Overview
The article addresses the challenges faced in accurately analyzing and mitigating ECG artifacts, which can significantly impact cardiac readings. It identifies various types of artifacts, including loose lead and wandering baseline disturbances. The article underscores the importance of proper skin preparation, quality electrodes, and advanced technologies such as the MaxYield™ platform. This platform enhances ECG accuracy, ultimately improving patient outcomes.
The MaxYield™ platform offers several key features that address these challenges:
- It provides advanced algorithms designed to detect and filter out common ECG artifacts effectively.
- Its integration with high-quality electrodes ensures optimal signal acquisition.
- The platform's user-friendly interface allows healthcare professionals to interpret data quickly and accurately.
These features translate into significant advantages for healthcare professionals. By utilizing the MaxYield™ platform, practitioners can achieve more reliable cardiac readings, leading to better-informed clinical decisions. Furthermore, the reduction of artifacts enhances the overall efficiency of ECG analysis, allowing for quicker patient assessments and improved care.
In conclusion, the MaxYield™ platform not only addresses the technical challenges of ECG analysis but also offers tangible benefits for healthcare providers. By improving the accuracy of cardiac readings, it ultimately contributes to enhanced patient outcomes, making it an essential tool in modern cardiology.
Introduction
Understanding the intricacies of ECG artifacts is essential for healthcare professionals aiming for accurate cardiac readings. These disturbances, arising from both physiological and external sources, can significantly undermine the accuracy of ECG interpretations, potentially leading to misdiagnoses. This article explores effective strategies for identifying, analyzing, and mitigating these artifacts, providing clinicians with the necessary tools to enhance diagnostic accuracy.
How can healthcare providers ensure they are not misled by erroneous signals? Additionally, what innovative solutions exist to address this widespread challenge?
Understand ECG Artifacts: Types and Causes
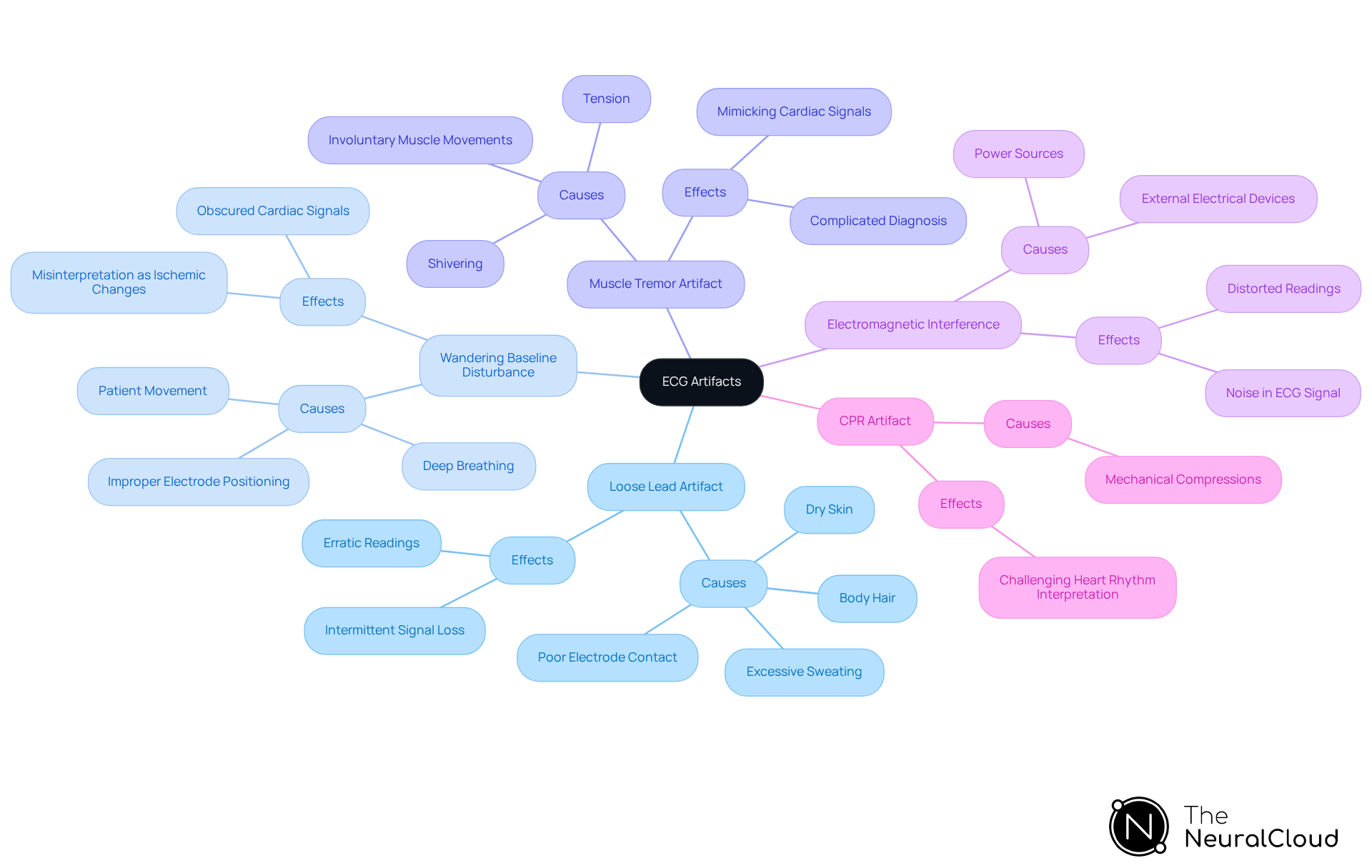
ECG disturbances, often referred to as [ECG artefacts](https://theneuralcloud.com/post/understanding-artefact-on-ecg-types-impact-and-reduction-strategies), can arise from various physiological and non-physiological sources, significantly impacting the accuracy of cardiac readings. Understanding these is crucial for clinicians to ensure precise ECG interpretation and to minimize potential misdiagnoses caused by misleading signals. Common types of ECG artifacts include:
