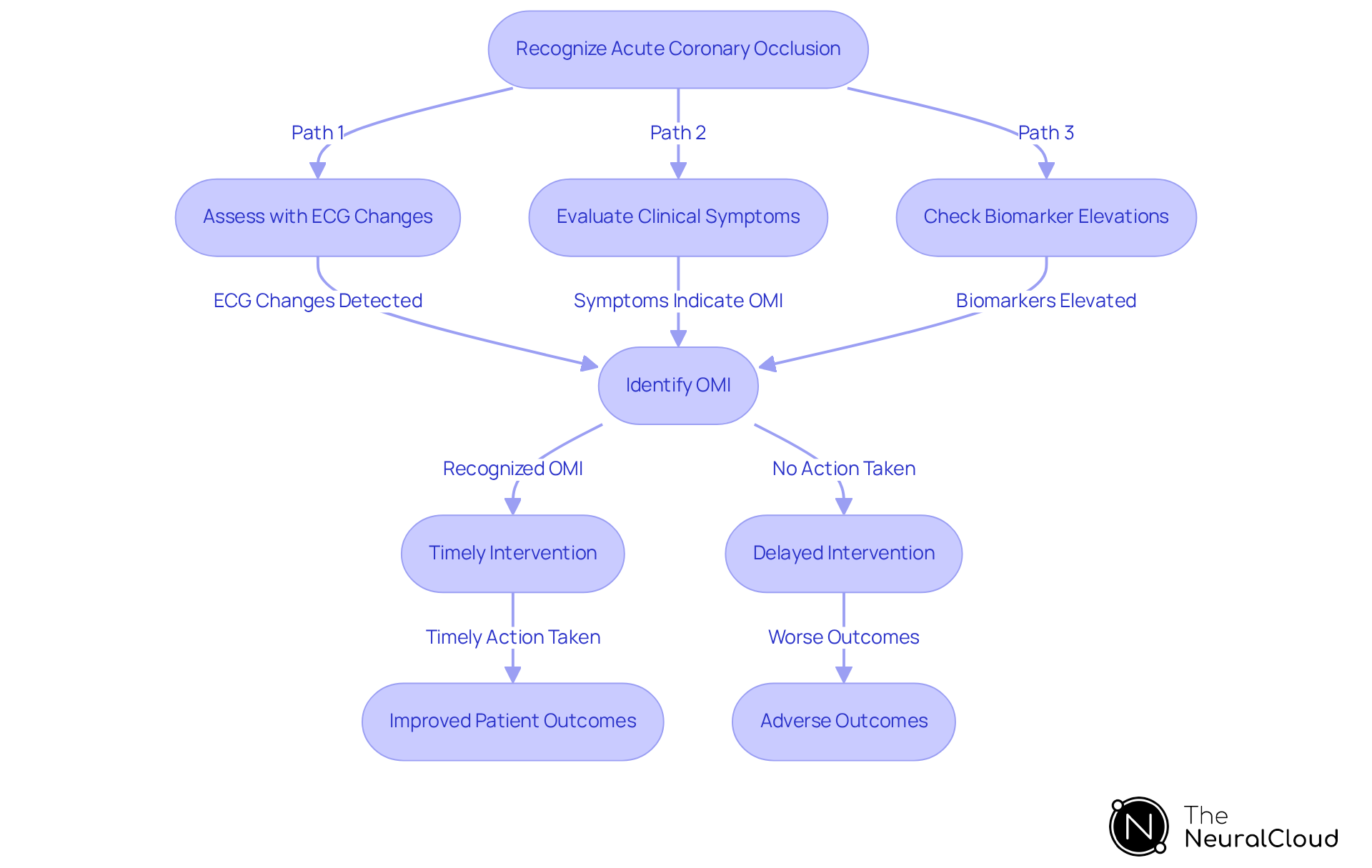
The clinical implications highlighted by the definition of OMI (Occlusion Myocardial Infarction) are significant; timely recognition can dramatically influence patient outcomes. The assessment criteria for the definition of OMI involve recognizing acute coronary occlusion, which can be evaluated through a combination of ECG changes, clinical symptoms, and biomarker elevations.
Unlike STEMI, which depends on specific ECG alterations, the definition of OMI indicates that it can be detected through clinical suspicion and advanced diagnostic techniques. Research indicates that the definition of OMI criteria improves the detection of occlusion cases, identifying approximately 30% more instances than traditional STEMI criteria. This enables earlier intervention, enhancing the chances of myocardial salvage and positive outcomes for individuals.
