Overview
The article addresses the challenges associated with ECG lead placement techniques, highlighting the necessity for accurate cardiac readings to prevent misdiagnoses. It underscores the critical importance of proper electrode positioning, referencing studies that indicate high rates of misplacement and the potential for significant clinical implications.
Furthermore, it introduces the MaxYield™ platform, a technological advancement designed to enhance the accuracy and reliability of ECG analysis. This platform not only improves the precision of electrode placement but also offers substantial benefits for healthcare professionals by facilitating better patient outcomes.
Introduction
The precision of ECG lead placement is not merely a procedural formality; it is essential for accurate diagnosis of heart conditions. Studies indicate that misplacement can result in significant misdiagnoses, making it crucial for healthcare professionals to grasp the intricacies of this process.
This guide explores step-by-step techniques for mastering ECG lead placement, highlighting the vital role of proper execution and preparation. Practitioners often encounter challenges in achieving this accuracy, and innovative technologies may enhance their efforts.
Understand the Basics of ECG Lead Placement
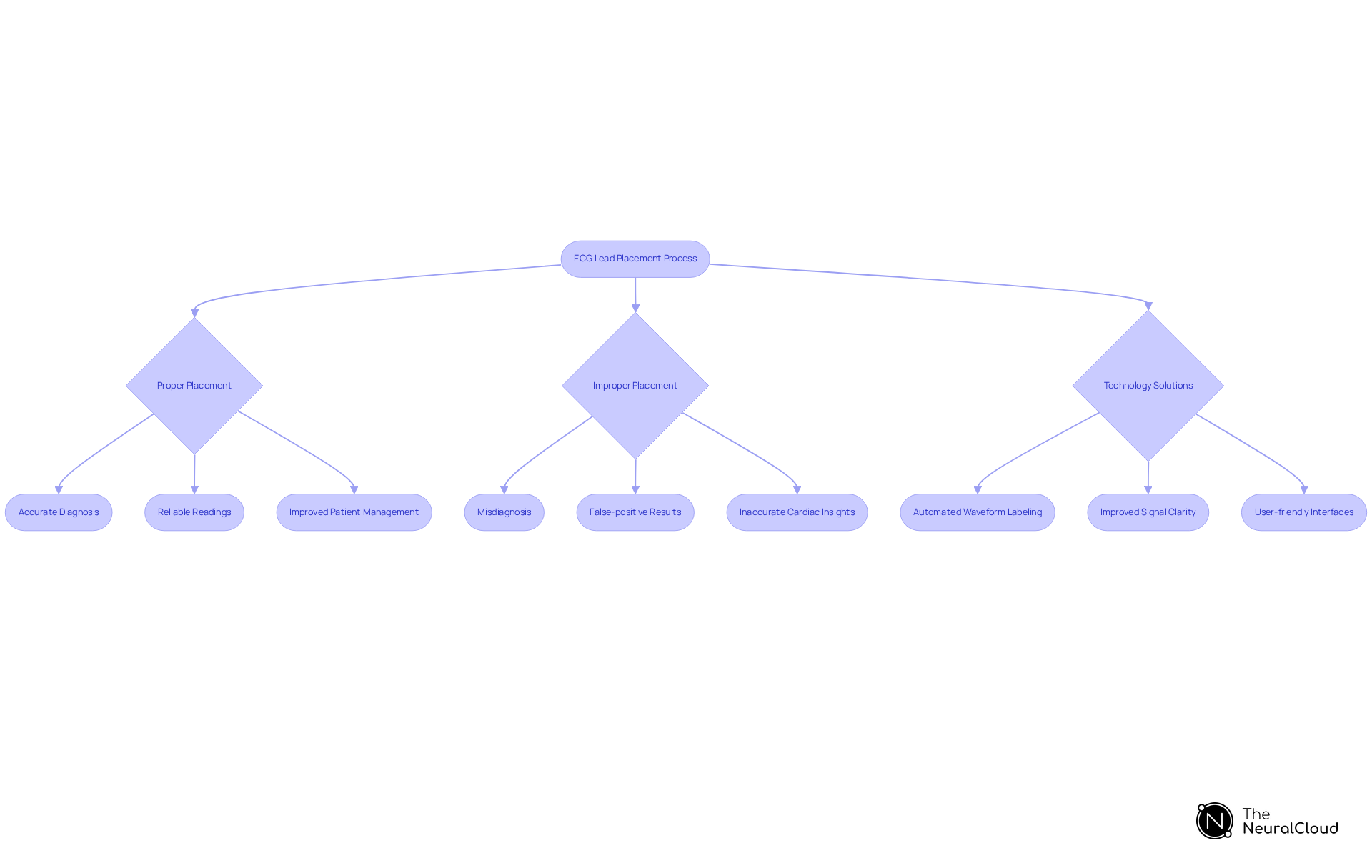
ECG lead placement is a critical procedure that involves positioning electrodes on the patient's body to accurately capture the heart's electrical signals. The standard 12-lead ECG lead placement includes limb electrodes (I, II, III, aVR, aVL, aVF) and precordial electrodes (V1 to V6). Each electrode provides a distinct perspective on the heart's electrical activity, essential for diagnosing various cardiac conditions. For instance, limb electrodes yield insights into the heart's activity in the frontal plane, while precordial electrodes evaluate the horizontal plane, together offering a comprehensive view of cardiac function.
