Overview
This article highlights the critical role of accurately measuring ST segment elevation in ECG readings, which is vital for diagnosing conditions such as ST-Elevation Myocardial Infarction (STEMI). It underscores the challenges faced in ECG analysis, particularly the risk of misinterpretation that can lead to serious clinical consequences.
To ensure reliable ECG interpretation, the article emphasizes the necessity of precise measurement techniques, appropriate equipment, and effective troubleshooting strategies. These features are essential for healthcare professionals who rely on accurate data to make informed decisions.
By adopting these best practices, clinicians can significantly improve their ECG analysis, leading to better patient outcomes. The article serves as a reminder that attention to detail in measurement can make a substantial difference in clinical settings.
Introduction
Understanding the complexities of ST segment elevation is essential for healthcare professionals, as it serves as a critical indicator of myocardial damage and ischemia in patients. Accurate measurement of this ECG phenomenon aids in diagnosing acute coronary syndromes, such as STEMI, and significantly influences patient outcomes through timely interventions.
However, clinicians face challenges due to the potential for misinterpretation and various factors that can affect readings. To ensure accurate measurement of ST segment elevation amidst these complexities, healthcare professionals must adopt systematic approaches and utilize advanced tools.
Understand ST Segment Elevation and Its Clinical Significance
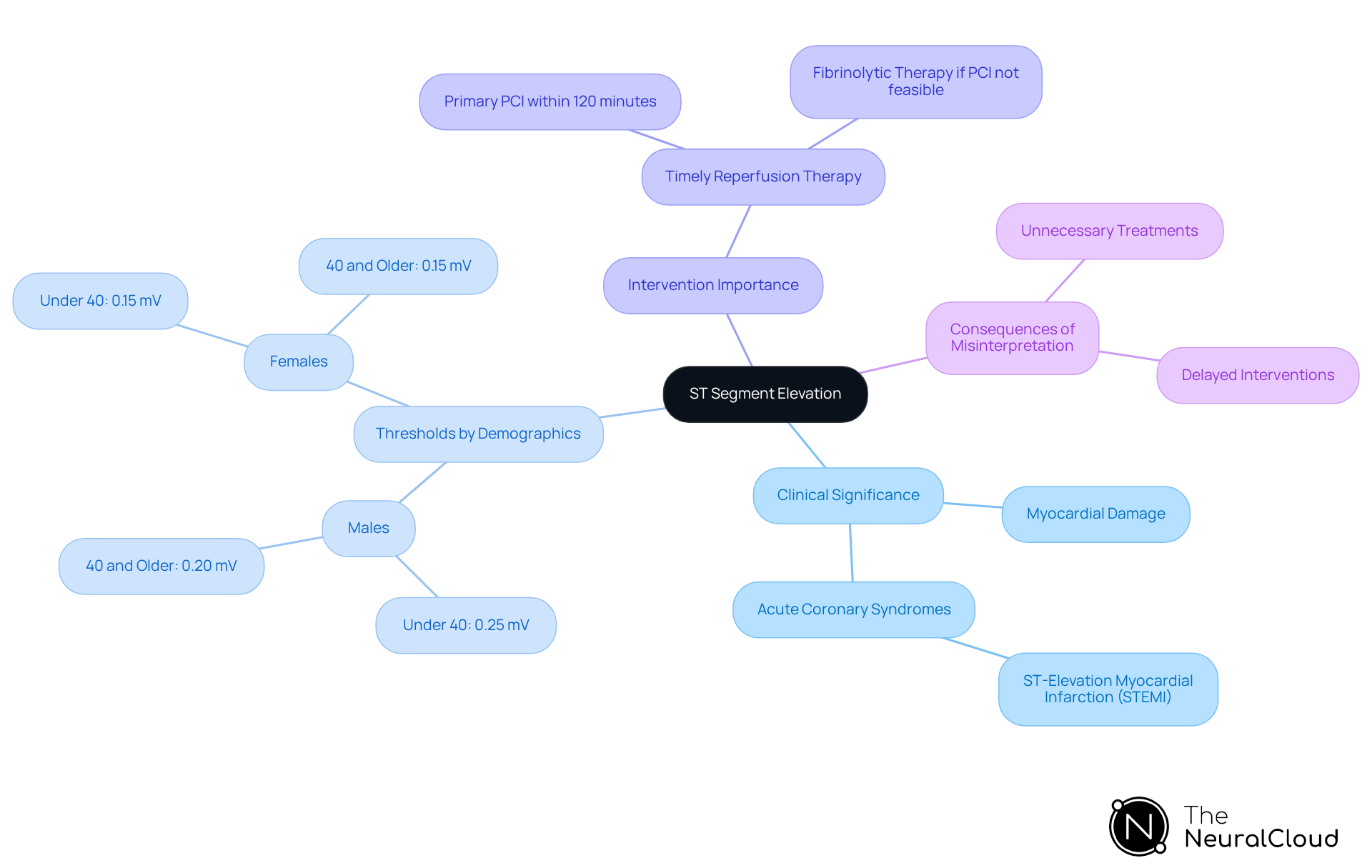
ST segment rise is characterized by an upward deflection in the ST area of an ECG, serving as a crucial indicator of myocardial damage or ischemia. This phenomenon plays a significant role in diagnosing acute coronary syndromes, particularly ST-Elevation Myocardial Infarction (STEMI). Rapid identification of ST wave rise is essential, as it can lead to timely interventions that significantly improve patient outcomes. Recent studies reveal that STEMI constitutes about 30% of all acute coronary syndrome cases, underscoring the necessity for precise ECG interpretation in clinical practice.
