Overview
The article highlights the essential ECG normal results that health tech developers must understand, including critical components such as:
- P-wave
- QRS complex
- ST segment
- T-wave
- QT interval
- Cardiac axis
- Normal heart rhythm
It underscores the significance of accurate analysis and interpretation of these elements through advanced technologies. The MaxYield™ platform stands out as a key tool, enhancing signal clarity and diagnostic precision. This improvement directly contributes to better patient outcomes in clinical settings. By utilizing the MaxYield™ platform, healthcare professionals can navigate the complexities of ECG analysis more effectively, ultimately leading to improved diagnostic capabilities.
Introduction
Understanding the intricacies of electrocardiogram (ECG) results is essential for health tech developers who aim to enhance cardiac diagnostics. As technology advances, the integration of automated systems like Neural Cloud Solutions' MaxYield™ platform promises to streamline ECG analysis. This ensures clarity and precision in interpreting vital heart signals. Yet, the complexity of normal and abnormal waveforms presents challenges. Developers must navigate issues such as noise, artifacts, and varying heart conditions to deliver reliable ECG results. This article explores the eight key ECG normal results that every health tech developer should master to improve patient outcomes and bolster clinical decision-making.
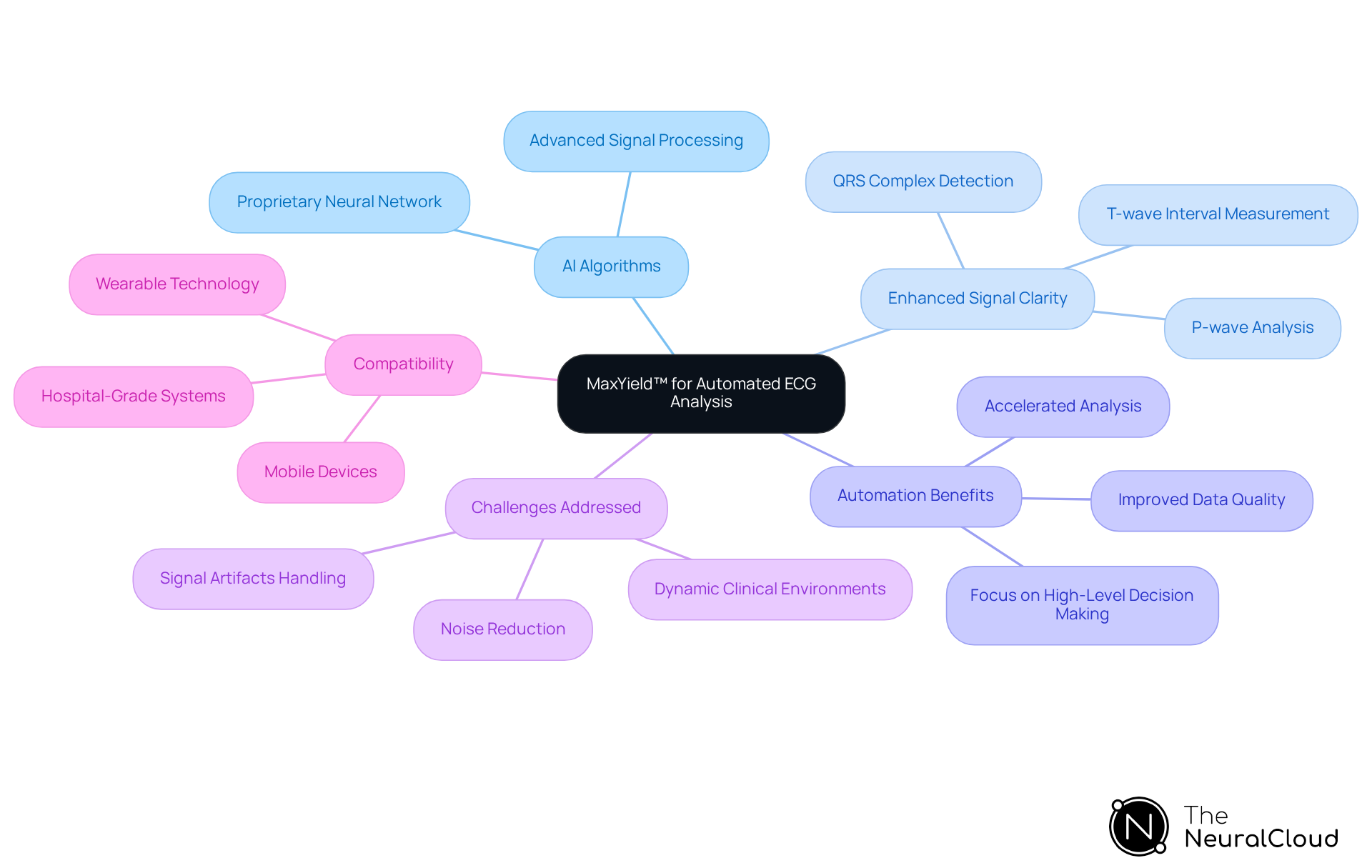
Neural Cloud Solutions: MaxYield™ for Automated ECG Analysis
Neural Cloud Solutions' MaxYield™ platform is revolutionizing ECG analysis through automation and enhanced signal clarity. This innovative platform leverages advanced AI algorithms to process over 200,000 heartbeats in under five minutes, delivering detailed beat-by-beat analysis that accurately labels critical features such as P-waves, QRS complexes, and T-wave intervals. The automation not only accelerates the analysis process but also significantly improves the quality of ECG data, leading to ECG normal results that are indispensable for healthcare professionals and researchers.
The integration of AI in ECG analysis effectively addresses common challenges, such as noise and signal artifacts, which can obscure true cardiac signals. Industry experts note that MaxYield™ enhances clinician confidence in their reviews and downstream analysis tools by delivering clearer ECG signals, which contribute to achieving ECG normal results even in noisy conditions. This capability is especially vital in dynamic clinical settings, where precise data interpretation is essential for effective care.
Furthermore, the platform's compatibility with both hospital-grade systems and mobile devices broadens its applicability, supporting better ECG signal interpretation across various monitoring settings. By focusing on automating labor-intensive tasks, MaxYield™ enables healthcare providers to concentrate on high-level decision-making. This ultimately leads to and operational efficiency.