The significance of cannot be overstated. Research indicates that improper ECG lead placement can lead to misdiagnoses, with up to 10.8% of ECGs potentially misclassified as myocardial infarction due to misalignment of the electrodes. Additionally, studies show that nurses misplace electrodes 64% of the time, and cardiologists indicate that proper ECG lead placement for V1 and V2 is achieved in fewer than 20% of cases, highlighting a widespread issue in clinical practice. As Marco Di Muzio from the Department of Clinical and Molecular Medicine remarked, "The level of theoretical knowledge and the level of accuracy in 12-leads ECG positioning must be high in nursing staff to reduce mistaken interpretation, misdiagnosis, patient mismanagement and/or inappropriate procedures."
In clinical settings, the implications of precise ECG lead placement are substantial. For example, incorrect ECG lead placement of V1 and V2 connections can result in false-positive anterior ST elevation, complicating ECG interpretation. Conversely, proper ECG lead placement enhances the reliability of readings, empowering healthcare professionals to make informed decisions based on accurate cardiac insights. The integration of advanced technologies, such as Neural Cloud Solutions' MaxYield™ platform, addresses these challenges by automating the labeling of ECG waveforms and improving overall signal clarity. This supports clinicians in achieving optimal diagnostic outcomes.
The MaxYield™ platform offers several features that enhance ECG analysis:
- Automated waveform labeling
- Improved signal clarity
- User-friendly interfaces
The advantages of these features are clear: they reduce the risk of misdiagnosis, enhance the accuracy of readings, and ultimately improve patient management. By leveraging this technology, healthcare professionals can ensure better diagnostic precision and patient care.