For example, studies show that patients identified through OMI criteria, particularly those with NSTEMI-ACO, experience similar adverse outcomes as their STEMI counterparts when revascularization is delayed. This shift in assessment standards underscores the necessity for healthcare professionals to receive training in recognizing the subtle presentations related to the definition of OMI, ensuring they are equipped to make informed decisions that can save lives.
Examine the Role of AI in OMI Detection and Analysis
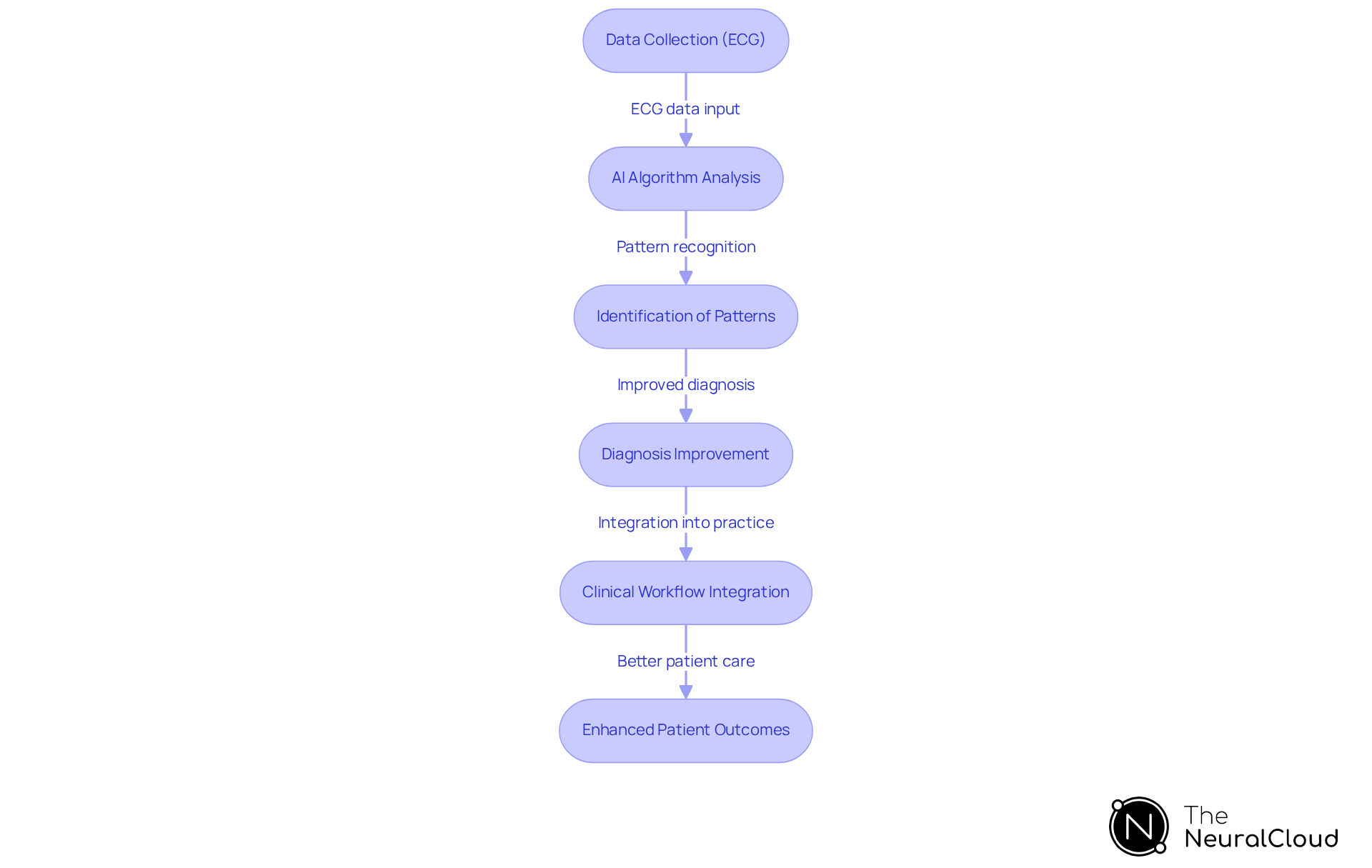
Artificial Intelligence (AI) is transforming the detection and analysis of Occlusion Myocardial Infarction (OMI) by facilitating rapid and precise interpretation of ECG data, which helps clarify the definition of OMI. Neural Cloud Solutions' MaxYield™ platform employs AI algorithms that analyze ECG data with remarkable speed and accuracy, converting lengthy and noisy recordings into clean, crisp signals. Recent studies indicate that these algorithms can identify subtle ECG patterns indicative of occlusion, even in the absence of classic ST-segment elevation. For instance, a machine learning model demonstrated a significant reduction in false positives, decreasing the rate from 59% to 29%, which underscores the improved accuracy in diagnosis.