P-Wave: Significance and Normal Characteristics
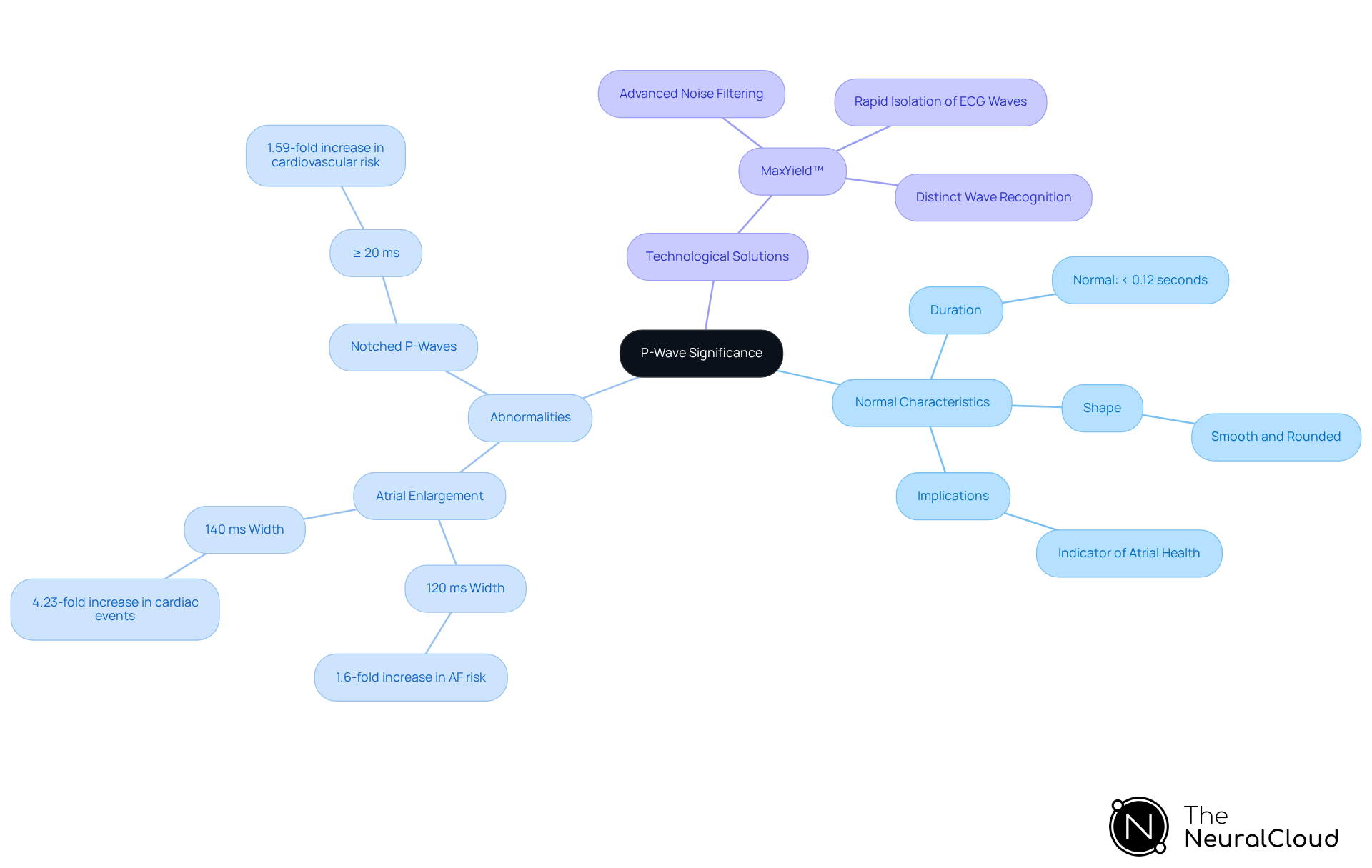
The P-wave is a critical component of the electrocardiogram (ECG), representing atrial depolarization. Typically, it manifests as a small, positive deflection, with normal P-waves measuring less than 0.12 seconds in duration and exhibiting a smooth, rounded shape. Abnormalities in P-wave morphology can signal conditions such as atrial enlargement, which is associated with increased risks of cardiovascular events. For example, a P-wave width of 120 ms or longer correlates with a 1.6-fold increase in the risk of developing atrial fibrillation, while a width of 140 ms or more is associated with a 4.23-fold increase in heart-related events. This underscores the necessity for health tech developers to ensure their ECG systems are capable of providing while accurately detecting these abnormalities.
The prevalence of P-wave abnormalities in the population is significant, with studies indicating that notched P-waves of 20 ms or longer are associated with a 1.59-fold increase in cardiovascular risk. Recognizing these abnormalities is crucial for effective heart monitoring and intervention, which makes it imperative for developers to incorporate robust algorithms capable of analyzing P-wave characteristics accurately to achieve ECG normal results. The MaxYield™ platform enhances this process through advanced noise filtering and distinct wave recognition. This allows for the rapid isolation of ECG waves even in recordings with high levels of noise and artifact.
As Robin Andlauer noted, chronic left atrial enlargement increases the risk of atrial fibrillation, highlighting the importance of precise P-wave measurement in clinical practice. To effectively implement these insights, developers should consider incorporating user manuals that detail the application of MaxYield™ features in real-world scenarios. This ensures that their systems can accurately analyze P-wave characteristics and enhance outcomes for users.