Prepare for ECG Lead Placement
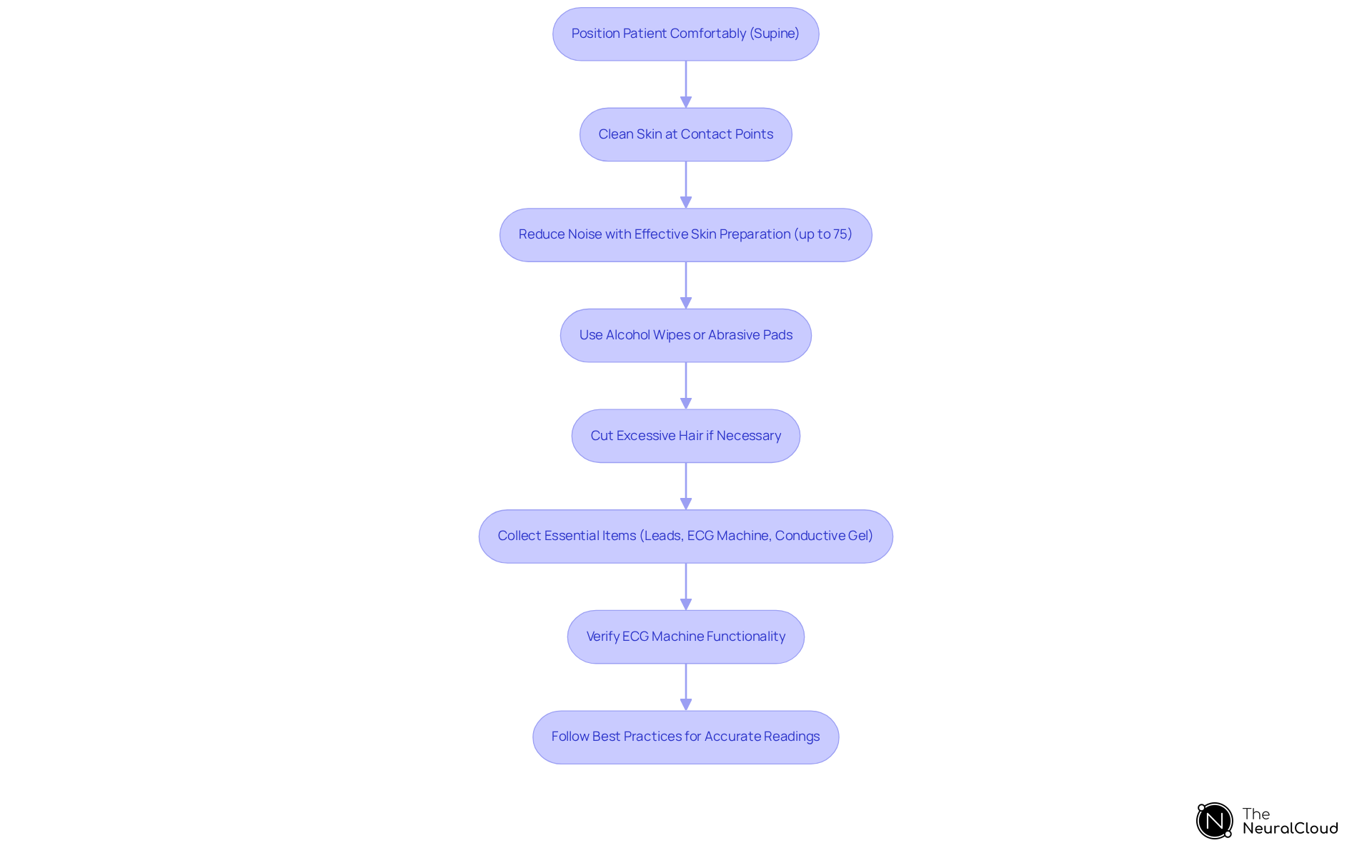
To ensure optimal ECG lead placement, start by positioning the patient comfortably, ideally in a supine position. Thoroughly clean the skin at the contact points to eliminate oils and dirt that can compromise signal quality. Research indicates that effective skin preparation can reduce baseline and alarm noise by up to 75%, significantly enhancing the accuracy of ECG readings. Utilize , particularly in hairy areas, to improve adhesion. If necessary, cut excessive hair rather than shaving, as this can enhance contact without causing irritation to the skin.
Collect all essential items, including leads, the ECG machine, and conductive gel if needed. Prior to use, verify that the ECG machine is functioning correctly and calibrated. This preparation will streamline the process and improve the reliability of the readings. Following best practices in ECG lead placement not only enhances signal quality but also aids in detecting subtle arrhythmias that might otherwise be overlooked.