- Loose Lead Artifact: This occurs when electrodes are not securely attached to the skin, leading to erratic readings. Poor electrode contact may result from dry skin, excessive sweating, or body hair, causing intermittent signal loss or irregular waveforms. Statistics indicate that a substantial proportion of ECG recordings are not analyzable due to such interferences, highlighting the importance of proper electrode positioning and skin preparation to reduce ECG artefacts.
- Wandering Baseline Disturbance: Often triggered by individual movement or improper electrode positioning, this disturbance leads to ECG artefacts that can obscure genuine cardiac signals. Deep or irregular breathing can also contribute to baseline wandering, which may be misinterpreted as ischemic ST-segment changes. Case studies have shown that wandering baseline disturbances, which are considered ECG artefacts, can impede ECG analysis, necessitating careful observation of patient activity during recordings.
- Muscle Tremor Artifact: Caused by involuntary muscle movements like shivering or tension, these can mimic cardiac signals and complicate diagnosis, contributing to the presence of ECG artefacts. Encouraging patients to relax and hold their breath briefly during recordings is essential to reduce this type of interference.
- Electromagnetic Interference (EMI): External electrical devices can introduce noise into the ECG signal, distorting readings. To mitigate such interference that may cause ECG artefacts, ECG machines should be plugged into dedicated, grounded outlets and positioned away from power sources and electronic equipment.
- CPR Artifact: During cardiopulmonary resuscitation, mechanical compressions can create distinct patterns on the ECG, making accurate interpretation of heart rhythms challenging. Training healthcare professionals to recognize ECG artefacts and other distortions is critical for effective cardiac monitoring.
The 'Neural Cloud Solutions' platform addresses these challenges by employing advanced noise filtering and wave recognition techniques. By swiftly isolating ECG waves from recordings affected by baseline drift, movement, and muscle interferences, the system enhances the precision of ECG analysis. Its algorithm evolves with each use, continuously improving accuracy and efficiency, enabling healthcare providers to recover previously obscured segments of lengthy Holter, 1-Lead, and patch monitor recordings. By identifying and addressing these common ECG artefacts, healthcare providers can significantly improve their ability to accurately assess cardiac conditions, ultimately enhancing patient outcomes.
