Overview
The article provides an overview of the key features and diagnostic insights associated with inferior myocardial infarction (MI) as reflected in electrocardiogram (ECG) readings. It highlights the importance of recognizing specific ECG characteristics, particularly ST-segment elevation in leads II, III, and aVF.
The incorporation of advanced technologies, such as AI-driven platforms, is emphasized as essential for accurate diagnosis and timely intervention. This approach ultimately enhances patient outcomes in cardiac care, demonstrating the critical role of precise ECG analysis in medical practice.
Introduction
Understanding the intricacies of an electrocardiogram (ECG) is crucial for healthcare professionals, particularly in diagnosing various types of myocardial infarctions (MIs). Among these, the inferior myocardial infarction exhibits distinct ECG features that can significantly influence patient management and outcomes. Recognizing these key indicators is essential; however, healthcare professionals must also navigate the complexities of potential misinterpretations that could lead to critical delays in treatment.
The essential characteristics that differentiate an inferior MI on an ECG include specific changes in the ST segment and T waves, which can provide vital information for timely intervention. Advanced technologies can enhance diagnostic accuracy in this vital area of cardiac care, ensuring that healthcare providers are equipped with the tools necessary for effective analysis. By leveraging these technologies, professionals can improve their understanding of ECG readings, ultimately benefiting patient care and outcomes.
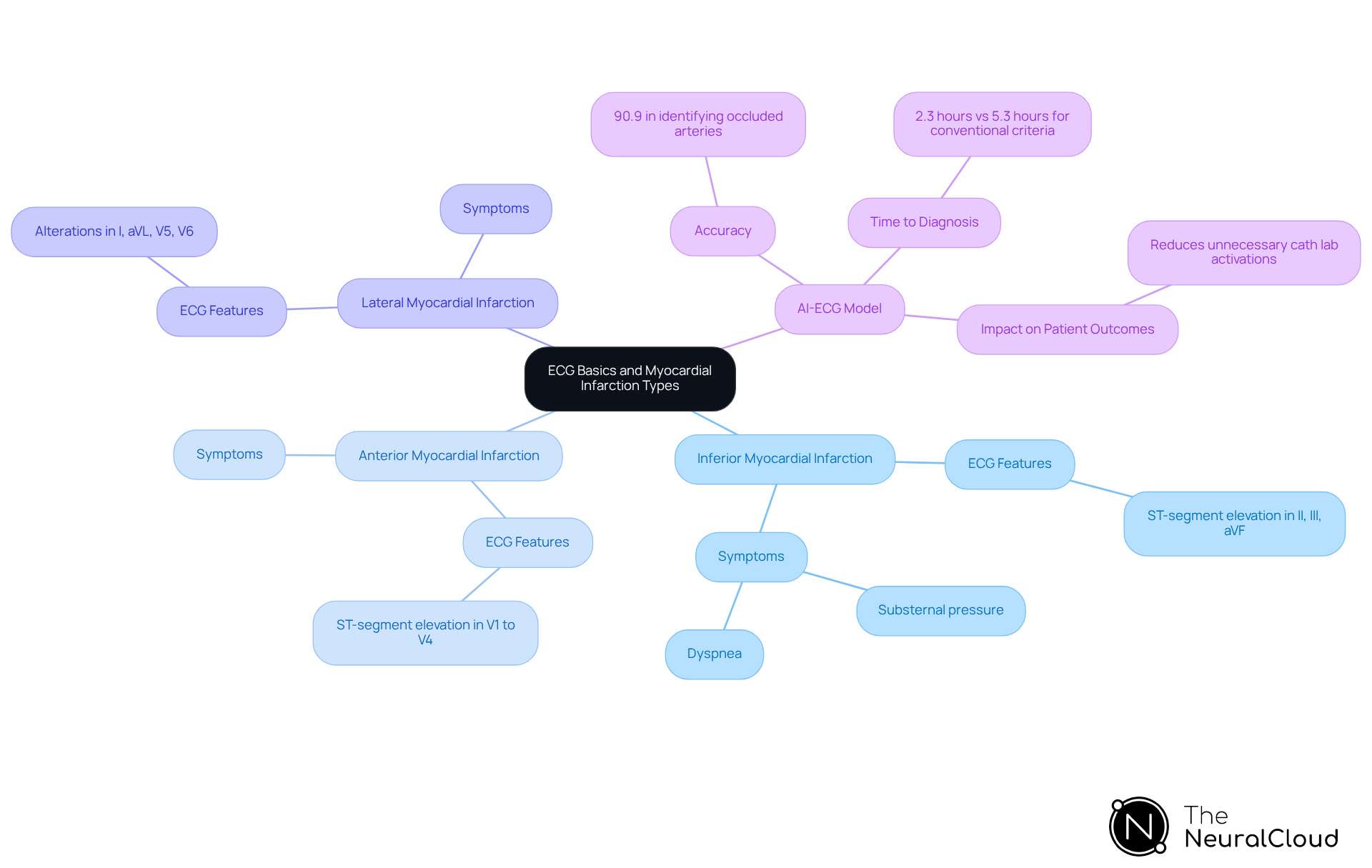
Clarify ECG Basics and Myocardial Infarction Types
An electrocardiogram (ECG) is an essential tool for diagnosing various cardiac conditions, particularly myocardial infarctions (MIs). Its significance in clinical settings is paramount, as it provides immediate insights into the heart's electrical activity, facilitating timely interventions. The integration of Neural Cloud Solutions' MaxYield™ enhances ECG analysis efficiency through advanced noise filtering and automation, enabling rapid data processing and clearer insights into cardiac events.