QRS Complex: Key Features and Interpretation
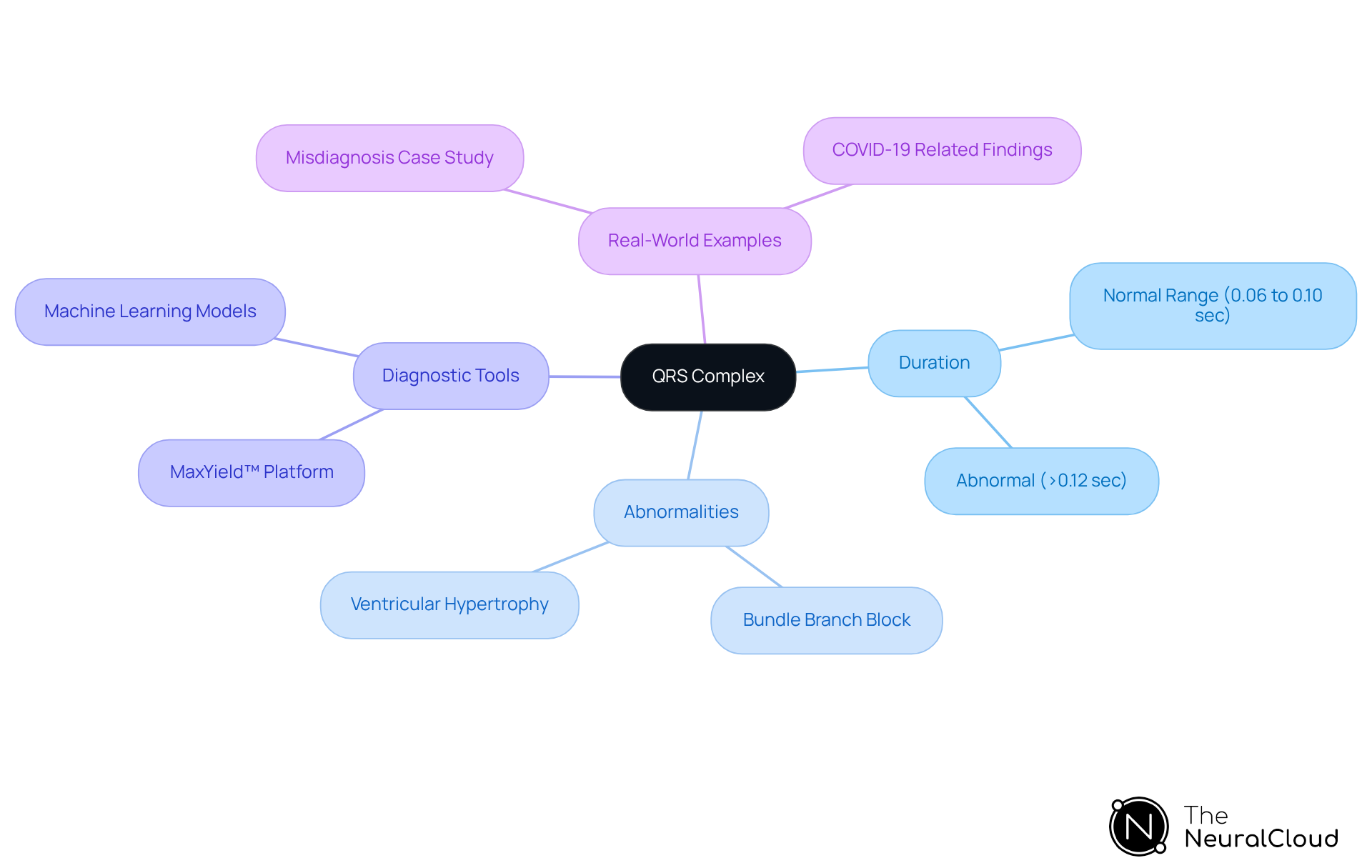
The QRS complex is a critical component of the electrocardiogram (ECG), representing ventricular depolarization and typically characterized by a sharp, tall deflection. Normal QRS duration ranges from 0.06 to 0.10 seconds, with deviations indicating potential cardiac conditions such as bundle branch blocks or ventricular hypertrophy. Notably, a QRS duration exceeding 0.12 seconds is considered abnormal and can be associated with increased mortality risk in various groups, including those with heart failure.
Accurate measurement of QRS duration is essential for effective diagnostics. Developers should prioritize algorithms that can reliably assess both QRS duration and morphology, significantly enhancing diagnostic capabilities. The MaxYield™ platform exemplifies this by utilizing advanced noise filtering and wave recognition to isolate ECG waves even in recordings with high levels of noise and artifact. This capability allows for the salvage of previously obscured sections of lengthy Holter, 1-Lead, and patch monitor recordings, ensuring that critical data is not lost. Furthermore, the continuous learning model of MaxYield™ evolves with each use, maximizing diagnostic yield and improving accuracy over time.
Recent studies have shown that machine learning models utilizing engineered features related to QRS polarity direction can improve the differentiation between wide complex tachycardia (WCT) types, achieving high accuracy in clinical settings. WCT is characterized by a and a rate of ≥100 bpm, making precise measurement crucial.
Real-world examples underscore the importance of precise QRS duration measurement. In one case, a 79-year-old woman with a dual-chamber pacemaker was initially misdiagnosed with nonsustained ventricular tachycardia (VT) based on her ECG. Upon closer examination, her irregular QRS complexes were identified as paced rhythms, highlighting the need for careful interpretation of QRS morphology. Moreover, the occurrence of bundle branch blocks in ECG readings requires that health tech developers create robust algorithms capable of distinguishing these conditions to enhance outcomes for individuals. To enhance diagnostic accuracy, developers are encouraged to incorporate features that account for variations in QRS morphology and to seek expert insights on the significance of QRS duration in clinical practice.
ST Segment: Normal Values and Clinical Implications
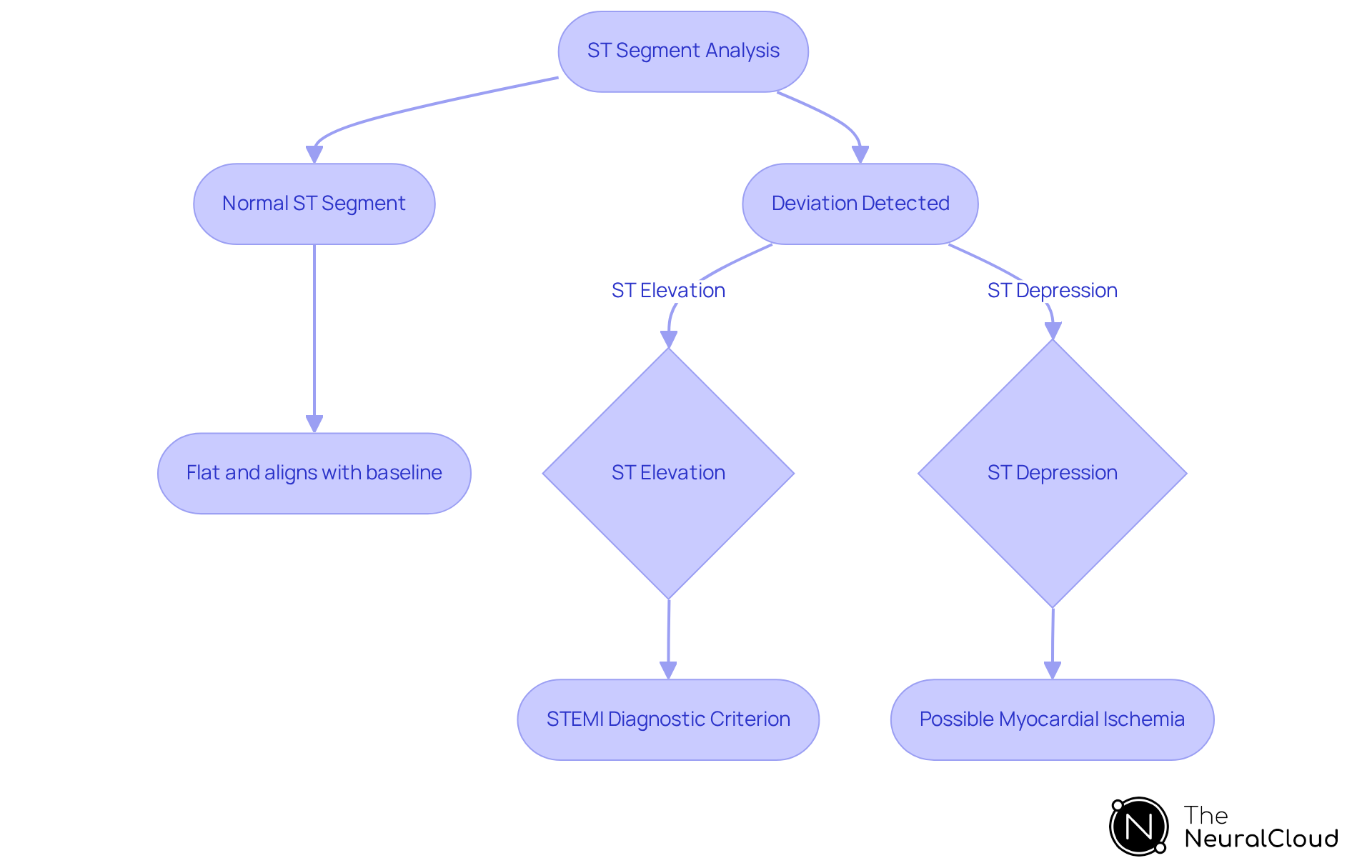
The ST segment, which follows the QRS complex, signifies the interval between ventricular depolarization and repolarization. A normal ST segment is typically flat and aligns with the baseline. Deviations from this baseline, such as ST elevation or depression, are critical indicators of myocardial ischemia or infarction. For instance, ST segment elevation of at least 1 mm in two contiguous leads is a key diagnostic criterion for ST-elevation myocardial infarction (STEMI). In clinical practice, precise identification of these deviations is essential, as can greatly influence individual outcomes.
