Overview
The article provides an informative overview on identifying anterior infarcts on an ECG, highlighting key indicators such as:
- ST segment elevation
- Q deflections
- T wave changes
It articulates the challenges faced in ECG analysis and presents a systematic step-by-step approach to enhance understanding. By emphasizing the importance of recognizing these indicators, the article supports accurate diagnosis and improved patient outcomes. This structured approach not only clarifies the process but also underscores the significance of these features in clinical practice.
Introduction
Understanding the intricacies of an electrocardiogram (ECG) is essential for healthcare professionals, especially when diagnosing conditions such as anterior myocardial infarction. Mastering the key indicators and patterns associated with this type of heart attack enables practitioners to enhance their diagnostic accuracy significantly and improve patient outcomes. However, navigating the complexities of ECG readings presents a challenge, as misinterpretation can lead to serious clinical consequences.
How can one effectively identify an anterior infarct on an ECG and avoid common pitfalls in interpretation?
Understand ECG Basics and Anterior Infarct Indicators
To effectively recognize a frontal infarct on an ECG, one must first understand the basic components of an ECG tracing. An ECG assesses the electrical activity of the heart through various connections, with each connection offering a different viewpoint on heart function. Key indicators of anterior infarction include:
- ST Segment Elevation: Look for ST segment elevation in leads V1 to V6, particularly V3 and V4, which are critical for diagnosing anterior myocardial infarction (MI). Research shows that an ST elevation of ≥0.2 mV in several anterior recordings has a sensitivity of 56% and a specificity of 94% for acute MI.
- Q Deflections: The presence of pathological Q deflections in these leads can indicate previous myocardial damage. Pathological Q deflections are defined as being greater than 40 ms wide, greater than 2 mm deep, or more than 25% of the depth of the QRS complex.