There are several types of MIs, each characterized by distinct ECG features:
- Inferior Myocardial Infarction: Typically results from blockage of the right coronary artery, leading to ST-segment elevation in channels II, III, and aVF. Symptoms often include substernal pressure and dyspnea.
- Anterior Myocardial Infarction: Frequently caused by blockage of the left anterior descending artery, it manifests with ST-segment elevation in positions V1 to V4, indicating damage to the anterior wall of the heart.
- Lateral Myocardial Infarction: Linked to blockage of the circumflex artery, this type shows alterations in channels I, aVL, V5, and V6, suggesting issues in the lateral wall.
Understanding these is vital for clinicians to identify the affected areas of the heart and tailor treatment strategies accordingly. The ECG's ability to reveal these changes is crucial for timely intervention, as studies indicate that early diagnosis can significantly reduce morbidity and mortality rates associated with MIs. For instance, the AI-ECG model has demonstrated an accuracy of 90.9% in identifying occluded coronary arteries, with a mean time to diagnosis of 2.3 hours, compared to 5.3 hours for conventional STEMI criteria. This underscores the potential for sophisticated ECG interpretation technologies to enhance clinical outcomes by providing beat-by-beat evaluations, identifying essential characteristics in each heartbeat, and delivering comprehensive outputs on P-wave, QRS complex, and T-wave onsets, offsets, and time-series intervals.
Recent research highlights the importance of ECG in diagnosing MIs, particularly in patients presenting with atypical symptoms or new-onset left bundle branch block (LBBB), which can complicate diagnosis by mimicking STEMI changes. Accurate interpretation of ECG changes is essential, as misinterpretation can lead to missed diagnoses and delayed treatment. As cardiology evolves, the integration of AI and advanced algorithms into ECG analysis, exemplified by Neural Cloud Solutions' MaxYield™, promises to further improve diagnostic accuracy and efficiency, potentially reducing unnecessary cath lab activations and enhancing patient outcomes. Ultimately, these advancements will significantly benefit patient care.