Understanding how to measure ST segment elevation and the typical ranges and variations is vital for accurate diagnosis. Factors such as age, sex, and pre-existing health conditions can influence ST interval readings, necessitating a solid grasp of the normal ECG waveform and specific diagnostic criteria. For instance, the notable ST elevation thresholds differ:
- For males under 40, it is set at 0.25 mV in leads V2 and V3.
- For females, the threshold is 0.15 mV.
Misinterpretation of ST changes can lead to unnecessary treatments, highlighting the importance of healthcare professionals being well-versed in the nuances of ST morphology.
Practical examples illustrate the importance of recognizing ST rise in STEMI patients. Immediate reperfusion therapy, such as primary percutaneous coronary intervention (PCI), is recommended within 120 minutes of diagnosis to minimize myocardial damage. Research indicates that timely intervention can lower mortality rates from 9% to 7%. Cardiologists emphasize that understanding ST variations is crucial for effective clinical management, as it aids in differentiating between benign conditions and serious myocardial injury. Thus, mastering how to measure ST segment elevation and interpret its rise is essential for enhancing care in acute coronary syndromes.
Gather Necessary Tools for Accurate Measurement
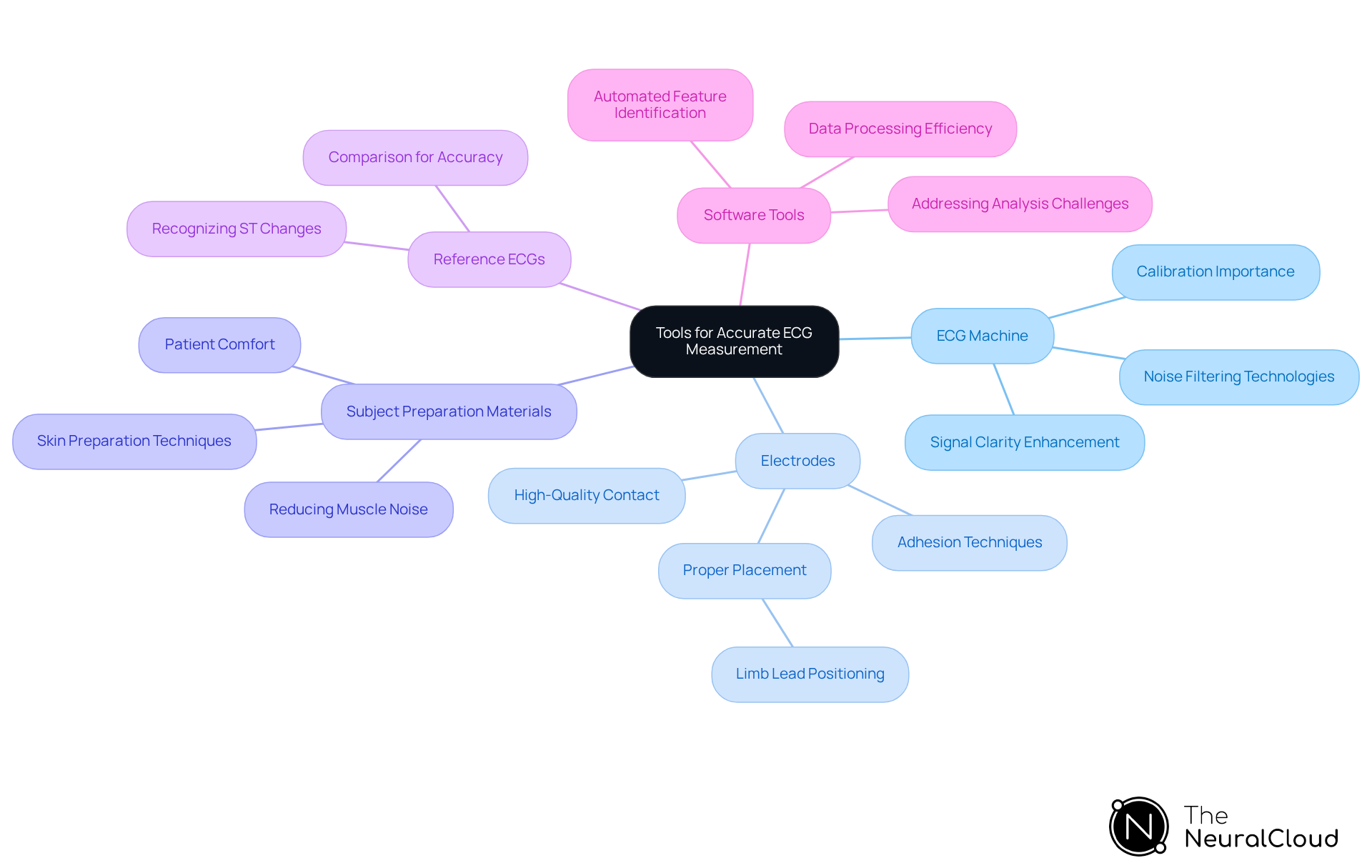
Healthcare professionals face several challenges in ECG analysis when learning how to measure ST segment elevation accurately. These challenges can be effectively addressed by utilizing advanced tools and techniques, particularly the MaxYield™ platform from Neural Cloud Solutions.
-
ECG Machine: A properly calibrated and optimally functioning ECG machine is essential. High-quality machines minimize noise and enhance signal clarity, which is crucial for accurate readings. The MaxYield™ platform incorporates advanced noise filtering technologies, streamlining the process and aligning with gold standard methodologies.
-
Electrodes: High-quality electrodes ensure good contact with the skin, which is vital for accurate readings. For instance, limb lead electrodes should be positioned approximately 7-12 cm above the ankles to avoid diagnostic errors. Misplacement can lead to reduced R-wave amplitude and misinterpretation of results.
-