Health tech developers must ensure their ECG systems are equipped to identify these changes effectively, as studies indicate that prompt recognition of ST segment alterations can lead to improved survival rates. Furthermore, cardiologists emphasize that while elevated troponin levels indicate myocardial injury, they do not reliably identify patients needing urgent intervention, underscoring the importance of comprehensive ECG analysis. By integrating advanced algorithms capable of detecting ST segment deviations, developers can enhance diagnostic accuracy and support clinicians in making informed decisions swiftly.
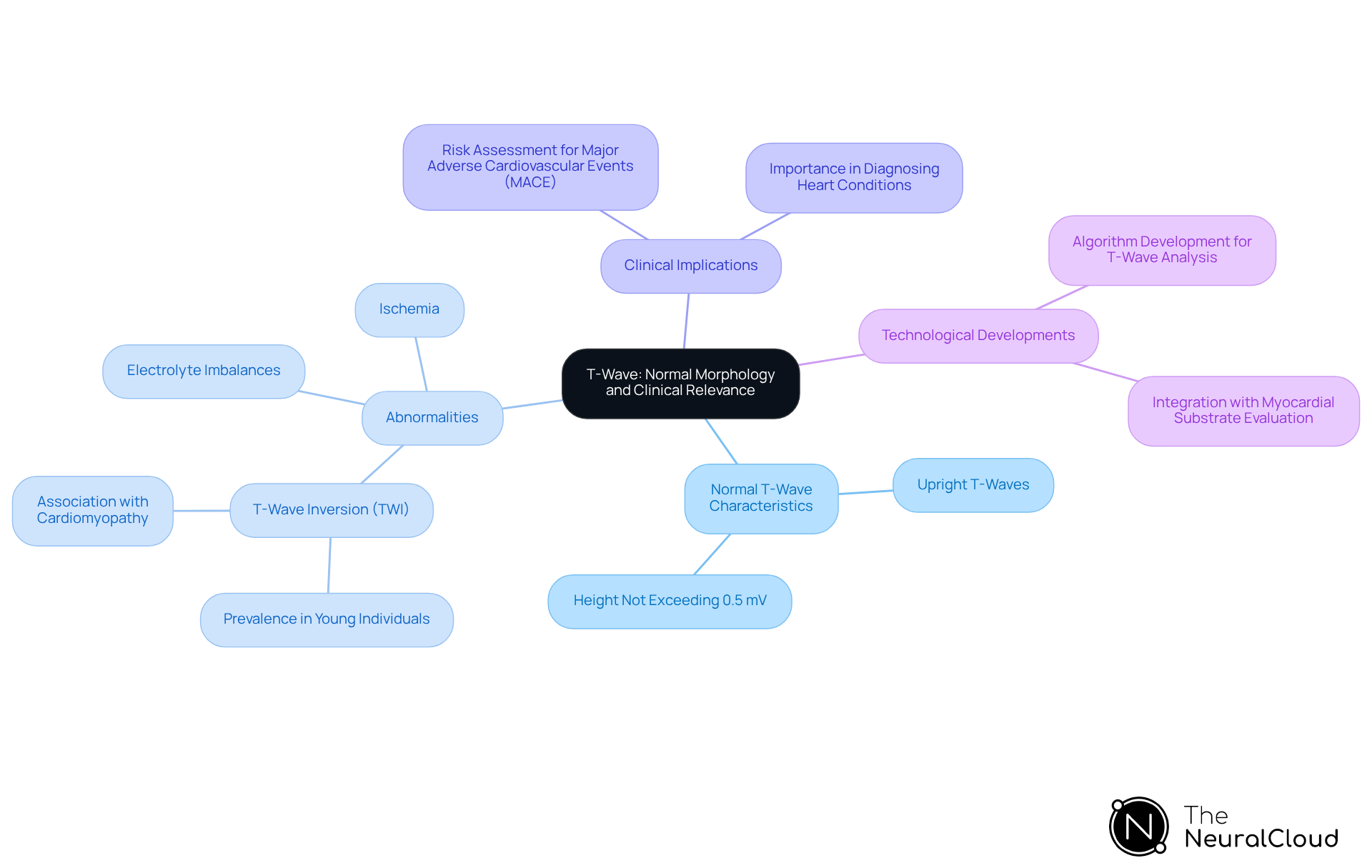
T-Wave: Normal Morphology and Clinical Relevance
The T-wave is a critical component of the electrocardiogram (ECG), representing ventricular repolarization. It typically appears as a smooth, rounded wave following the QRS complex, and the presence of upright T-waves not exceeding 0.5 mV in height indicates ECG normal results in most leads.
Abnormalities in T-wave morphology can indicate various heart conditions, including electrolyte imbalances and ischemia. For instance, studies suggest that T-wave inversion (TWI) is common in approximately 2% of young individuals undergoing heart evaluations, with 13% of those identified with cardiomyopathy.