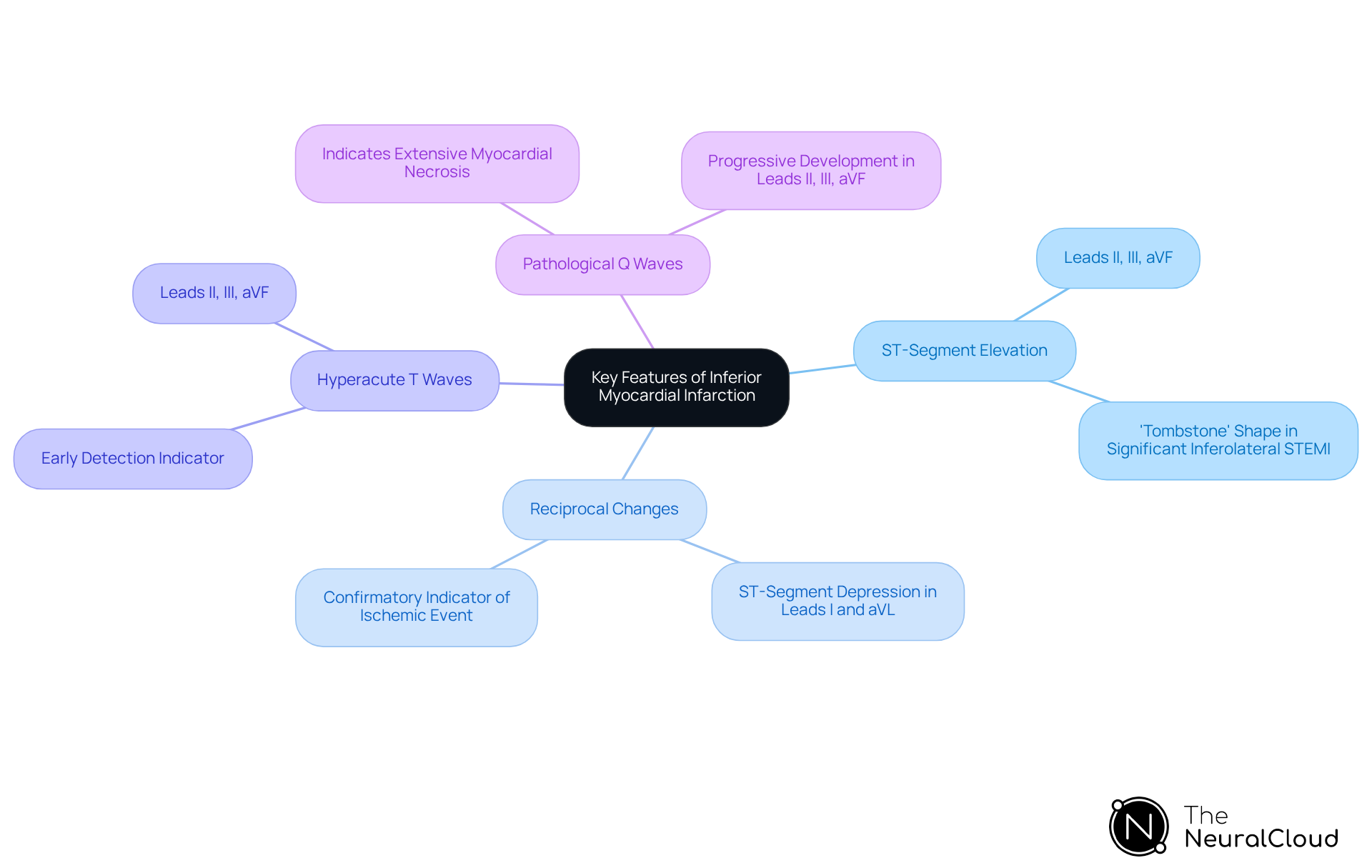
Identify Key Features of Inferior Myocardial Infarction
Key features of the ECG inferior infarct are crucial for accurate diagnosis and timely intervention. These features include:
- ST-Segment Elevation is primarily observed in leads II, III, and aVF, indicating an ECG inferior infarct that affects the inferior wall of the heart. In cases of significant inferolateral STEMI, pronounced ST elevation may present a 'tombstone' shape, suggesting extensive infarction.