Identify ECG Artifacts: Techniques and Best Practices
To effectively identify ECG artifacts, clinicians can utilize several techniques, enhanced by the capabilities of Neural Cloud Solutions' MaxYield™ platform:
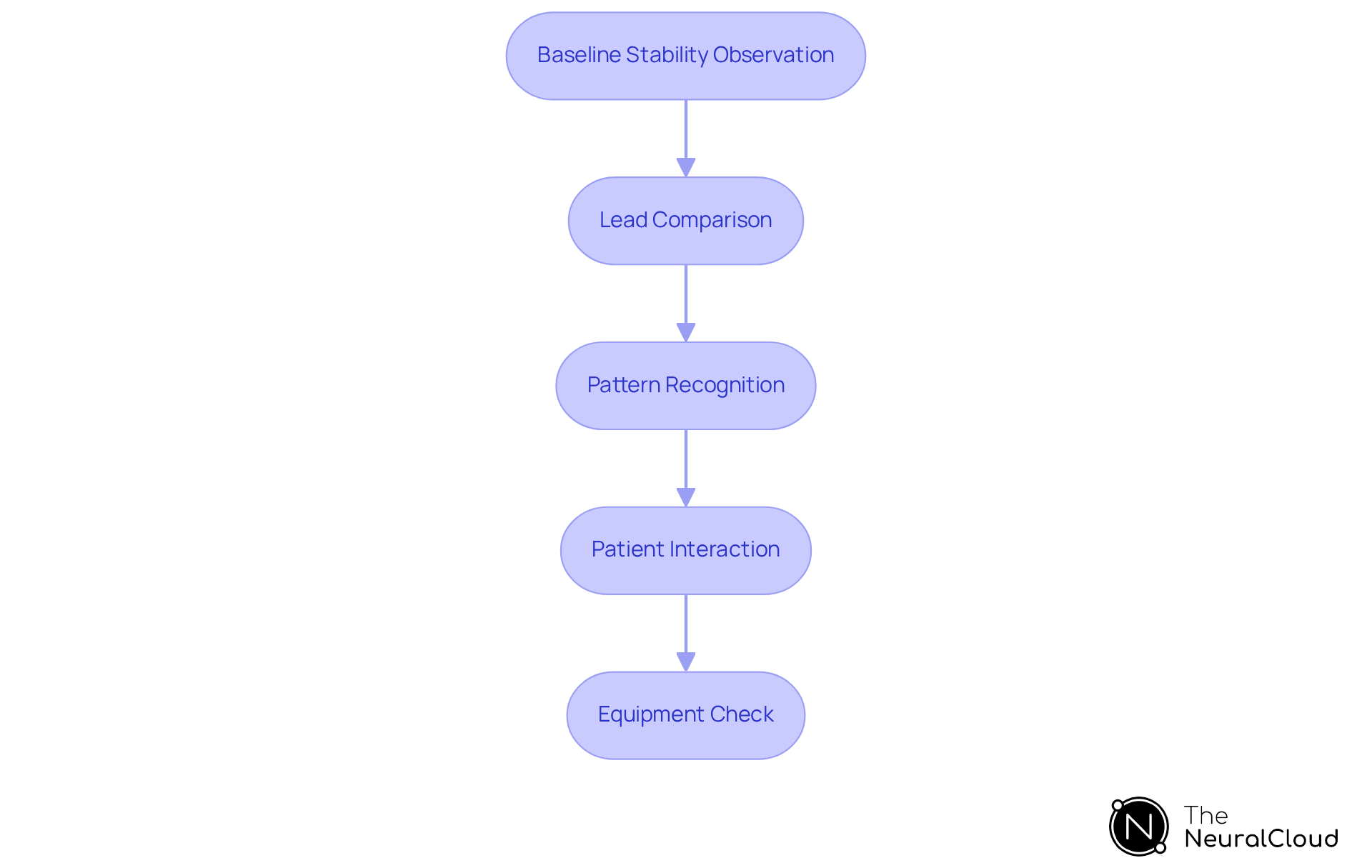
- Baseline Stability Observation: Clinicians should monitor the baseline for stability; fluctuations may indicate artifacts. MaxYield™ excels in isolating ECG waves while managing ECG artefacts, even amidst baseline wander, ensuring clearer readings.