This highlights the necessity for developers to create algorithms capable of accurately assessing to enhance diagnostic precision. Furthermore, combining T-wave analysis with myocardial substrate evaluation has shown improvements in risk assessment for major adverse cardiovascular events (MACE), underscoring the clinical significance of T-wave characteristics in predicting heart risks.
As the occurrence of abnormal T-wave features remains a concern, particularly in groups at risk for sudden heart failure, the development of advanced ECG systems that can accurately assess these features is crucial for achieving ECG normal results and improving outcomes for individuals.
QT Interval: Normal Duration and Its Importance
The QT interval is a critical measurement in electrocardiography, representing the duration from the onset of the QRS complex to the conclusion of the T-wave. This interval indicates the total time required for ventricular depolarization and repolarization, with a , contingent on the heart rate. Prolonged QT intervals are associated with an elevated risk of life-threatening arrhythmias, such as torsade de pointes, which can lead to sudden cardiac events. Recent studies indicate that the prevalence of prolonged QT intervals in the general population is significant, necessitating vigilant monitoring.
Health tech developers must prioritize the accuracy of their systems in measuring and interpreting QT intervals to enhance safety and clinical outcomes. As cardiologists emphasize, early detection of QT prolongation can be pivotal in preventing severe complications, underscoring the need for [reliable ECG analysis tools](https://theneuralcloud.com/technician-solution) in clinical practice. Furthermore, it is important to note that the QT measurement capabilities of wearables are less well documented, which highlights the necessity for robust systems in this area.
Additionally, the Bazett formula has been shown to result in longer QT prolongation periods than other formulas in 40.9% of ECGs examined, raising concerns about measurement accuracy. As Sarah Handzel, BSN, RN, stated, 'Early detection and identification of QT interval changes can be key to saving an individual's life.' This reinforces the critical need for effective monitoring solutions.
Devices like AliveCor's KardiaMobile 6L, which enable individuals to monitor their QT interval, exemplify the practical applications of technology in this field. Moreover, integrating advanced solutions like MaxYield™ can significantly enhance ECG analysis by filtering noise and accurately recognizing waveforms, thereby improving the reliability of QT interval measurements and overall patient safety.

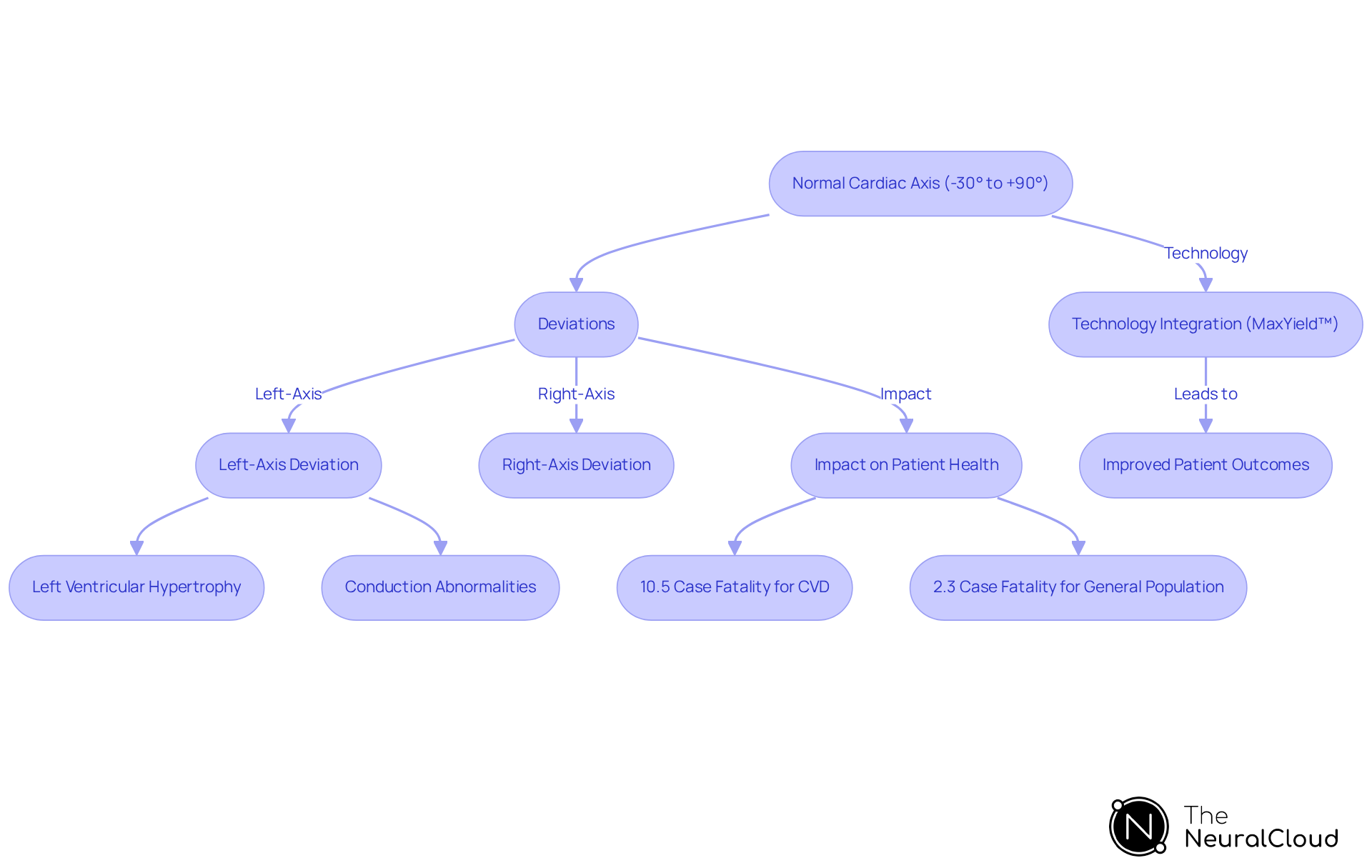
Cardiac Axis: Understanding Normal Orientation
The heart axis indicates the predominant direction of the heart's electrical activity during depolarization, typically ranging from -30° to +90°. Deviations from this range may indicate various cardiac conditions, such as left or right ventricular hypertrophy and conduction abnormalities. For instance, left-axis deviation can be associated with specific anatomical changes, as seen in individuals with a mean electrical axis of 51.8° (± 26.6°) and corresponding CT anatomical axes averaging 20.9° and 50.5°. Such deviations can significantly affect patient health, as evidenced by the increased case fatality rate of 10.5% for those with cardiovascular disease (CVD), compared to 2.3% for the general population.