- T Changes: Inversion of T changes may also suggest ischemia.
Acquainting yourself with these indicators will enhance your ability to identify possible infarcts in clinical practice. Moreover, testimonials from cardiologists highlight the significance of correctly interpreting Q waves, stating that miscommunication about ECG results can lead to considerable clinical implications. Understanding these indicators is essential for healthcare professionals, as they possible anterior infarct on ECG in clinical practice.

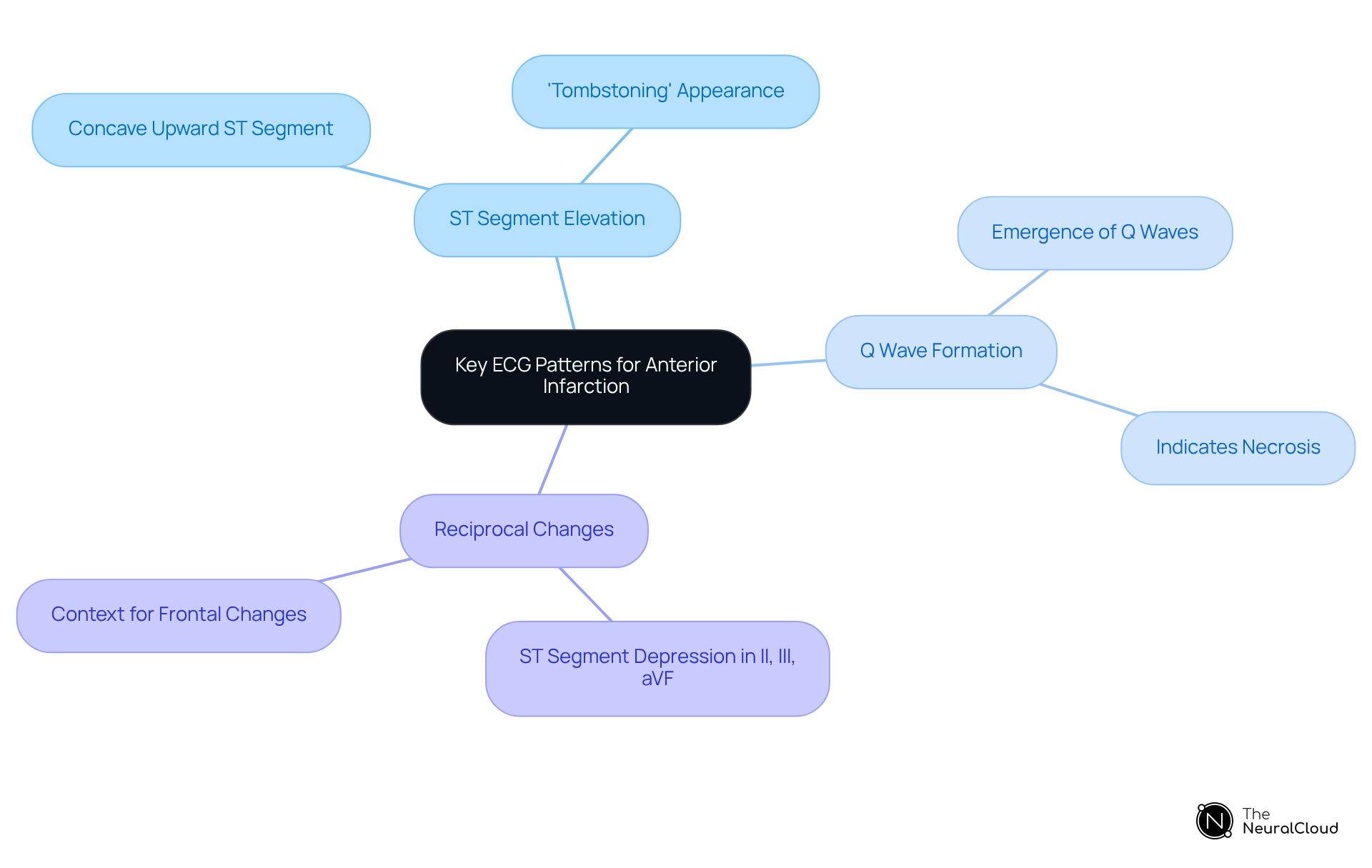
Recognize Key ECG Patterns for Anterior Infarction
Key ECG patterns to recognize for anterior infarction include:
- ST Segment Elevation: Look for a concave upward ST segment elevation in leads V3 and V4, often described as 'tombstoning.' This pattern is a hallmark of , often identified as an anterior infarct on ECG.
- Q Wave Formation: The emergence of Q waves in positions V1 to V6 suggests necrosis and serves as a vital indicator of an old or progressing heart attack.
- Reciprocal Changes: Observe for ST segment depression in inferior recordings (II, III, aVF), as these can provide further context for the frontal changes.
By familiarizing yourself with these patterns, you can enhance your diagnostic accuracy and improve patient outcomes.
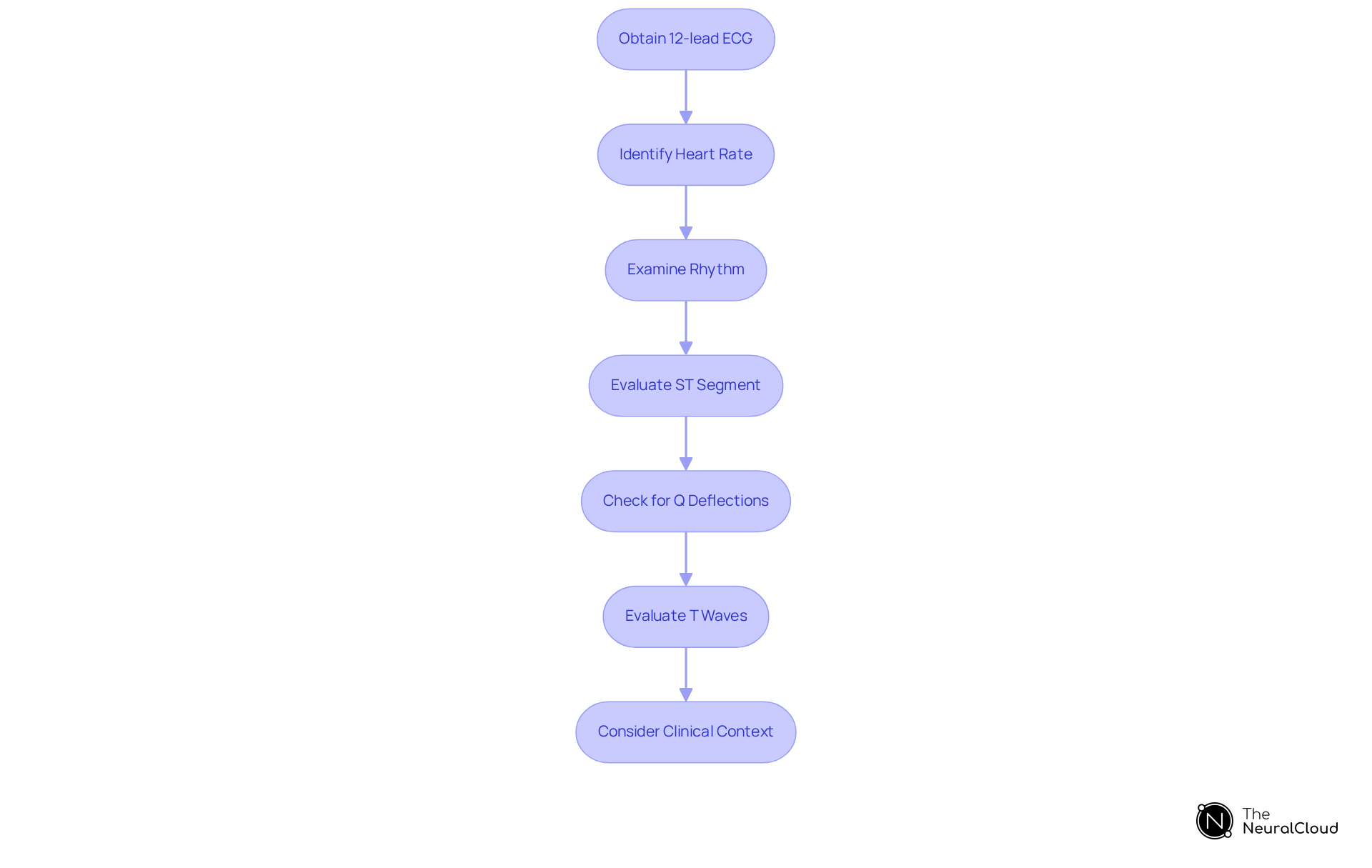
Analyze ECG Readings: Step-by-Step Identification Process
To analyze ECG readings for anterior infarction, follow these steps:
- Obtain a 12-lead electrocardiogram: Ensure proper electrode placement to avoid misinterpretation due to artifacts.
- Identify the heart rate: Calculate the heart rate to assess for bradycardia or tachycardia, which can influence interpretation.
- Examine the rhythm: Determine if the rhythm is regular or irregular, as this can provide context for the ST segment changes.
- Evaluate the ST segment: Check for elevation in positions V3 and V4, observing the degree and shape of the elevation.
- Check for Q deflections: Identify any Q deflections in the precordial leads, which indicate myocardial necrosis.
- Evaluate T waves: Look for T wave inversions that may accompany ST segment changes.