- Lead Comparison: Comparing readings across different leads can help identify inconsistencies that may indicate ECG artefacts. The platform's advanced algorithms adapt to physiological variability, improving accuracy across diverse patient profiles.
- Pattern Recognition: Familiarizing oneself with common patterns, such as sharp spikes or irregular rhythms, aids in quickly identifying anomalies and distinguishing them from ECG artefacts. The system continuously evolves its recognition capabilities, enhancing diagnostic yield over time.
- Patient Interaction: Engaging with the patient minimizes movement and ensures comfort, which can help reduce issues related to motion. The combination of wearable technology allows for automated labeling, further simplifying this process.
- Equipment Check: Regularly inspecting and maintaining ECG equipment prevents technical issues that could introduce ECG artefacts. This system aids in salvaging previously obscured sections of recordings, ensuring that even with equipment challenges, critical data is not lost.
Implementing these techniques, alongside the advanced features of MaxYield™, can significantly improve the accuracy of ECG readings and minimize ECG artefacts, enhancing the clinician's ability to make informed decisions.
Mitigate ECG Artifacts: Effective Reduction Strategies
To effectively mitigate ECG artifacts, implement the following strategies:
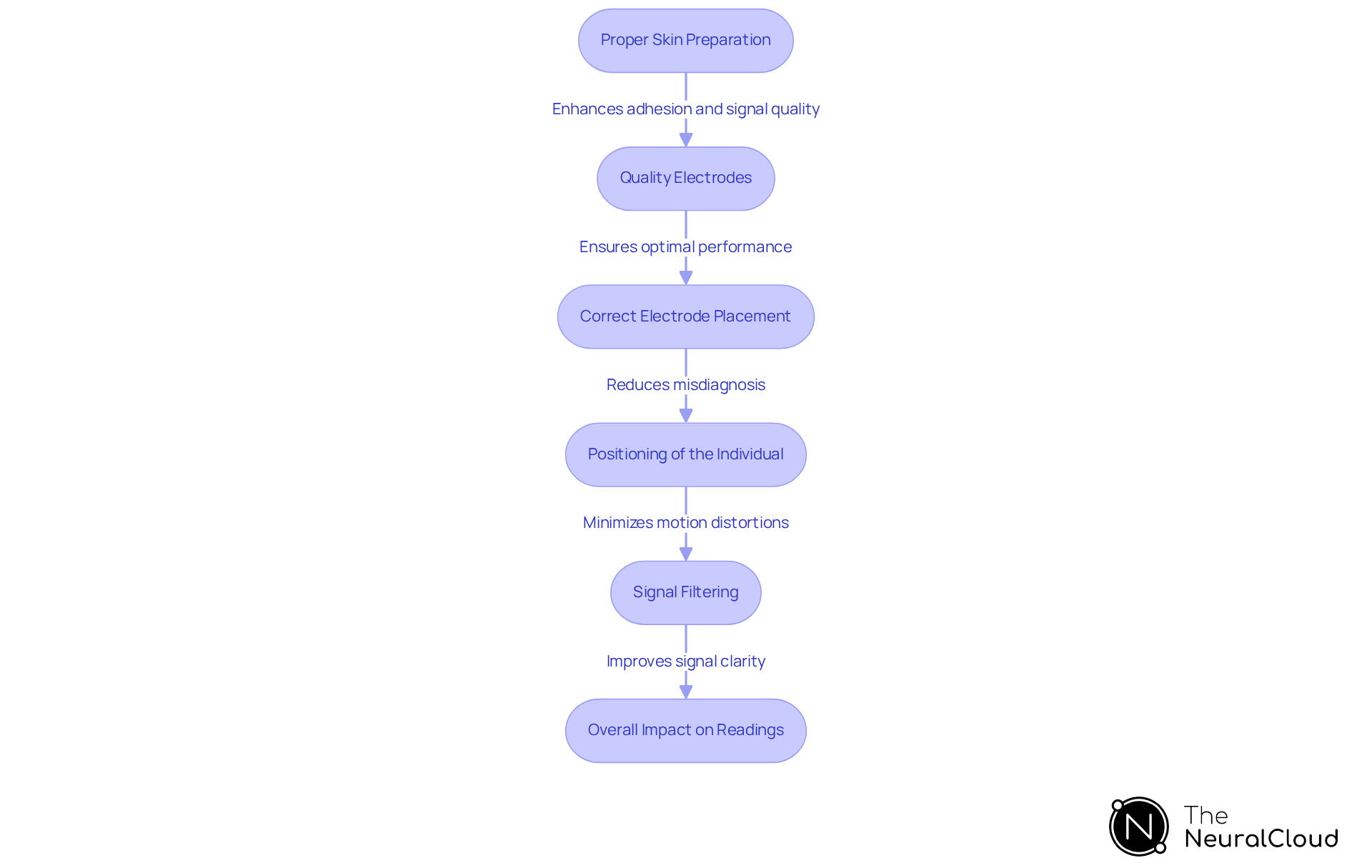
- Proper Skin Preparation: Thoroughly cleanse and dry the skin prior to electrode placement to enhance adhesion and signal quality. Research indicates that proper skin preparation can reduce ECG artefacts by up to 70%, which significantly improves the accuracy of readings. The system further supports this by ensuring that the signal quality is optimized through its advanced noise filtering capabilities.
- Quality Electrodes: Utilize high-quality electrodes tailored to the patient's skin type and condition. Studies have shown that the application of conductive gel can enhance the performance of textile electrodes, making them a viable alternative to traditional Ag/AgCl electrodes. MaxYield™ can help in identifying the best electrode types for specific conditions, ensuring optimal performance.
