Introduction
Peaked T waves, characterized by their tall and narrow appearance on an electrocardiogram (ECG), represent more than just a technical anomaly; they often signal underlying cardiovascular issues that require attention. Understanding the causes and implications of these T wave abnormalities is essential for healthcare professionals, as they can act as early warning signs for conditions such as hyperkalemia and myocardial ischemia. However, accurately distinguishing these significant markers from other T wave variations presents a challenge.
This raises an important question: how can clinicians effectively interpret peaked T waves to enhance patient outcomes and ensure timely interventions? By focusing on the features of peaked T waves, healthcare providers can better understand their implications, leading to improved diagnostic accuracy and patient care.
Incorporating advanced ECG analysis tools can aid in this process, allowing for a more precise interpretation of T wave abnormalities. These tools not only enhance the clarity of ECG readings but also provide healthcare professionals with the necessary insights to make informed decisions. Ultimately, understanding and interpreting peaked T waves can significantly impact patient management and outcomes.
Define Peaked T Waves: An Overview
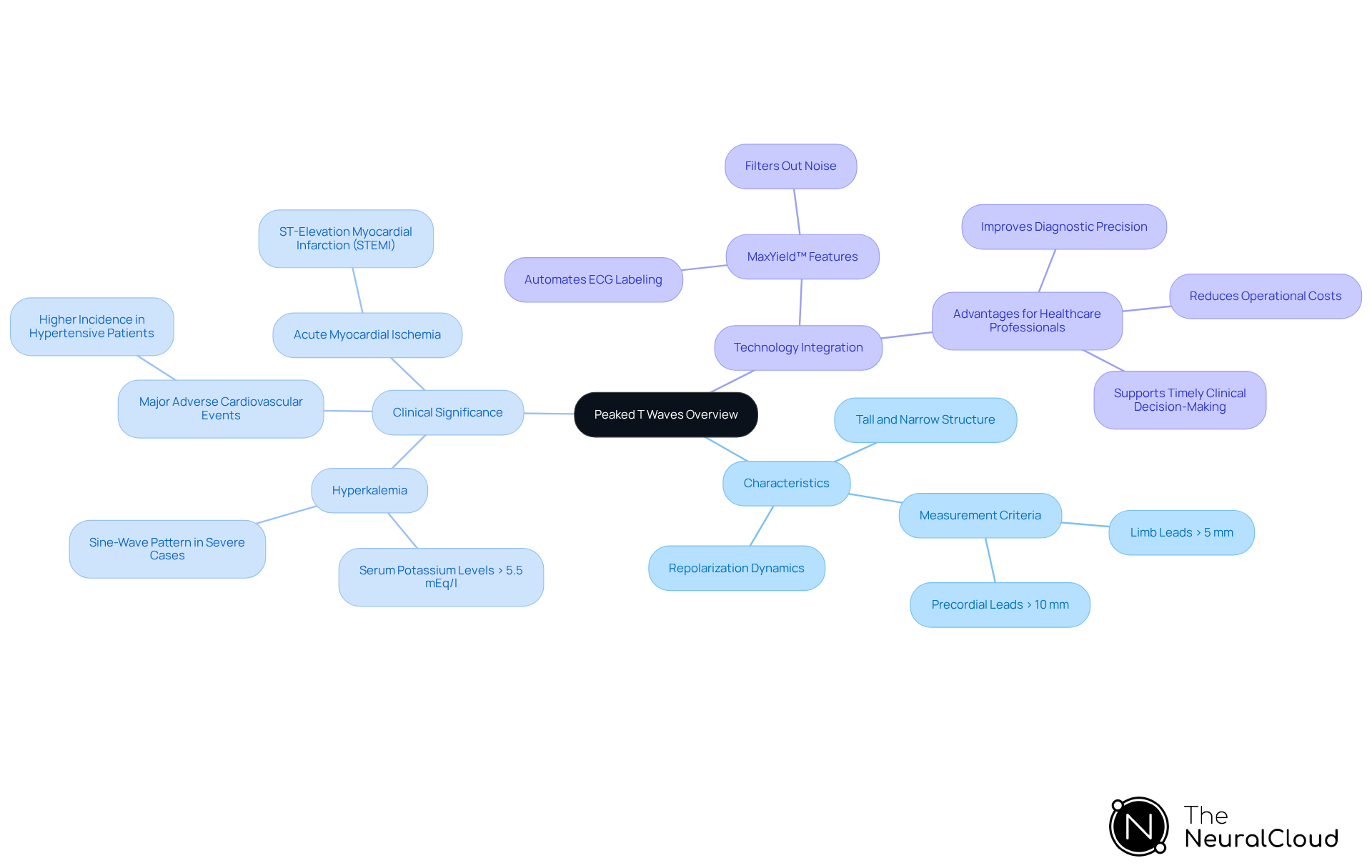
Peaked T shapes are characterized by their tall, narrow, and symmetric structure on an electrocardiogram (ECG), representing the repolarization of the ventricles. Typically, these signals exceed 5 mm in limb leads and 10 mm in precordial leads, marking a critical ECG abnormality that requires further clinical evaluation. Their presence is often linked to elevated potassium levels in the blood, a condition that contributes to what causes peaked T waves by disrupting normal cardiac repolarization dynamics. Research indicates that these elevated T shapes can serve as early indicators of hyperkalemia, prompting inquiries into what causes peaked T waves, with significant correlations identified between T shape characteristics and potassium levels.
For instance, studies have shown that hypertensive patients exhibiting irregular T patterns face a notably higher occurrence of major adverse cardiovascular events (MACE), underscoring the clinical importance of these findings. Additionally, case studies highlight what causes peaked T waves in the diagnosis of acute myocardial ischemia, particularly in ST-elevation myocardial infarction (STEMI), where localized potassium accumulation alters repolarization. In cases of severe hyperkalemia (greater than 8.0 mmol/L), a sine-wave pattern may develop, complicating both diagnosis and treatment.