- Reciprocal changes, including ST-segment depression observed in leads I and aVL, are often a confirmatory indicator of an ECG inferior infarct. The presence of these reciprocal changes is vital, as they can illuminate the extent of the ischemic event.
- Hyperacute T Waves: These may appear before ST-segment elevation and are essential for early detection of myocardial infarction. Hyperacute T waves in leads II, III, and aVF represent some of the earliest ischemic alterations, signaling the onset of an ECG inferior infarct.
- Pathological Q Waves: The appearance of Q waves in the inferior leads suggests an ECG inferior infarct, indicating a more extensive myocardial necrosis. The progressive development of Q waves in leads II, III, and aVF serves as a significant marker of myocardial damage.
Recognizing these features empowers healthcare professionals to make informed decisions regarding patient management and intervention. This is particularly critical in the context of , which is essential for optimizing outcomes in STEMI patients.
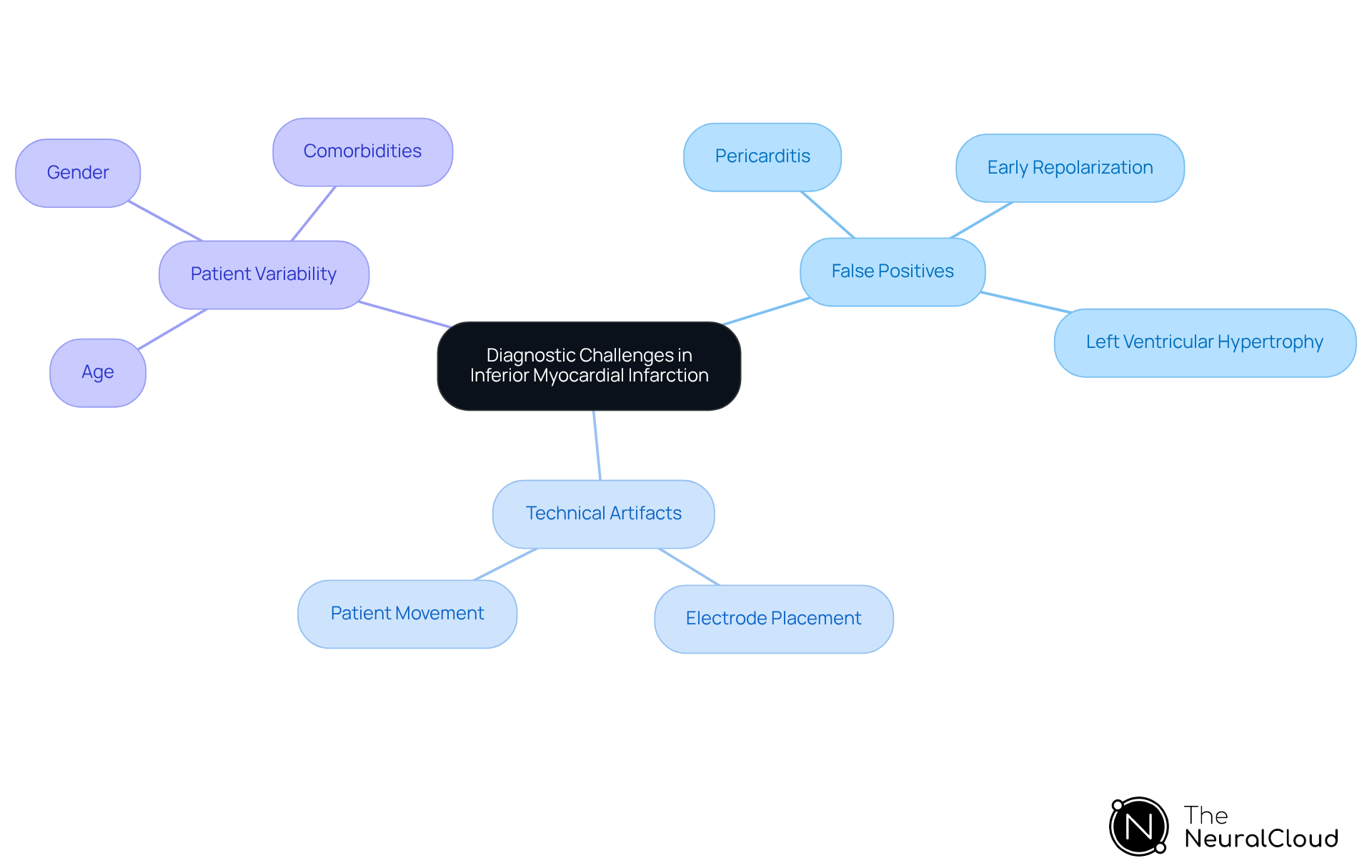
Recognize Diagnostic Challenges and False Positives
Diagnostic challenges in identifying inferior myocardial infarction include:
- False Positives: Conditions such as pericarditis, early repolarization, and left ventricular hypertrophy can mimic ST-segment elevation, leading to misdiagnosis. Studies indicate that false activations due to misinterpretation of ECGs can reach rates as high as 34%, underscoring the critical need for accurate assessment.