Execute Accurate ECG Lead Placement
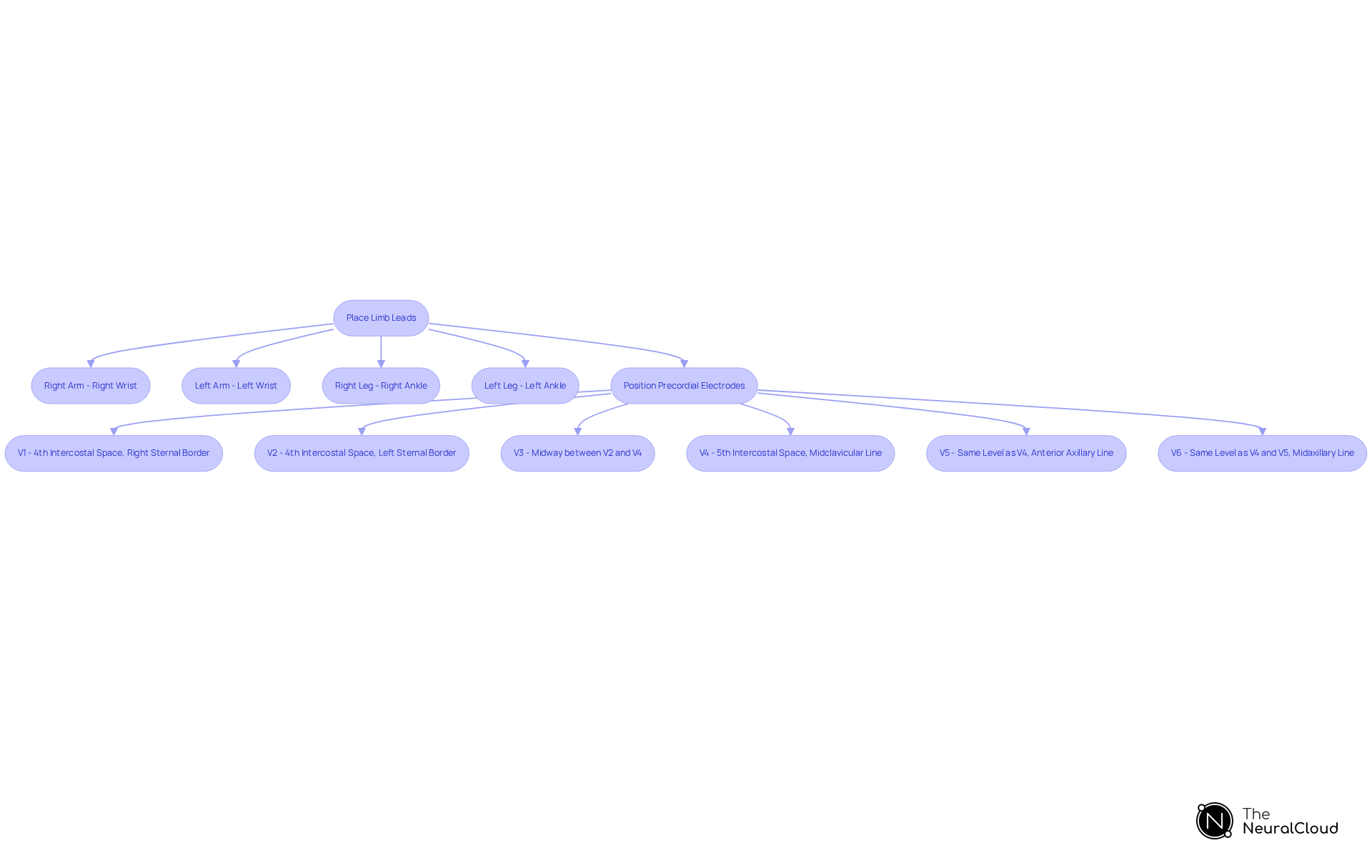
- To ensure , begin by placing the limb leads accurately. Position the right arm sensor on the right wrist, the left arm sensor on the left wrist, the right leg sensor on the right ankle, and the left leg sensor on the left ankle. It is crucial to ensure that the electrodes are securely attached to the skin for optimal performance.