- Correct Electrode Placement: Follow established guidelines for electrode positioning to reduce frequent mistakes that can result in distortions. Inaccurate lead placement is a frequent cause of misdiagnosis, with automated systems experiencing a 45% misdiagnosis rate due to ECG artefacts. MaxYield™ enhances this process by providing real-time feedback on electrode placement, reducing the likelihood of errors.
- Positioning of the Individual: Ensure the individual is comfortably situated and minimize movement during the ECG recording. Patient movements, such as coughing or shifting, can introduce motion distortions that complicate interpretation. The platform can monitor patient movement and notify the technician of potential issues during the recording.
- Signal Filtering: Employ advanced filtering techniques, including low-pass and high-pass filters, to eliminate unwanted noise while maintaining the integrity of the ECG signal. The 'Neural Cloud Solutions' platform enhances this process by employing sophisticated noise filtering and wave identification, enabling the separation of ECG waves even in recordings with elevated levels of noise and interference. Setting the diagnostic mode of a 12-lead ECG monitor to 0.05 - 40 Hz can help minimize 60 cycle interference, further enhancing signal clarity.
By adopting these strategies, healthcare professionals can significantly reduce the impact of ECG artefacts on readings, leading to more reliable data for clinical decision-making. As noted by Wendy Pearson, "[Proper skin preparation techniques are essential for ensuring high-quality ECG recordings](https://theneuralcloud.com/technician-solution), as they can significantly influence the accuracy of the results." Additionally, incorporating the system into the workflow can streamline processes, automate repetitive tasks, and enhance overall diagnostic yield.
Leverage Technology: Integrate Advanced Solutions for Accurate ECG Analysis
To enhance ECG analysis, it is essential to integrate advanced technologies that can help .