- Technical Artifacts: Poor electrode placement or patient movement can introduce noise, obscuring true ECG signals. This technical variability can significantly impact the interpretation of ST-segment changes, complicating the diagnostic process.
- Patient Variability: Factors such as age, gender, and comorbidities can influence ECG readings, further complicating interpretation. For instance, the presence of left bundle branch block (LBBB) can lead to discordant ST-segment changes, making it challenging to distinguish between true myocardial infarction and an ECG inferior infarct.
To reduce these challenges, clinicians should consider the clinical context and patient history while employing such as Neural Cloud Solutions' platform. This innovative tool enhances ECG clarity and automates the evaluation process, significantly reducing the likelihood of misinterpretation and improving diagnostic accuracy.
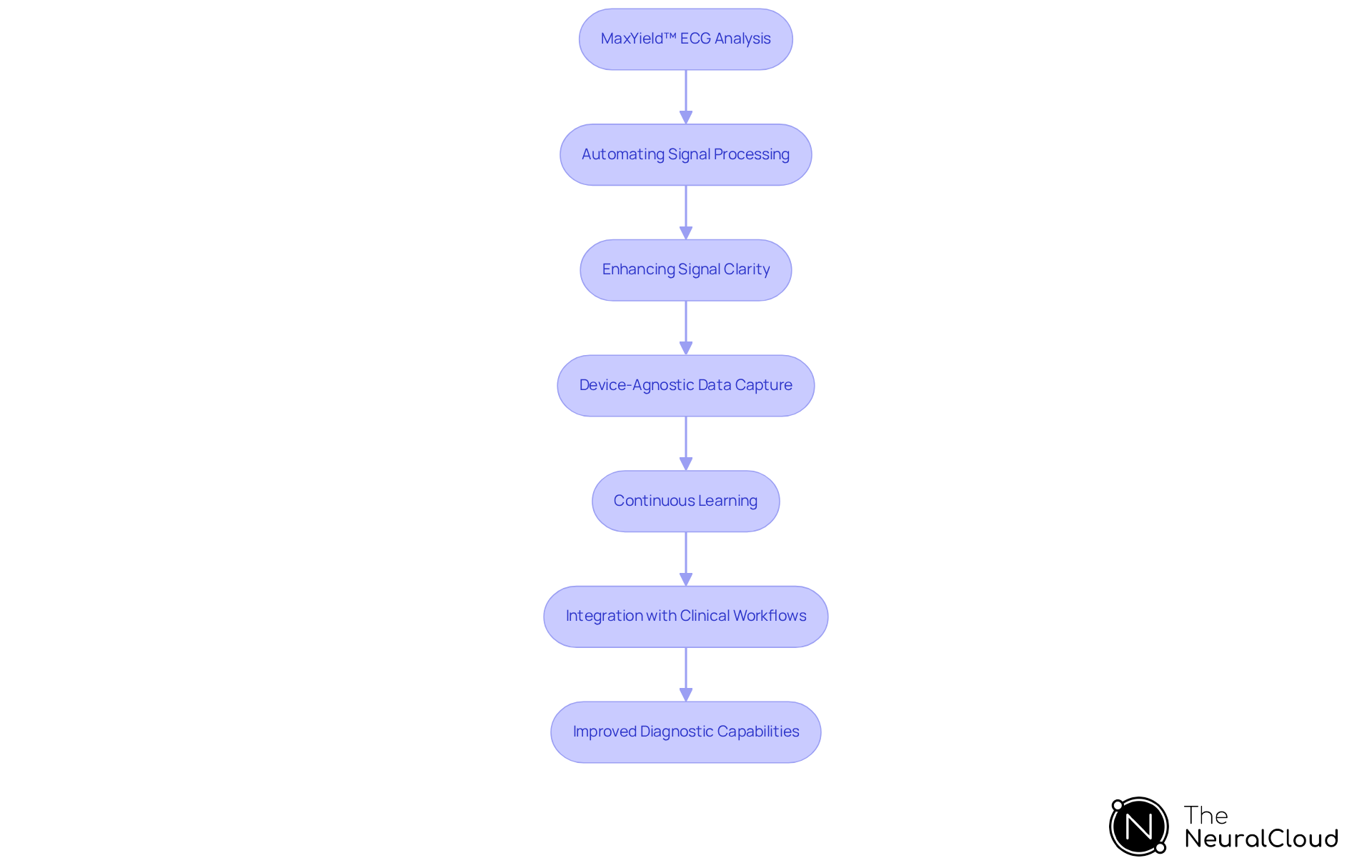
Utilize Advanced Technologies for Enhanced ECG Analysis
Advanced technologies, particularly AI-driven ECG analysis platforms like MaxYield™, significantly enhance the diagnostic process by addressing common challenges in ECG analysis. The platform offers several key features that improve the accuracy and efficiency of cardiac evaluations, ultimately benefiting healthcare professionals and their patients.
- Automating Signal Processing: This system can analyze over 200,000 heartbeats in less than five minutes, delivering rapid and precise insights that streamline clinical workflows. This beat-by-beat analysis includes detailed outputs such as P-wave, QRS complex, and T-wave onsets, offsets, and time-series intervals, allowing for efficient data management and supporting confident clinical decision-making.