Subject Preparation Materials: Effective subject preparation is crucial for obtaining high-quality ECG recordings. Ensuring the individual is relaxed and comfortable helps reduce anxiety, which can introduce muscle noise into the readings. Techniques such as lightly abrading the skin to reduce impedance and ensuring the area is free from lotions can significantly improve electrode adhesion and signal quality.
-
Reference ECGs: Access to reference ECGs is advantageous for comparison, assisting in recognizing normal versus abnormal ST changes. This resource helps clinicians make informed decisions based on accurate data.
-
Software Tools: Employing software tools that assist in analyzing ECG data is vital. The MaxYield™ platform automates the identification of key features in the ECG waveform, processing more data in less time and enhancing diagnostic accuracy. This automation addresses challenges in ECG analysis, such as how to measure ST segment elevation, physiological variability, and signal artifacts, ultimately leading to more reliable results.
By adhering to these guidelines and utilizing the features of MaxYield™, healthcare professionals can ensure that their ECG measurements are precise and dependable, ultimately resulting in improved outcomes for individuals.
Follow Step-by-Step Procedures for Measuring ST Segment Elevation
To measure ST segment elevation accurately, follow these essential steps:
- Prepare the Patient: Position the patient comfortably, ideally lying down, and explain the procedure to alleviate any anxiety.
- Electrode Placement: Adhere to the standard 12-lead ECG configuration for electrode placement. Ensure secure attachment to minimize movement artifacts, as improper placement can lead to significant measurement errors. Cardiologists emphasize that proper electrode placement is crucial for reliable ECG interpretation, as even minor deviations can significantly affect the results.
- Obtain the ECG: Initiate the ECG machine and allow it to record for at least 10 seconds to capture a stable reading. Set the machine to the appropriate speed, typically 25 mm/sec, to ensure clarity. Utilizing advanced tools like Neural Cloud Solutions' MaxYield™, which excels in isolating ECG waves from recordings with noise and artifacts, can significantly enhance the quality of the readings by providing clearer data for analysis.
- Identify the ST Portion: After printing the ECG, locate the ST portion in leads most relevant for assessing myocardial ischemia, particularly leads II, III, aVF, and V2-V6.