- Consider clinical context: Always correlate ECG findings with the patient's clinical presentation and history.
By following this structured approach, you can systematically identify an anterior infarct on ECG and make informed clinical decisions.
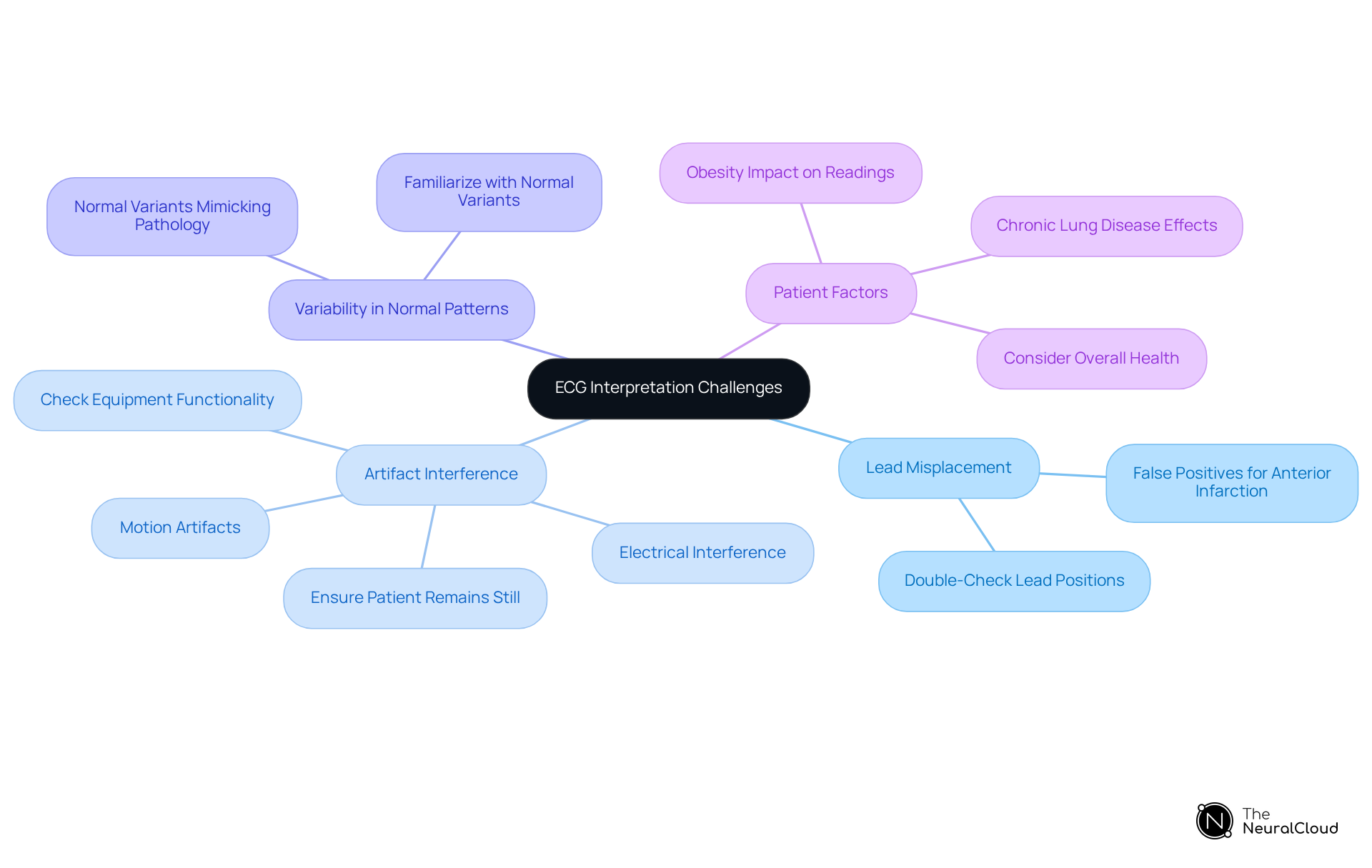
Troubleshoot Common ECG Interpretation Challenges
Common challenges in ECG interpretation include:
- Lead Misplacement: Incorrect lead placement can lead to false positives for anterior infarction. Always double-check lead positions to ensure accuracy.
- Artifact Interference: Motion artifacts or electrical interference can obscure true ECG signals. Ensure the patient remains still and that the equipment is functioning properly to mitigate these issues.
- Variability in Normal Patterns: Normal variations in ECG can mimic pathological changes. Familiarize yourself with normal variants to avoid misinterpretation and enhance diagnostic accuracy.
- Patient Factors: Conditions such as obesity or chronic lung disease can alter ECG readings. Always consider the patient's overall health when interpreting results to provide a comprehensive analysis.
By being aware of these challenges and employing troubleshooting strategies, you can enhance your ECG interpretation skills and improve diagnostic accuracy.
Conclusion
Mastering the identification of anterior infarcts on an ECG is essential for healthcare professionals seeking to enhance their diagnostic capabilities. A solid understanding of the fundamental components of ECG readings—such as ST segment elevation, Q deflections, and T wave changes—establishes a foundation for accurately recognizing anterior myocardial infarction. By familiarizing themselves with these indicators and the specific ECG patterns associated with anterior infarction, clinicians can significantly improve their ability to make informed decisions in emergency situations.
This article outlines essential steps for analyzing ECG readings, emphasizing a systematic approach that includes:
- Obtaining a 12-lead ECG
- Evaluating heart rate and rhythm
- Closely examining ST segments and Q deflections