- Enhancing Signal Clarity: Advanced algorithms in the system effectively filter out noise and artifacts, ensuring that genuine cardiac signals are accurately represented. This capability is crucial for reliable diagnosis, particularly in complex cases.
- Device-Agnostic Data Capture: The system seamlessly captures ECG recordings from any 1-lead or 3-lead device, including wearable devices and Holter monitors. This flexibility improves the incorporation of ECG evaluation into various clinical environments.
- Continuous Learning: These AI systems are designed to evolve over time, enhancing their diagnostic accuracy as they assimilate new data, thereby adapting to emerging clinical needs.
- Integration with Clinical Workflows: Advanced ECG technologies such as MaxYield™ can effortlessly merge with current healthcare systems, promoting effective data management and evaluation, which is vital for contemporary clinical settings. The evaluation results can be exported in CSV format for easy ingestion into current workflows.
By leveraging such innovative tools, healthcare professionals can significantly enhance their diagnostic capabilities, leading to improved patient outcomes and optimized resource allocation. The integration of AI in ECG analysis not only reduces interpretation variability but also supports early detection of conditions like hypertrophic cardiomyopathy and atrial fibrillation. This ultimately transforms cardiac care, as highlighted by the advancements in tools like MaxYield™ that enable rapid data processing and the discovery of new digital biomarkers.