- Measure the Elevation: Utilize calipers or digital measurement tools to assess the height of the ST segment from the baseline (isoelectric line). The height should be assessed in relation to the standard range, which is typically >1 mm in adjacent leads, with particular thresholds differing by individual demographics. Notably, misplacement of electrodes can occur in up to 30% of cases, leading to inaccurate readings. The MaxYield™ platform's adaptive algorithm continuously improves its accuracy with each use, helping to mitigate these issues.
- Document Findings: Record all measurements and observations, including the lead used and the individual's condition during the measurement. This documentation is vital for clinical decision-making and future reference.
Recent methods for assessing ST elevation utilize sophisticated digital instruments that improve precision and minimize human mistakes, guaranteeing prompt and efficient care for individuals. By identifying complex patterns or subtle deviations that could suggest a coronary event, AI, especially through solutions like MaxYield™, can enhance clinical decision-making in chest pain groups.

Troubleshoot Common Issues in ST Segment Elevation Measurement
When measuring ST segment elevation, several common issues may arise, along with effective troubleshooting strategies:
-
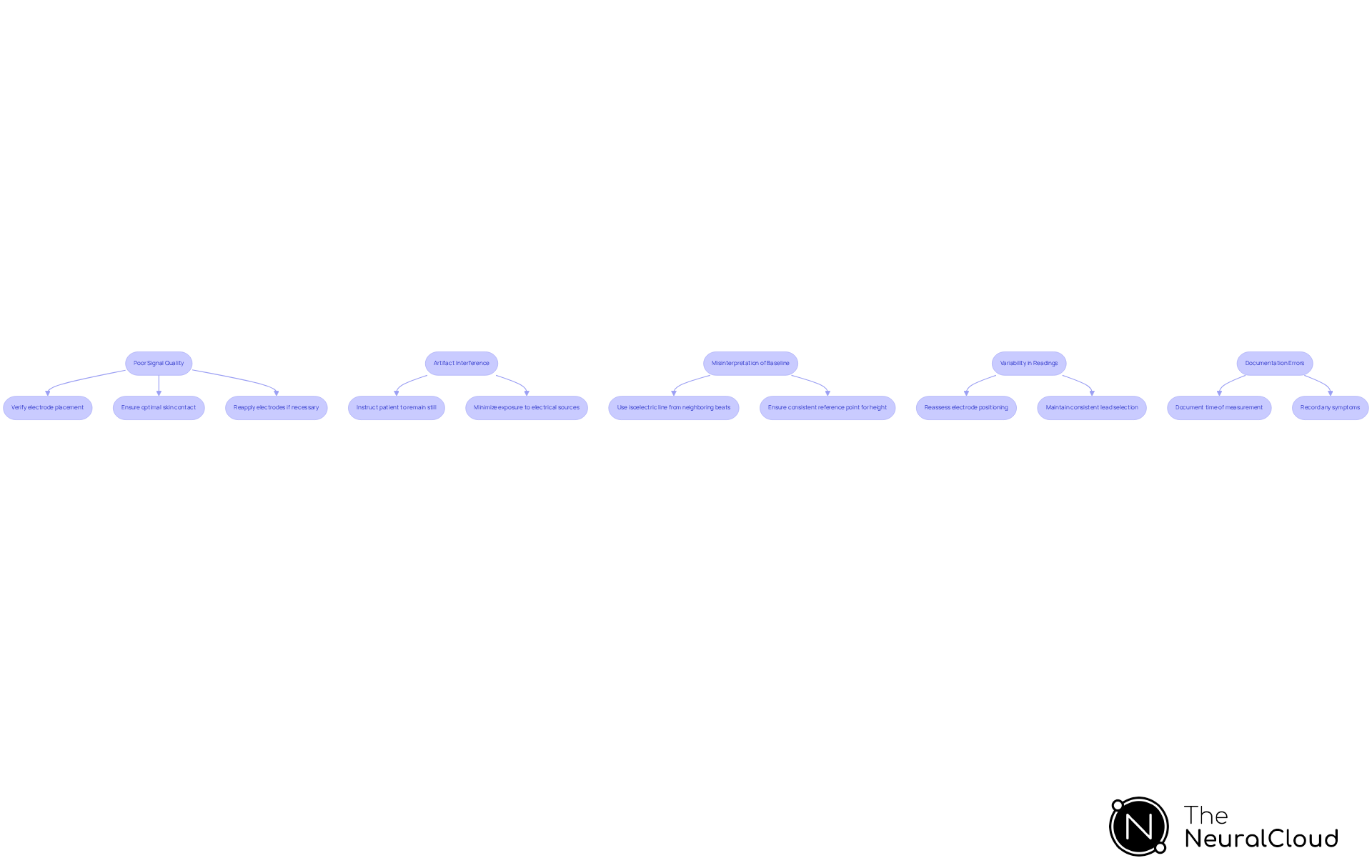
Poor Signal Quality: Noisy or unclear ECG signals can significantly hinder accurate measurements. To improve signal quality, verify electrode placement and ensure optimal skin contact. If necessary, reapply electrodes to enhance conductivity.