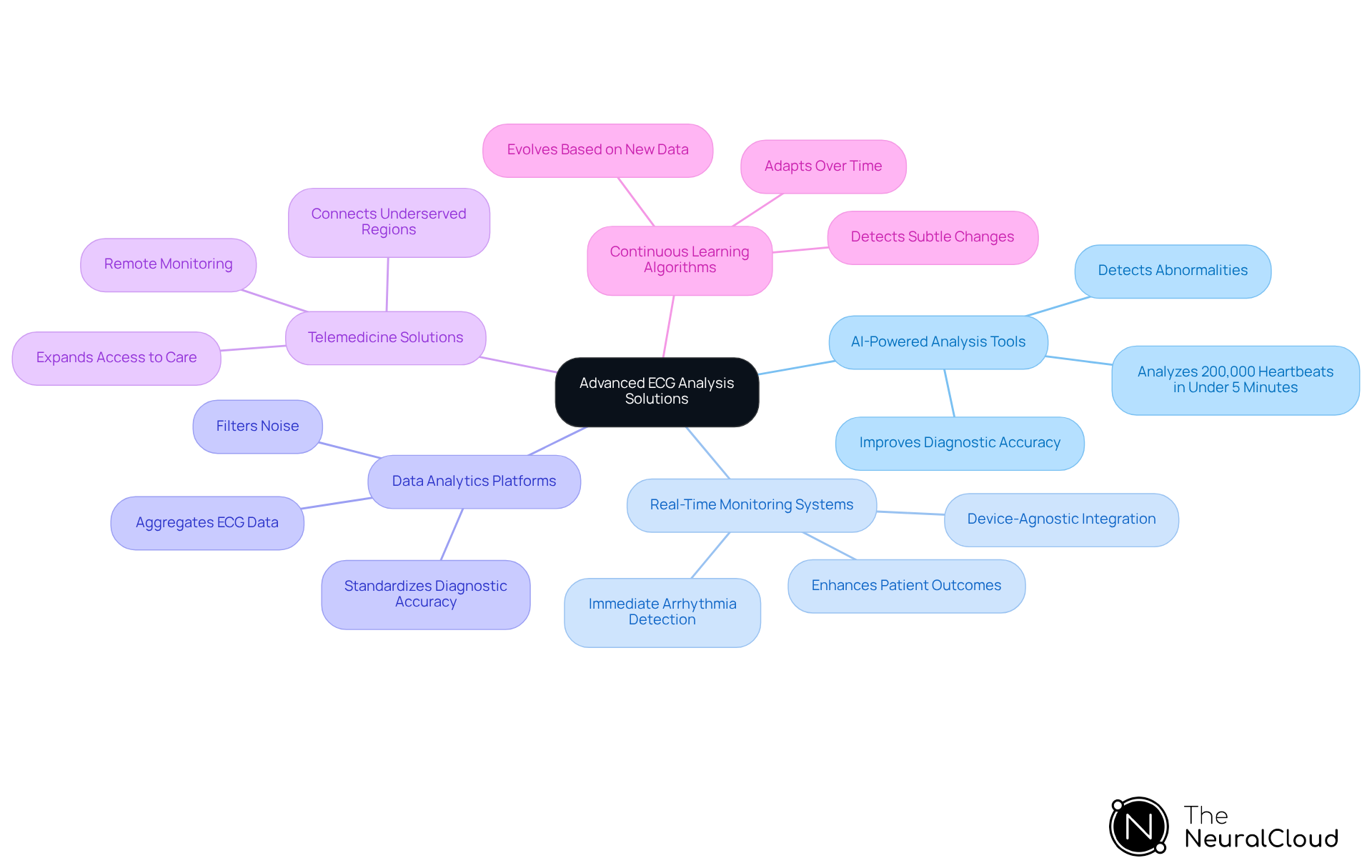
- AI-Powered Analysis Tools: The MaxYield™ platform from Neural Cloud Solutions leverages AI algorithms to automatically detect and classify ECG abnormalities. This significantly improves diagnostic accuracy and speed. The system can analyze 200,000 heartbeats in under five minutes, demonstrating high accuracy in arrhythmia detection.
- Real-Time Monitoring Systems: Continuous ECG monitoring systems facilitate immediate detection of arrhythmias and other cardiac issues. The device-agnostic features allow for smooth integration with various monitoring apparatus, which is crucial for prompt interventions that enhance outcomes for patients.
- Data Analytics Platforms: Utilizing platforms that aggregate and analyze ECG data from multiple sources provides comprehensive insights into cardiac health. This process is enhanced by filtering noise and isolating critical ECG waves to minimize ECG artefacts, ensuring standardized diagnostic accuracy across health systems.
- Telemedicine Solutions: Telemedicine technologies enable remote ECG monitoring and interpretation, thereby expanding access to care. This approach is particularly beneficial for connecting with individuals in underserved regions, ultimately improving healthcare delivery.