Developers should prioritize algorithms that accurately calculate and interpret the heart axis, as this capability is crucial for enhancing diagnostic precision. By integrating advanced ECG systems like MaxYield™, which utilizes AI technology to transform lengthy and noisy ECG recordings into clean signals, developers can markedly improve the clarity and speed of heart evaluations. MaxYield™ offers beat-by-beat analysis, providing detailed insights into P-wave, QRS complex, and T-wave onsets and offsets. Healthcare professionals stress the importance of recognizing these deviations, noting that arrhythmia can manifest with heart rates ranging from 350 to 650 beats per minute, often accompanied by irregular rhythms and absent P waves. Notably, arrhythmia was identified in 16.7% of hospitalized individuals with COVID-19, highlighting its prevalence.
By utilizing MaxYield™ to effectively measure the heart axis and emphasize potentially significant ECG data, developers can enhance patient outcomes and ensure more reliable heart assessments. The platform's ability to deliver not only aids healthcare professionals in making informed decisions but also contributes to improved patient care and safety.
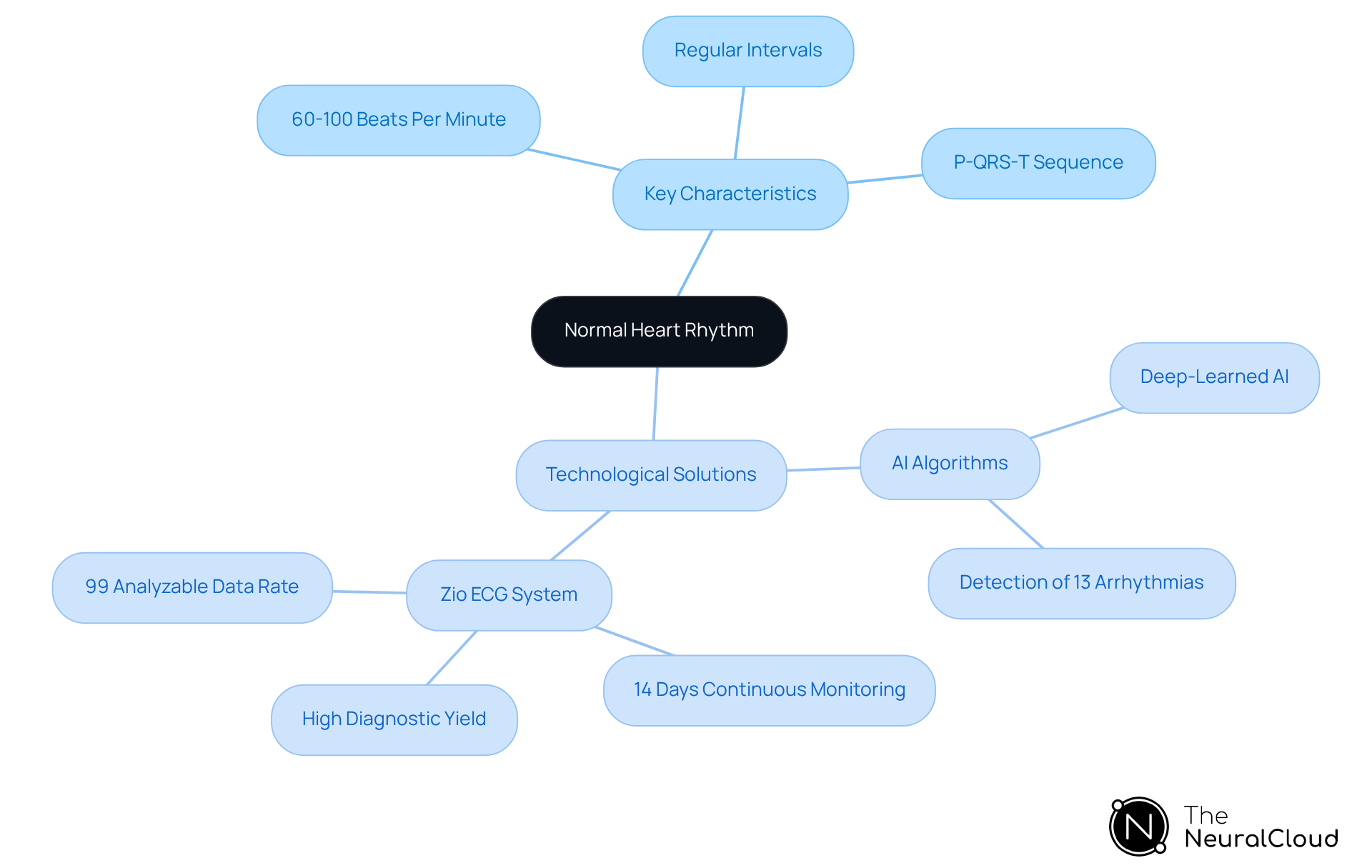
Normal Heart Rhythm: Characteristics and Recognition
A normal heart rhythm is characterized by a consistent rate of 60 to 100 beats per minute, regular intervals between beats, and a distinct P-QRS-T sequence. Deviations from this established pattern may indicate arrhythmias or other heart conditions. With (AF) impacting approximately 37.5 million people globally, accurately identifying and differentiating between normal and abnormal rhythms is essential for improving diagnostic accuracy. Health tech developers must ensure their systems are capable of effectively recognizing these variations.
For example, advanced ECG systems like the Zio ECG Recording and Analysis System employ AI algorithms to detect 13 types of arrhythmias. This technology achieves a diagnostic yield that significantly decreases the likelihood of retesting. Such capability is crucial as the prevalence of cardiac arrhythmias continues to rise, with projections suggesting a 60% increase in AF cases by 2050.
By focusing on the characteristics of normal heart rhythms and integrating robust detection systems, developers can contribute to improved outcomes for patients with ECG normal results and enhance clinical workflows. This approach not only enhances diagnostic precision but also supports healthcare professionals in managing and treating heart conditions more effectively.