It also addresses common challenges in ECG interpretation, such as lead misplacement and artifact interference, while providing valuable troubleshooting strategies to enhance accuracy. Each of these elements contributes to a comprehensive understanding of how to effectively identify anterior infarcts and mitigate the risks associated with misinterpretation.
Ultimately, the ability to accurately interpret ECGs for anterior myocardial infarction not only aids in timely diagnosis but also plays a pivotal role in improving patient outcomes. As the landscape of cardiac care continues to evolve, mastering these skills empowers healthcare professionals to respond adeptly to critical situations. Embracing ongoing education and practice in ECG interpretation is essential for anyone involved in patient care, ensuring they remain at the forefront of effective cardiac diagnostics.
Frequently Asked Questions
What is the purpose of an ECG?
An ECG assesses the electrical activity of the heart through various connections, providing different viewpoints on heart function.
What are the key indicators of an anterior myocardial infarction (MI) on an ECG?
Key indicators include ST segment elevation, pathological Q deflections, and T changes.
How can ST segment elevation indicate an anterior infarct?
ST segment elevation in leads V1 to V6, especially V3 and V4, is critical for diagnosing anterior MI. An elevation of ≥0.2 mV in several anterior recordings has a sensitivity of 56% and a specificity of 94% for acute MI.
What defines pathological Q deflections?
Pathological Q deflections are defined as being greater than 40 ms wide, greater than 2 mm deep, or more than 25% of the depth of the QRS complex.
What does T wave inversion suggest in an ECG?
Inversion of T waves may suggest ischemia.
Why is it important for healthcare professionals to understand ECG indicators?
Understanding these indicators enhances the ability to identify possible anterior infarcts, which is crucial for effective clinical practice and can prevent miscommunication regarding ECG results that may have significant clinical implications.