- Following the limb leads, proceed to position the precordial electrodes as part of the ECG lead placement. Start with V1, placing it in the fourth intercostal space at the right sternal border. For V2, position it in the fourth intercostal space at the left sternal border. Continue with V3, which should be placed midway between V2 and V4, located in the fifth intercostal space at the midclavicular line. V5 should be positioned at the same horizontal level as V4, but at the anterior axillary line, while V6 is to be placed at the same level as V4 and V5, but at the midaxillary line. Ensure that each connector is securely attached, maintaining good contact with the skin.
Troubleshoot Common Lead Placement Issues
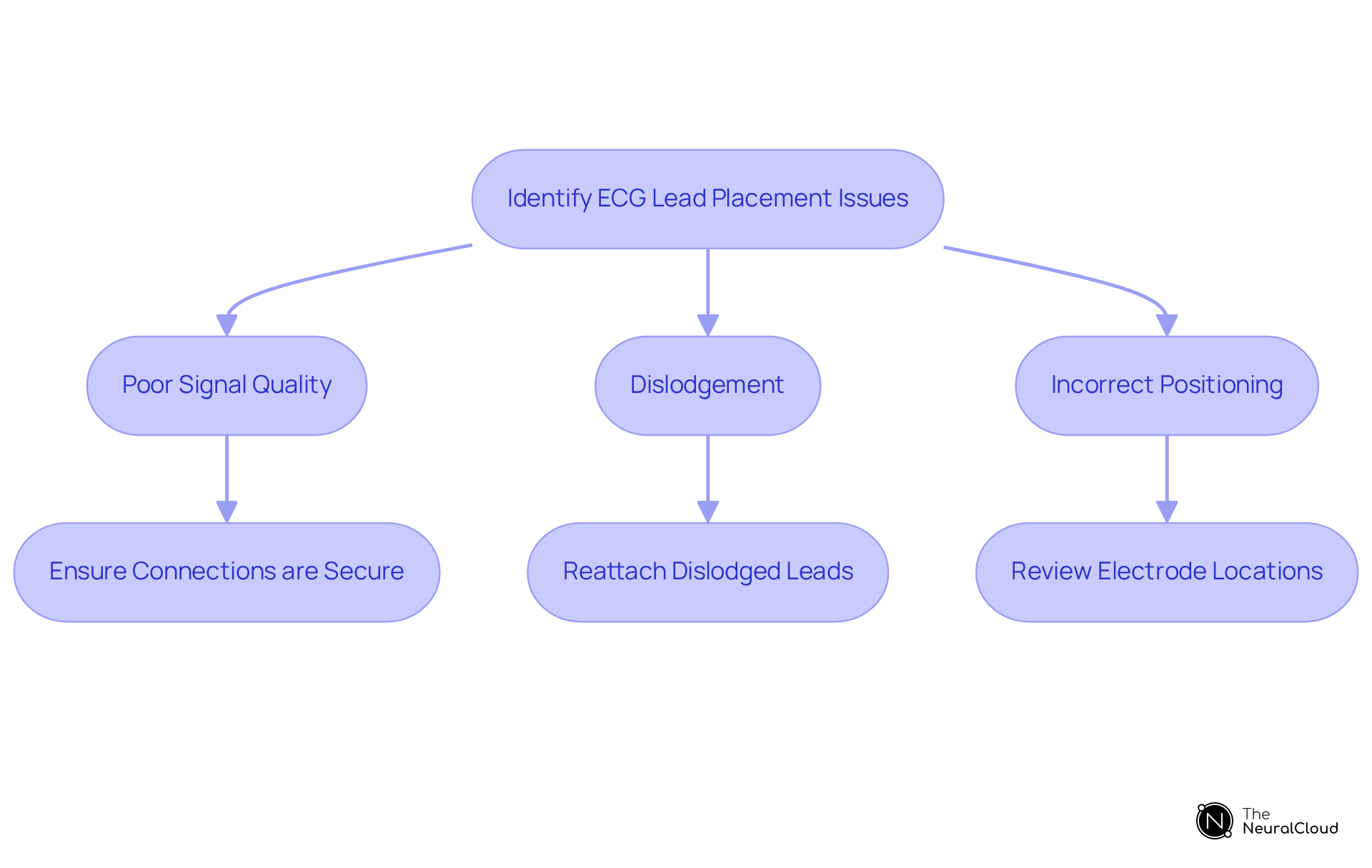
Common challenges during ECG lead placement include issues such as poor signal quality, dislodgement, and incorrect positioning. Statistics indicate that nurses misplace ECG lead placement wires in up to 64% of all cases, highlighting the prevalence of these issues.