Understanding the definition and characteristics of elevated T waves is essential for healthcare providers, enabling them to identify and manage potential cardiac issues effectively. The integration of wearable technology with Neural Cloud Solutions' MaxYield™ platform significantly enhances ECG analysis by automating the labeling process and filtering out noise. This advancement improves the precision and efficiency of detecting critical irregularities, such as elevated T patterns.
Features of MaxYield™:
- Automates ECG labeling
- Filters out noise for clearer signals
- Enhances detection of irregularities
Advantages for Healthcare Professionals:
- Improves diagnostic precision
- Reduces operational costs
- Supports timely clinical decision-making
By leveraging the capabilities of MaxYield™, healthcare providers can navigate the complexities of ECG analysis with greater confidence and effectiveness.
Context and Clinical Importance of Peaked T Waves
Peaked T forms are not just a technical finding; they carry significant clinical implications. In cases of hyperkalemia, identifying what causes peaked T waves can serve as an early warning sign of potentially life-threatening arrhythmias. Their appearance on an ECG may indicate that immediate medical intervention is required, particularly for patients with renal failure or those on potassium-sparing medications. Moreover, elevated T forms can also manifest in the early stages of myocardial ischemia, making them crucial indicators for cardiologists.
The MaxYield™ platform addresses the challenges of ECG analysis by leveraging advanced AI technology. It transforms lengthy and noisy ECG recordings into clean, crisp signals, significantly enhancing the clarity and speed of analysis. This capability allows healthcare providers to focus on critical data without the distraction of extraneous noise. By understanding what causes peaked T waves, healthcare professionals can prioritize patient care and make informed treatment decisions.
The integration of MaxYield™ offers several advantages for healthcare professionals:
- Automated labeling and advanced noise filtering features streamline the analysis process.
- Allows for quicker and more accurate interpretations.
- Improves patient outcomes and enhances the efficiency of clinical workflows.
- Ensures healthcare providers are equipped with the best tools to respond to urgent medical situations.