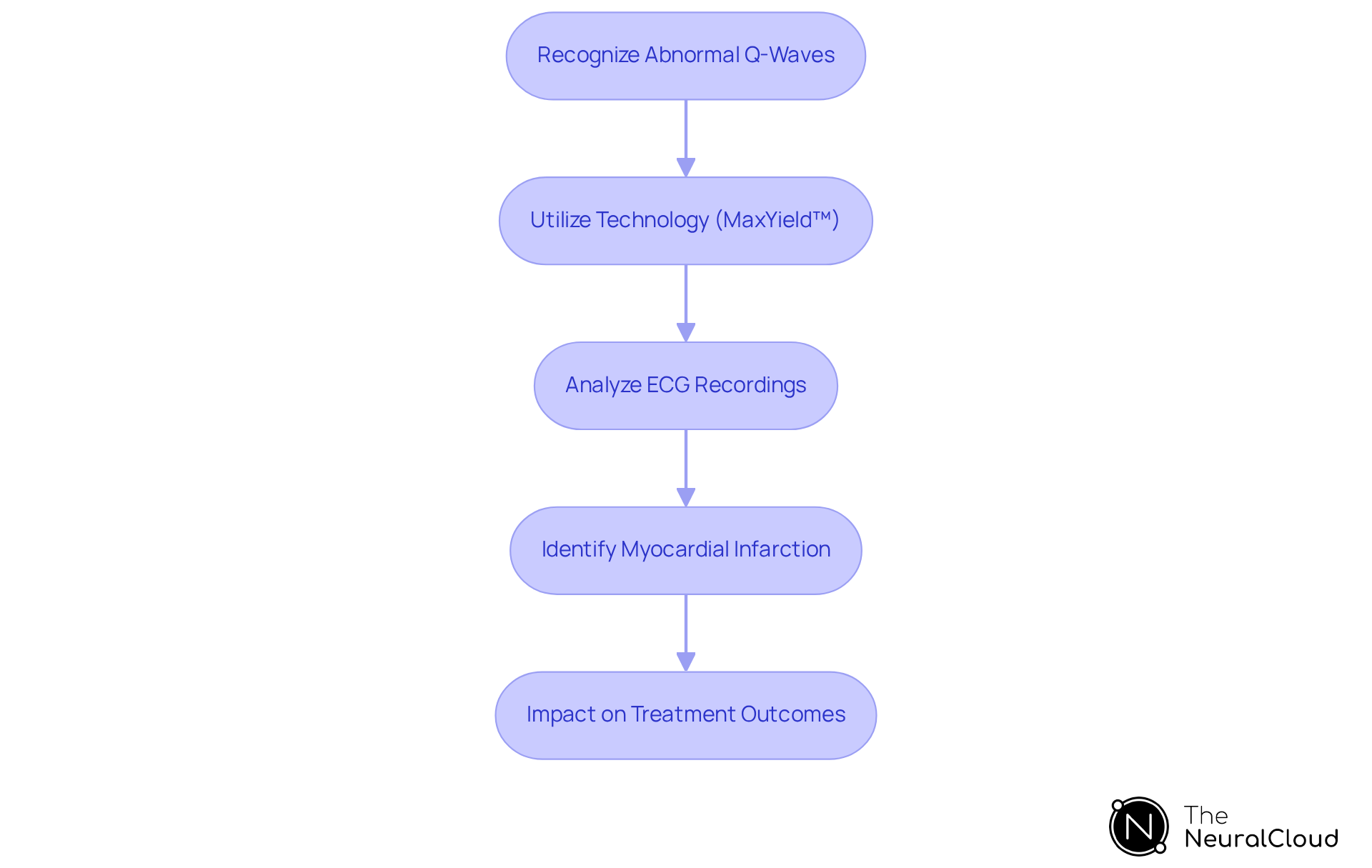
Abnormal Q-Waves: Indicators of Myocardial Infarction
Abnormal Q-waves are distinguished by their increased width and depth compared to normal Q-waves, serving as significant indicators of previous myocardial infarction (MI). Their presence in specific leads correlating with the affected heart region is crucial for accurate diagnosis. For instance, studies have shown that models with Q-waves in leads II + aVF exhibit a remarkable specificity of 100% for identifying myocardial scars. This underscores the necessity for developers to create algorithms that can reliably detect these abnormalities. The identification of abnormal Q-waves can profoundly impact treatment outcomes, as timely recognition allows for appropriate interventions.
In 2025, advancements in ECG analysis technology, such as Neural Cloud Solutions' MaxYield™, will further refine the detection of abnormal Q-waves, enhancing diagnostic accuracy. MaxYield™ utilizes cutting-edge AI technology to transform lengthy and noisy ECG recordings into clean, crisp signals, enabling rapid beat-by-beat analysis. Key features of MaxYield™ include:
- Transformation of noisy ECG recordings into clear signals.
- Rapid analysis of 200,000 heartbeats in less than 5 minutes.
- Detailed output of P-wave, QRS complex, and T-wave onsets and offsets.
As Dr. Han Kim notes, "No one has fully understood how often these heart attacks occur and what they mean in terms of prognosis." Understanding the implications of these findings is essential, particularly as (UMIs) remain vague. Moreover, individuals with non-Q-wave attacks have a 17-fold greater risk of death from heart issues, emphasizing the urgency of prompt detection. By concentrating on the advancement of advanced detection algorithms, health tech creators can greatly aid in enhancing care and outcomes, utilizing platforms like MaxYield™ to improve clarity and efficiency in ambulatory waveform processing.