To , it is essential to ensure that electrode connections are secure and that the skin is clean and dry before application. If connections become dislodged during the procedure, they should be quickly reattached, confirming their accurate positioning against recognized anatomical landmarks.
In instances of suspected improper ECG lead placement, a thorough review of each electrode's location is crucial. Additionally, patient movement or anxiety can significantly impact signal quality; therefore, encouraging patients to relax and remain still during the recording is vital.
Integrating classroom instruction and regular practice can enhance electrode positioning accuracy. Implementing these strategies can greatly improve the accuracy and reliability of ECG readings. Addressing these common ECG lead placement problems is essential for ensuring high-quality ECG signal acquisition.
Conclusion
Mastering ECG lead placement is essential for accurate cardiac monitoring and diagnosis. This guide emphasizes the importance of precise electrode positioning; even minor errors can lead to significant misinterpretations of a patient's heart health. The integration of advanced technologies, such as the MaxYield™ platform, enhances the reliability of ECG readings. This ensures that healthcare professionals can make informed decisions based on accurate data.
Key insights throughout the article highlight the critical steps in preparing for and executing ECG lead placement. Understanding the anatomy of lead placement and troubleshooting common issues are vital for achieving optimal results. Skin preparation, secure electrode attachment, and patient comfort are paramount, as these factors directly influence the quality of the ECG signals obtained.
Ultimately, mastering ECG lead placement transcends mere technical skill; it is a crucial component of patient care that can greatly affect clinical outcomes. By prioritizing proper techniques and leveraging modern technology, healthcare professionals can enhance their diagnostic capabilities and reduce the risk of misdiagnosis. This ultimately improves patient management. Embracing these practices fosters a culture of excellence in cardiac care and empowers clinicians to deliver the highest standard of healthcare.
Frequently Asked Questions
What is ECG lead placement?
ECG lead placement is the procedure of positioning electrodes on a patient's body to accurately capture the heart's electrical signals. It typically involves standard 12-lead placement, which includes limb electrodes and precordial electrodes.
What are the different types of electrodes used in a standard 12-lead ECG?
The standard 12-lead ECG includes limb electrodes (I, II, III, aVR, aVL, aVF) and precordial electrodes (V1 to V6). Each type of electrode provides a unique perspective on the heart's electrical activity.
Why is accurate ECG lead placement important?
Accurate ECG lead placement is crucial as improper placement can lead to misdiagnoses. Research indicates that up to 10.8% of ECGs may be misclassified as myocardial infarction due to misalignment, and studies show a high rate of misplacement among nurses and cardiologists.
What are the consequences of incorrect ECG lead placement?
Incorrect lead placement, especially for V1 and V2, can result in false-positive anterior ST elevation, complicating ECG interpretation and leading to potential mismanagement of patients.
How can technology assist in improving ECG lead placement?
Technologies like Neural Cloud Solutions' MaxYield™ platform can automate the labeling of ECG waveforms and improve signal clarity, thereby enhancing the reliability of readings and supporting clinicians in making informed decisions.
What features does the MaxYield™ platform offer?
The MaxYield™ platform offers features such as automated waveform labeling, improved signal clarity, and user-friendly interfaces.
What are the benefits of using the MaxYield™ platform?
The platform reduces the risk of misdiagnosis, enhances the accuracy of ECG readings, and ultimately improves patient management and care.