Identify Causes of Peaked T Waves: Physiological and Pathological Factors
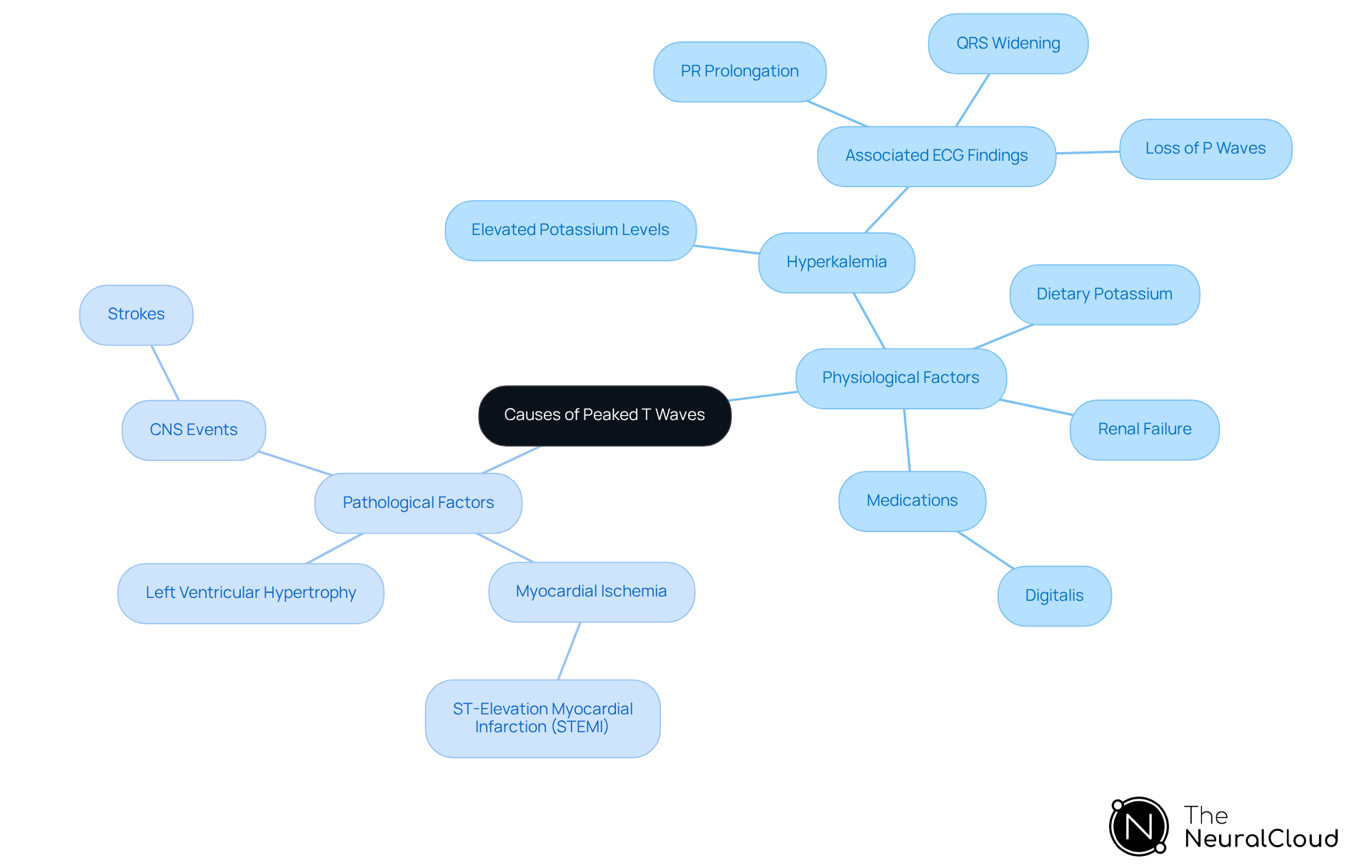
It is important to understand what causes peaked T waves, as they can arise from various physiological and pathological factors. Hyperkalemia, which is characterized by elevated potassium levels that disrupt cardiac repolarization, is the most common physiological cause of what causes peaked T waves. This condition often results from renal failure, excessive dietary potassium, or certain medications.
Pathologically, elevated T forms are frequently associated with myocardial ischemia, particularly during the early stages of ST-elevation myocardial infarction (STEMI), which raises questions about what causes peaked T waves. In fact, around 30% of patients may exhibit this ECG finding. Other pathological contributors that help explain what causes peaked T waves include left ventricular hypertrophy and central nervous system events, such as strokes.