-
Artifact Interference: Movement or electrical interference often introduces artifacts that can distort readings. It is crucial to instruct the patient to remain still during the recording and to minimize exposure to external electrical sources, which can exacerbate noise.
-
Misinterpretation of Baseline: An unclear baseline can lead to inaccurate ST segment measurements. Employ the isoelectric line from neighboring beats to create a dependable baseline, ensuring that the reference point for height is consistent.
-
Variability in Readings: Significant discrepancies between leads may indicate issues with electrode placement. Reassess the positioning of electrodes and maintain consistent lead selection for accurate comparisons across measurements.
-
Documentation Errors: Accurate documentation of findings is essential. Document all pertinent details, including the time of measurement and any symptoms, as this information is essential for follow-up and treatment choices.
Addressing these issues not only enhances how to measure ST segment elevation accurately but also improves patient outcomes by reducing the likelihood of misdiagnosis due to artifact interference. For instance, studies have shown that high false alarm rates in critical care settings, where 88.8% of arrhythmia alarms were deemed false or non-actionable, can be mitigated through improved signal quality management and tailored approaches to artifact detection. By implementing these strategies, healthcare professionals can ensure more reliable ECG readings and enhance clinical decision-making.
Conclusion
Mastering the measurement of ST segment elevation is essential for healthcare professionals, as it significantly influences the diagnosis and management of acute coronary syndromes. This guide emphasizes the importance of understanding ST segment elevation, the necessary tools for accurate measurement, and the step-by-step procedures for effective ECG analysis. With a solid grasp of these concepts, clinicians can enhance their diagnostic capabilities and improve patient outcomes.
Key insights discussed include the clinical significance of ST segment elevation in identifying myocardial damage, specific thresholds for different demographics, and advanced tools available, such as the MaxYield™ platform. This platform aids in achieving precise readings, addressing common challenges in ECG analysis. Furthermore, practical troubleshooting strategies are provided to tackle issues that may arise during the measurement process, reinforcing the need for meticulous attention to detail in ECG interpretation.
The MaxYield™ platform features:
- Precision Measurement: Ensures accurate ST segment elevation readings.
- User-Friendly Interface: Simplifies the ECG analysis process for healthcare professionals.
- Real-Time Data Analysis: Provides immediate feedback to enhance clinical decision-making.
Ultimately, the ability to accurately measure ST segment elevation not only enhances clinical decision-making but also plays a crucial role in timely interventions that can save lives. By continually refining skills and utilizing the right tools, healthcare professionals can ensure they deliver the highest standard of care in cardiology. Embracing these best practices will lead to improved diagnostic accuracy and better health outcomes for patients experiencing acute coronary syndromes.
Frequently Asked Questions
What is ST segment elevation and why is it clinically significant?
ST segment elevation is characterized by an upward deflection in the ST area of an ECG, indicating myocardial damage or ischemia. It is crucial for diagnosing acute coronary syndromes, particularly ST-Elevation Myocardial Infarction (STEMI).
How common is STEMI in acute coronary syndrome cases?
STEMI constitutes about 30% of all acute coronary syndrome cases, highlighting the importance of precise ECG interpretation in clinical practice.
What factors can influence ST interval readings?
Factors such as age, sex, and pre-existing health conditions can influence ST interval readings, making it essential to understand the normal ECG waveform and specific diagnostic criteria.
What are the ST elevation thresholds for males and females?
For males under 40, the ST elevation threshold is set at 0.25 mV in leads V2 and V3, while for females, the threshold is 0.15 mV.
What are the consequences of misinterpreting ST changes?
Misinterpretation of ST changes can lead to unnecessary treatments, emphasizing the need for healthcare professionals to be well-versed in the nuances of ST morphology.
What is the recommended treatment for STEMI patients upon diagnosis?
Immediate reperfusion therapy, such as primary percutaneous coronary intervention (PCI), is recommended within 120 minutes of diagnosis to minimize myocardial damage.
How does timely intervention affect mortality rates in STEMI patients?
Timely intervention can lower mortality rates from 9% to 7%, underscoring the importance of rapid identification and treatment of ST segment elevation.
Why is it important for cardiologists to understand ST variations?
Understanding ST variations is crucial for effective clinical management, as it helps differentiate between benign conditions and serious myocardial injury.