Conclusion
Understanding the key features of ECG inferior infarcts is essential for healthcare professionals aiming to provide timely and effective cardiac care. This article emphasizes the importance of accurate ECG interpretation in diagnosing myocardial infarctions, particularly inferior MIs, which are indicated by specific changes in ECG patterns. With advancements in technology, such as AI-driven platforms like Neural Cloud Solutions' MaxYield™, the diagnostic process can be significantly streamlined, enhancing both speed and accuracy.
The discussion highlights the critical characteristics of inferior myocardial infarctions, including:
- ST-segment elevation
- Reciprocal changes
- Hyperacute T waves
- Pathological Q waves
Each of these features plays a vital role in identifying the extent of myocardial damage and guiding appropriate treatment strategies. Furthermore, the article addresses the diagnostic challenges, including false positives and technical artifacts, underscoring the necessity for clinicians to remain vigilant and utilize advanced tools to mitigate misinterpretation risks.
In conclusion, the integration of advanced technologies into ECG analysis not only enhances diagnostic accuracy but also promises to revolutionize cardiac care. As the field evolves, embracing AI and innovative solutions will be crucial for improving patient outcomes and optimizing clinical workflows. Healthcare professionals are encouraged to leverage these advancements to ensure swift and accurate diagnoses of inferior myocardial infarctions, ultimately leading to better patient management and care.
Frequently Asked Questions
What is an electrocardiogram (ECG) and its significance in diagnosing cardiac conditions?
An electrocardiogram (ECG) is a vital tool for diagnosing various cardiac conditions, especially myocardial infarctions (MIs). It provides immediate insights into the heart's electrical activity, which is crucial for timely interventions in clinical settings.
How does Neural Cloud Solutions' MaxYield™ enhance ECG analysis?
Neural Cloud Solutions' MaxYield™ improves ECG analysis efficiency through advanced noise filtering and automation, allowing for rapid data processing and clearer insights into cardiac events.
What are the different types of myocardial infarctions (MIs) and their ECG features?
- Inferior Myocardial Infarction: Caused by blockage of the right coronary artery, characterized by ST-segment elevation in channels II, III, and aVF.
- Anterior Myocardial Infarction: Often due to blockage of the left anterior descending artery, indicated by ST-segment elevation in positions V1 to V4.
- Lateral Myocardial Infarction: Associated with blockage of the circumflex artery, showing alterations in channels I, aVL, V5, and V6.
Why is understanding the types of MIs important for clinicians?
Understanding the classifications of MIs helps clinicians identify the affected areas of the heart and tailor treatment strategies accordingly, which is vital for effective patient care.
How does early diagnosis of MIs impact patient outcomes?
Early diagnosis of MIs can significantly reduce morbidity and mortality rates. Studies show that advanced ECG interpretation technologies can enhance clinical outcomes by providing timely and accurate evaluations.
What is the accuracy of the AI-ECG model in diagnosing occluded coronary arteries?
The AI-ECG model has demonstrated an accuracy of 90.9% in identifying occluded coronary arteries, with a mean time to diagnosis of 2.3 hours, compared to 5.3 hours for conventional STEMI criteria.
How does the interpretation of ECG changes affect the diagnosis of MIs?
Accurate interpretation of ECG changes is crucial, especially in patients with atypical symptoms or new-onset left bundle branch block (LBBB), as misinterpretation can lead to missed diagnoses and delayed treatment.
What advancements are being made in ECG analysis to improve diagnostic accuracy?
The integration of AI and advanced algorithms, such as those exemplified by Neural Cloud Solutions' MaxYield™, promises to improve diagnostic accuracy and efficiency, potentially reducing unnecessary cath lab activations and enhancing patient outcomes.