It is crucial for clinicians to distinguish elevated T forms from normal variants, especially in acute care settings. This differentiation is vital as it guides further diagnostic testing and treatment strategies.
Management of peaked T patterns, particularly in cases of hyperkalemia, involves stabilizing the cardiac membrane, shifting potassium into cells, and removing excess potassium through various medical interventions. Understanding these causes and management strategies ultimately enhances patient outcomes.
Examine Key Characteristics and ECG Findings of Peaked T Waves
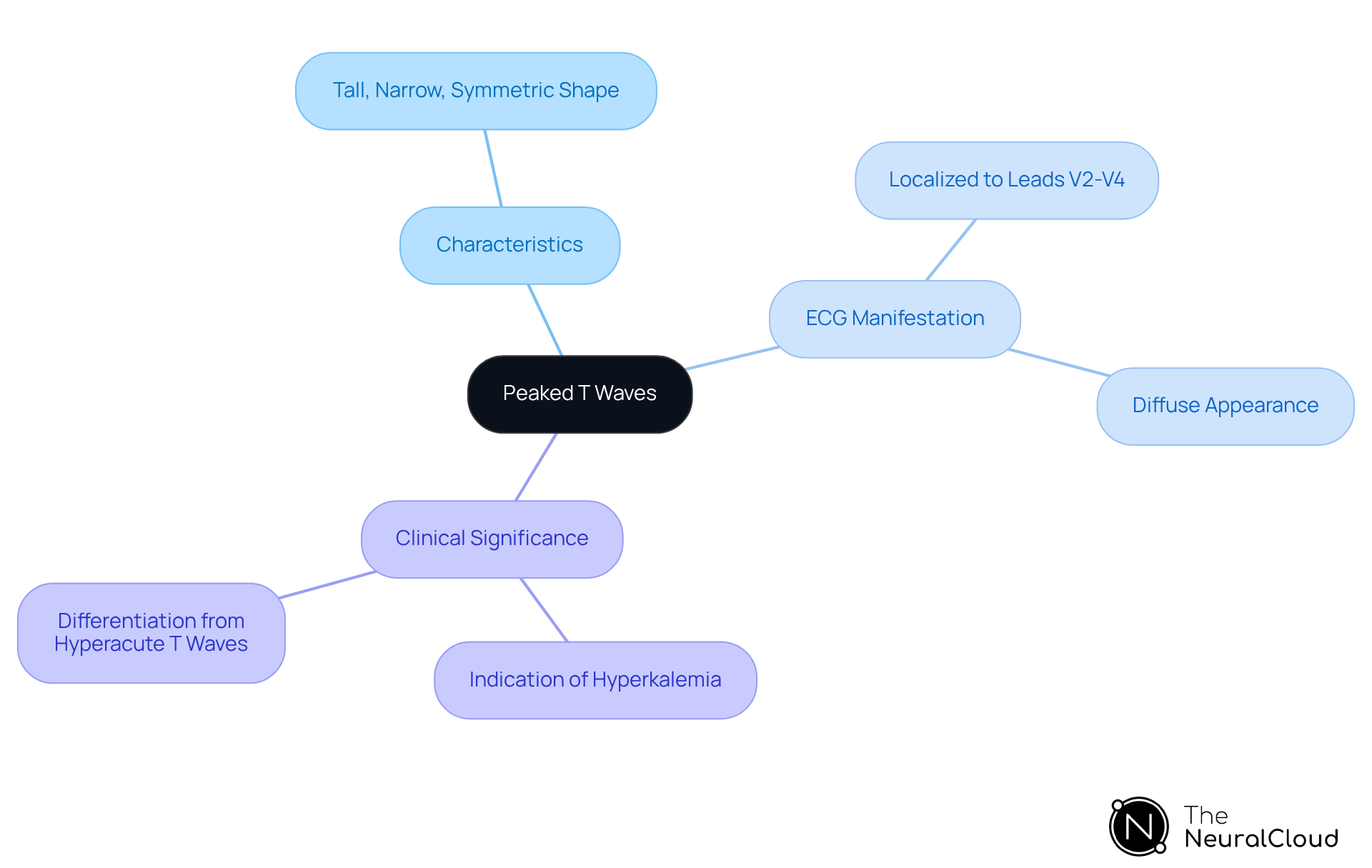
Understanding what causes peaked T waves is important, as they are notable for their tall, narrow, and symmetric shape, setting them apart from other T abnormalities. On an ECG, these signals manifest as prominent deflections following the QRS complex, often surpassing the height of the preceding QRS. Their appearance may be localized to specific leads, particularly V2-V4, which can indicate regional myocardial ischemia, or they may be diffuse, suggesting systemic issues like elevated potassium levels.