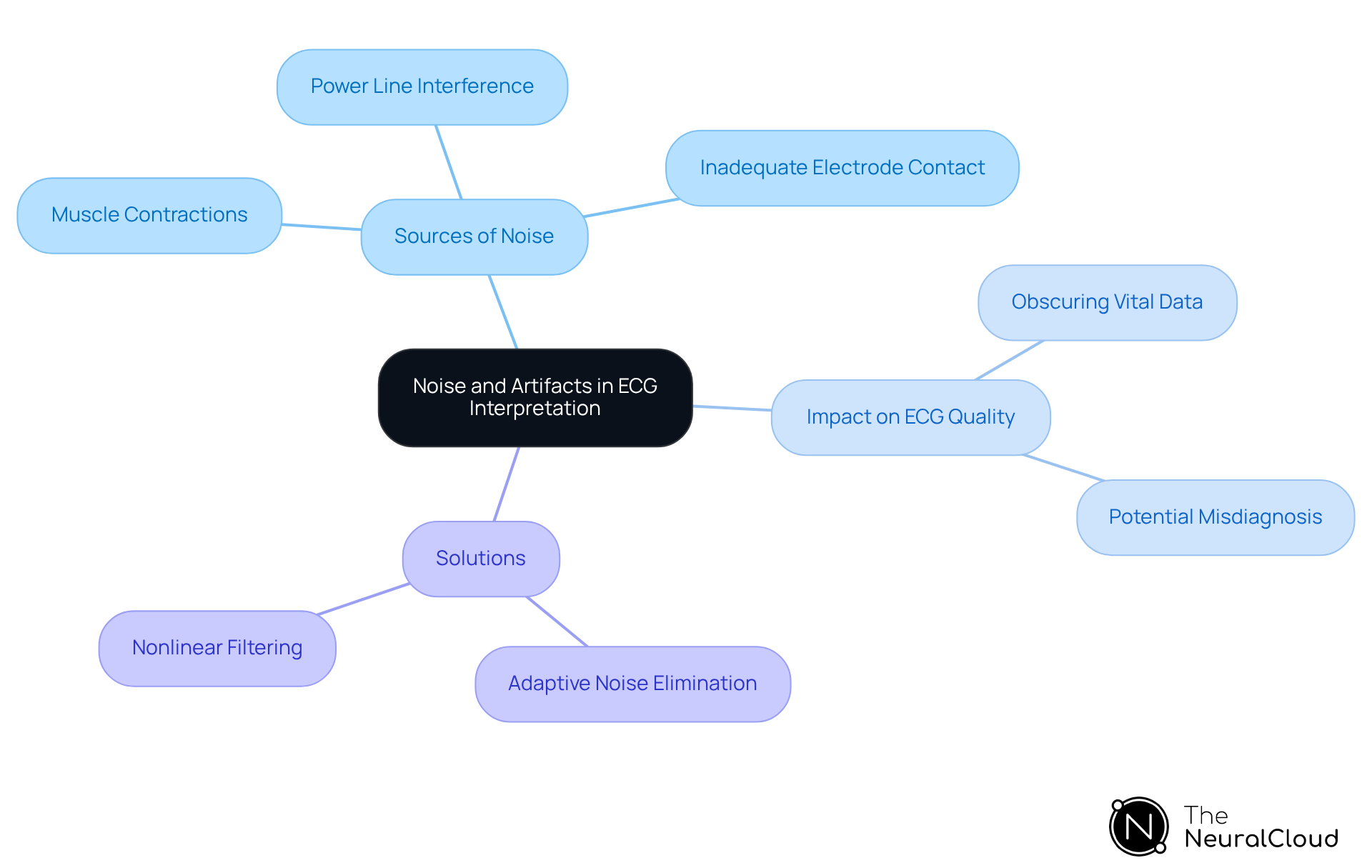
Noise and Artifacts: Impact on ECG Interpretation
Noise and artifacts significantly compromise the integrity of ECG signals, often leading to misinterpretation and potential misdiagnosis. Research indicates that improper grounding and electrical interference can produce a fuzzy baseline on the ECG trace, complicating accurate readings. Common sources of noise include:
- Muscle contractions
- Power line interference
- Inadequate electrode contact
These factors can obscure critical information regarding an individual's health status. In fact, studies have shown that high-resolution ECG signals are essential for accurately measuring cardiac abnormalities, as poor signal quality can lead to erroneous conclusions.
Healthcare professionals emphasize the importance of addressing these challenges. Experts note that artifacts can obscure vital data, making effective noise reduction techniques crucial for reliable ECG analysis. Developers are encouraged to prioritize the creation of advanced algorithms capable of filtering out these interferences. Techniques such as:
- Adaptive noise elimination
- Nonlinear filtering
have shown promise in enhancing signal quality, thereby improving diagnostic accuracy. By focusing on these innovations, health tech developers can significantly enhance clinical decision-making and patient outcomes.
Conclusion
The insights provided in this article emphasize the crucial role of understanding key ECG normal results for health tech developers. By focusing on the intricacies of various ECG components—such as the P-wave, QRS complex, ST segment, T-wave, QT interval, cardiac axis, and normal heart rhythm—developers can create innovative solutions that enhance diagnostic accuracy and improve patient care. The integration of advanced technologies like Neural Cloud Solutions' MaxYield™ streamlines ECG analysis and ensures that healthcare professionals receive clear and actionable data.
Key arguments highlight the importance of precise measurements and the ability to detect abnormalities in ECG readings. Each component discussed, from the significance of P-wave characteristics to the implications of abnormal Q-waves, underscores the necessity for robust algorithms that can filter noise and enhance signal quality. The potential of AI in revolutionizing ECG interpretation is also stressed, allowing for rapid analysis and improved clinical decision-making.
In light of these findings, it is imperative for health tech developers to prioritize the advancement of ECG technologies. By embracing innovations that address the challenges of noise and artifacts while ensuring accurate detection of critical abnormalities, they can significantly enhance the quality of cardiac care. The ongoing commitment to refining ECG analysis tools is essential, not only for improving diagnostic outcomes but also for ultimately saving lives through timely and effective interventions.
Frequently Asked Questions
What is MaxYield™ and how does it improve ECG analysis?
MaxYield™ is a platform developed by Neural Cloud Solutions that automates ECG analysis using advanced AI algorithms. It processes over 200,000 heartbeats in under five minutes, providing detailed beat-by-beat analysis and improving signal clarity, which leads to more accurate ECG results.
What are the benefits of automating ECG analysis with MaxYield™?
Automation accelerates the analysis process, enhances the quality of ECG data, and helps healthcare professionals achieve ECG normal results, even in noisy conditions. This is crucial for effective patient care and decision-making.
How does MaxYield™ handle noise and signal artifacts in ECG readings?
The platform utilizes advanced noise filtering and wave recognition to isolate ECG waves, effectively addressing common challenges such as noise and artifacts that can obscure true cardiac signals.
What is the significance of the P-wave in an ECG?
The P-wave represents atrial depolarization and is a critical component of the ECG. Normal P-waves are less than 0.12 seconds in duration and have a smooth, rounded shape. Abnormalities in P-wave morphology can indicate conditions like atrial enlargement and increased cardiovascular risk.
What are the risks associated with abnormal P-wave measurements?
A P-wave width of 120 ms or longer correlates with a 1.6-fold increase in the risk of developing atrial fibrillation, while a width of 140 ms or more is associated with a 4.23-fold increase in heart-related events.
What does the QRS complex represent in an ECG?
The QRS complex represents ventricular depolarization and is characterized by a sharp, tall deflection. Normal QRS duration ranges from 0.06 to 0.10 seconds, with deviations indicating potential cardiac conditions.
Why is accurate measurement of QRS duration important?
Accurate measurement of QRS duration is essential for diagnostics, as abnormal durations (greater than 0.12 seconds) can indicate serious cardiac conditions and are associated with increased mortality risk.
How does MaxYield™ enhance the measurement of QRS duration?
MaxYield™ uses advanced noise filtering and wave recognition to isolate ECG waves, ensuring accurate measurement of QRS duration and morphology, even in recordings with significant noise.
What is the role of machine learning in improving ECG analysis with MaxYield™?
The platform employs machine learning models that improve over time, maximizing diagnostic yield and accuracy by utilizing engineered features related to QRS polarity direction and other critical measurements.
How can developers ensure their ECG systems provide accurate analysis?
Developers should incorporate robust algorithms capable of analyzing P-wave and QRS characteristics accurately, focusing on noise filtering and distinct wave recognition to achieve ECG normal results.