- Continuous Learning Algorithms: Systems that adapt and improve over time enhance the ability to detect subtle changes in ECG patterns. The continuous learning model ensures that diagnostic tools evolve based on new data, maintaining their cutting-edge status in ECG analysis.
Integrating these technologies can revolutionize ECG analysis by reducing ECG artefacts, empowering healthcare professionals to deliver more accurate and timely cardiac care. As Milind Desai, Director of the Center for Hypertrophic Cardiomyopathy at Cleveland Clinic, noted, "By utilizing AI as an additional set of eyes, we can enhance the capacity to identify more individuals with HCM sooner and among varied populations, addressing a condition that’s frequently difficult to recognize." The integration of advanced ECG technologies, particularly through Neural Cloud Solutions' MaxYield™, is pivotal in overcoming the challenges of traditional diagnostic methods, especially those related to ECG artefacts, ultimately leading to improved patient outcomes.
Conclusion
Understanding and addressing ECG artifacts is essential for accurate cardiac monitoring and diagnosis. By recognizing various types of artifacts, including loose lead artifacts, wandering baseline disturbances, and electromagnetic interference, healthcare professionals can significantly enhance ECG reading quality. The MaxYield™ platform offers advanced technologies that equip clinicians with powerful tools to effectively identify and mitigate these artifacts, ensuring clearer and more reliable data for informed decision-making.
Key strategies for mitigating ECG artifacts encompass:
- Proper skin preparation
- The use of quality electrodes
- Maintaining correct electrode placement
Engaging with patients to minimize motion and employing advanced signal filtering techniques are also crucial steps in improving ECG reading accuracy. Implementing these best practices and leveraging technology enables healthcare providers to reduce misdiagnosis risks and enhance patient outcomes.
The importance of mastering ECG artifacts cannot be overstated. As cardiac care evolves, adopting innovative solutions and methodologies is vital to overcoming traditional challenges. Embracing advanced technologies not only improves diagnostic accuracy but also expands access to quality cardiac care. Ultimately, prioritizing the reduction of ECG artifacts leads to more effective monitoring and treatment, ensuring patients receive the best possible care in their journey toward better heart health.
Frequently Asked Questions
What are ECG artifacts?
ECG artifacts are disturbances that can arise from various physiological and non-physiological sources, impacting the accuracy of cardiac readings and potentially leading to misdiagnoses.
What are common types of ECG artifacts?
Common types of ECG artifacts include Loose Lead Artifact, Wandering Baseline Disturbance, Muscle Tremor Artifact, Electromagnetic Interference (EMI), and CPR Artifact.
What causes Loose Lead Artifact?
Loose Lead Artifact occurs when electrodes are not securely attached to the skin, often due to dry skin, excessive sweating, or body hair, leading to erratic readings and intermittent signal loss.
How does Wandering Baseline Disturbance affect ECG readings?
Wandering Baseline Disturbance, caused by individual movement or improper electrode positioning, can obscure genuine cardiac signals and may be misinterpreted as ischemic ST-segment changes.
What is Muscle Tremor Artifact and how can it be reduced?
Muscle Tremor Artifact is caused by involuntary muscle movements such as shivering or tension, which can mimic cardiac signals. Encouraging patients to relax and hold their breath briefly during recordings can help reduce this interference.
What is Electromagnetic Interference (EMI) in ECG?
Electromagnetic Interference (EMI) is noise introduced into the ECG signal from external electrical devices, distorting readings. To mitigate this, ECG machines should be plugged into dedicated, grounded outlets and kept away from power sources and electronic equipment.
How does CPR Artifact impact ECG interpretation?
CPR Artifact occurs during cardiopulmonary resuscitation when mechanical compressions create distinct patterns on the ECG, making accurate interpretation of heart rhythms challenging.
What solutions does the 'Neural Cloud Solutions' platform provide for ECG artifacts?
The 'Neural Cloud Solutions' platform employs advanced noise filtering and wave recognition techniques to isolate ECG waves from recordings affected by various artifacts, enhancing the precision of ECG analysis and improving the ability to assess cardiac conditions.