In cases of elevated potassium, what causes peaked T waves is the T deflection becoming high, slender, and uniform, especially evident in precordial leads V2-V4, where myocardial voltage vectors are most pronounced. This change is crucial, as elevated T formations are often the first ECG indication of hyperkalemia, prompting inquiries into what causes peaked T waves prior to QRS widening. Clinicians must be adept at recognizing these characteristics, as they are essential for accurate ECG interpretation and effective patient management.
The pointed T signal serves as the earliest and most reversible indicator, making its identification vital in clinical practice. Understanding what causes peaked T waves and differentiating them from other morphologies, such as hyperacute T waves, is also important; while both can signal serious conditions, hyperacute T waves are generally broader and asymmetrically peaked, frequently associated with acute myocardial infarction. Understanding these distinctions is critical for timely and effective clinical decision-making.
Conclusion
Peaked T waves are a significant clinical marker in electrocardiography, often signaling underlying health issues that need immediate attention. Their distinct tall, narrow, and symmetric appearance serves as a crucial signal for healthcare professionals, particularly in cases of hyperkalemia and myocardial ischemia. Recognizing these patterns is essential for timely intervention and effective patient care.
The article has explored various aspects of peaked T waves, including:
- Their physiological and pathological causes
- Key characteristics on ECG
- The clinical implications they carry
Elevated potassium levels and conditions such as myocardial ischemia are among the primary contributors to these abnormalities, underscoring the importance of accurate ECG interpretation. Advanced tools like the MaxYield™ platform enhance healthcare providers' ability to analyze these critical signals, ultimately improving diagnostic precision and patient outcomes.
Understanding the causes of peaked T waves is not merely an academic exercise; it is a vital component of effective clinical practice. By prioritizing the recognition and evaluation of these ECG findings, healthcare professionals can significantly impact patient management and outcomes. Embracing technology and continuous education in this area empowers clinicians to respond swiftly and accurately to the challenges posed by cardiac conditions, highlighting the importance of vigilance in monitoring and interpreting these vital signs.
Frequently Asked Questions
What are peaked T waves?
Peaked T waves are characterized by their tall, narrow, and symmetric structure on an electrocardiogram (ECG), representing the repolarization of the ventricles.
How can peaked T waves be identified on an ECG?
Peaked T waves typically exceed 5 mm in limb leads and 10 mm in precordial leads, indicating a critical ECG abnormality that requires further clinical evaluation.
What is the primary condition associated with peaked T waves?
The presence of peaked T waves is often linked to elevated potassium levels in the blood, known as hyperkalemia, which disrupts normal cardiac repolarization dynamics.
Why are peaked T waves clinically significant?
Peaked T waves can serve as early indicators of hyperkalemia and have been correlated with an increased occurrence of major adverse cardiovascular events (MACE) in patients, particularly those with hypertension.
How do peaked T waves relate to acute myocardial ischemia?
In cases of acute myocardial ischemia, particularly ST-elevation myocardial infarction (STEMI), localized potassium accumulation can alter repolarization, leading to the development of peaked T waves.
What happens in severe cases of hyperkalemia related to T waves?
In severe hyperkalemia (greater than 8.0 mmol/L), a sine-wave pattern may develop on the ECG, complicating diagnosis and treatment.
How does the MaxYield™ platform enhance ECG analysis?
MaxYield™ automates ECG labeling, filters out noise for clearer signals, and enhances the detection of irregularities, improving the precision and efficiency of ECG analysis.
What advantages does MaxYield™ offer to healthcare professionals?
MaxYield™ improves diagnostic precision, reduces operational costs, and supports timely clinical decision-making, enabling healthcare providers to navigate ECG analysis more effectively.