Moreover, AI models have outperformed traditional assessment criteria, achieving sensitivity rates as high as 81% for detecting cases related to the definition of OMI, in contrast to conventional methods that frequently misclassify normal ECGs. This advancement not only streamlines the diagnostic process but also enables healthcare providers to make timely and informed decisions. By incorporating MaxYield™ into clinical workflows, cardiologists can better identify individuals at risk and initiate prompt interventions, ultimately enhancing outcomes in acute coronary syndromes.
The potential of AI in this field highlights the need for ongoing research and development to refine these algorithms and improve their clinical applicability. Additionally, the Gold Standard Methodologies employed by MaxYield™, including advanced noise filtering and automation, further enhance workflow efficiency, allowing for more effective management of patients. Testimonials from healthcare professionals underscore the transformative impact of MaxYield™ in clinical settings, emphasizing its role in improving diagnostic accuracy and patient care.
Conclusion
The concept of Occlusion Myocardial Infarction (OMI) marks a significant advancement in the understanding and management of acute coronary syndromes. This paradigm shift moves away from traditional definitions focused on ST-segment elevation, emphasizing instead the critical importance of recognizing coronary occlusion. Such a focus enhances the accuracy of diagnoses and underscores the necessity of timely intervention to improve patient outcomes.
Key insights from the article highlight the substantial impact of OMI on clinical practice:
- Misclassifying patients based on outdated definitions can result in dangerous delays in treatment, particularly for vulnerable populations.
- The integration of advanced technologies, including AI-driven ECG analysis platforms, is crucial for refining diagnostic processes.
- These innovations enable the early identification of occlusion cases, ensuring that patients receive the urgent care they require, ultimately improving survival rates and quality of care.
As the landscape of cardiac care evolves, it is essential for healthcare professionals to embrace the OMI paradigm. The ongoing development of diagnostic tools and adherence to updated clinical guidelines will be vital in reducing misdiagnoses and enhancing treatment efficiency. By prioritizing the recognition of OMI and leveraging technological advancements, the medical community can guarantee that all patients at risk of myocardial damage receive timely and appropriate care, reinforcing the importance of this critical shift in cardiology.
Frequently Asked Questions
What is Occlusion Myocardial Infarction (OMI)?
Occlusion Myocardial Infarction (OMI) is characterized by an acute coronary occlusion or near-occlusion of a culprit coronary artery, leading to insufficient collateral circulation and active myocardial infarction. This condition poses an immediate risk of myocardial damage due to inadequate blood flow.
How does OMI differ from traditional definitions of myocardial infarction?
Unlike traditional definitions, the OMI framework emphasizes the critical need to identify occlusion as a key factor in patient management and treatment strategies, focusing on the underlying pathophysiology rather than solely on electrocardiogram (ECG) findings.
Why is it important to recognize OMI in clinical practice?
Recognizing OMI is crucial because it can significantly impact individual outcomes. Patients with OMI often experience more severe clinical symptoms and worse outcomes compared to those with non-occlusive culprit arteries. Misclassification can lead to delays in reperfusion, adversely affecting patient care.
What are the consequences of misclassifying OMI patients?
Misclassification of OMI patients can result in significant delays in reperfusion, particularly among older individuals and those with atypical symptoms. These delays can negatively impact patient outcomes.
What sociodemographic factors can affect the care of OMI patients?
Sociodemographic factors such as age and sex can lead to inequitable delays in care for individuals with occlusion myocardial infarction who meet STEMI criteria.
How can the OMI paradigm enhance the quality of care?
Experts advocate for the OMI paradigm as it can improve diagnostic accuracy and therapeutic interventions, allowing for better identification and management of patients at risk for myocardial infarction.
What technological advancements are being utilized to improve OMI diagnosis?
Technologies such as Neural Cloud Solutions' MaxYield™ platform, which offers automated ECG analysis with enhanced noise filtering and wave recognition, are being integrated to revolutionize the diagnostic process and reduce misclassification of OMI patients.


