Overview
Hyperacute T-waves serve as essential indicators of myocardial ischemia, identifiable by their broad, symmetrical shape and heightened amplitude. These features often appear before ST-segment elevation in instances of acute coronary occlusion. The article underscores their clinical significance by illustrating how early detection can facilitate quicker diagnoses and enhance patient outcomes, particularly in acute cardiac care scenarios. By recognizing these critical signs, healthcare professionals can intervene more effectively, ultimately improving the quality of care provided to patients experiencing acute cardiac events.
Introduction
Hyperacute T-waves are a crucial early warning sign in cardiac care, often manifesting as broad, symmetrical shapes with increased amplitude during the early stages of myocardial ischemia. Their timely identification can significantly accelerate the diagnosis of acute coronary occlusion, potentially leading to life-saving interventions.
However, clinicians face the challenge of recognizing these subtle yet vital indicators amidst a multitude of other ECG abnormalities. Therefore, understanding the characteristics and interpretation of hyperacute T-waves is essential for healthcare professionals who aim to enhance patient outcomes in acute cardiac situations.
Define Hyperacute T-Waves and Their Clinical Relevance
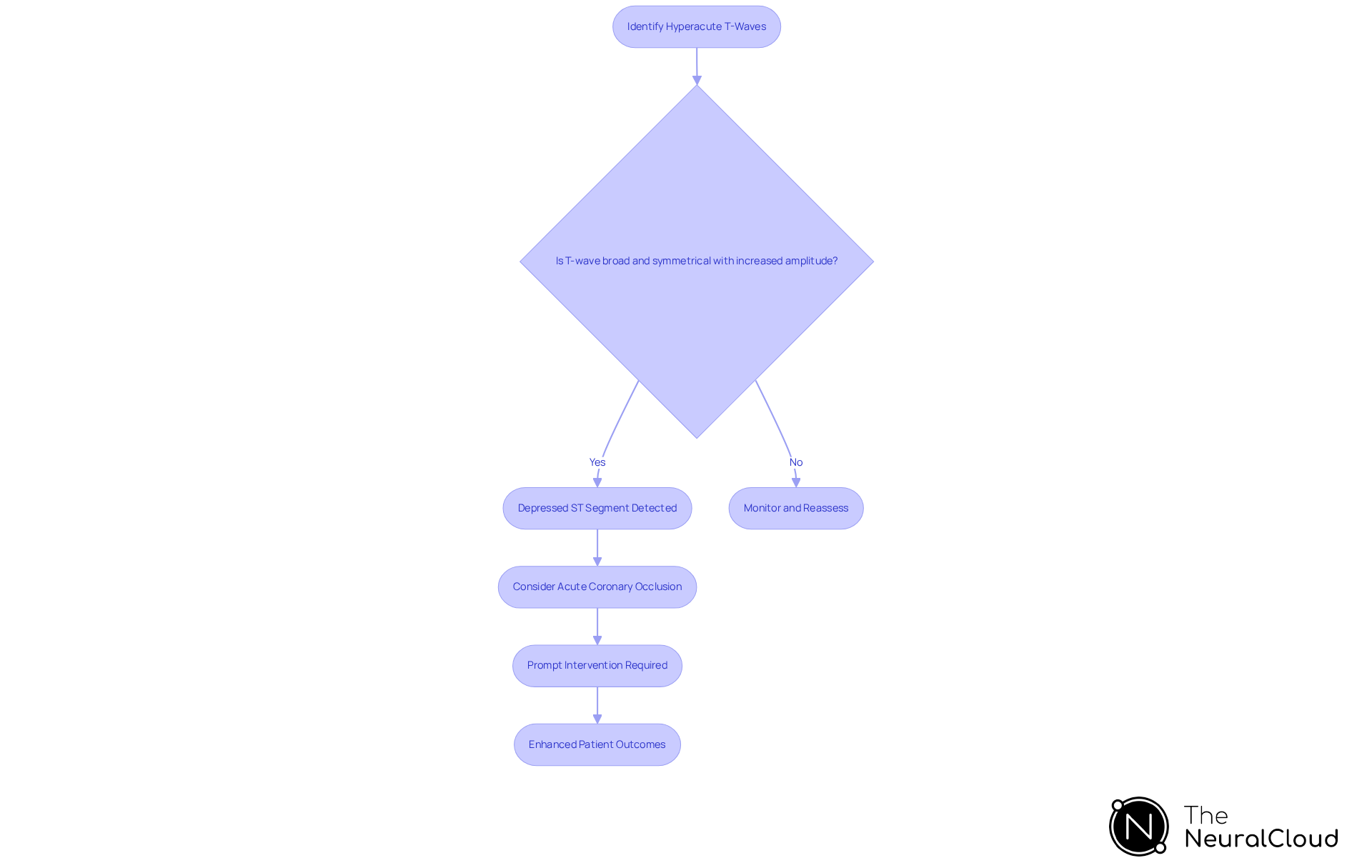
Hyperacute T-waves are characterized by broad, symmetrical shapes with increased amplitude, typically observed in the early stages of myocardial ischemia. These specific hyperacute T-waves often accompany a depressed ST segment and can precede ST-segment elevation, marking them as critical indicators for diagnosing acute coronary occlusion. The clinical significance of hyperacute T-waves cannot be overstated; their detection is crucial for directing prompt interventions, particularly in cases of suspected myocardial infarction (MI). Research has shown that identifying sharp waveforms can lead to a diagnosis up to three hours faster than conventional techniques, significantly influencing patient outcomes.
Cardiologists emphasize the importance of hyperacute T-waves among these electrical signals in acute cardiac care. As one specialist noted, 'Identifying sharp deflections like hyperacute T-waves as STEMI equivalents underscores the critical need for prompt intervention to enhance patient outcomes.' This reinforces the necessity for clinicians to remain vigilant in , as they can determine urgent treatment strategies.
Recent case analyses further highlight the clinical relevance of hyperacute T-waves in the context of rapid cardiac repolarization during acute coronary blockage. For instance, a review focused on sharp waveforms advocates for the integration of advanced technologies, such as AI-driven ECG models, to enhance diagnostic accuracy. These models aid healthcare professionals in accurately detecting subtle ischemic patterns that may be difficult to identify through standard evaluations.
In summary, the ability to recognize sharp deflections, particularly hyperacute T-waves, is essential for the prompt and effective management of acute coronary blockage, underscoring their role as a vital component in the electrocardiographic assessment of patients presenting with chest pain.
Identify Key Characteristics of Hyperacute T-Waves
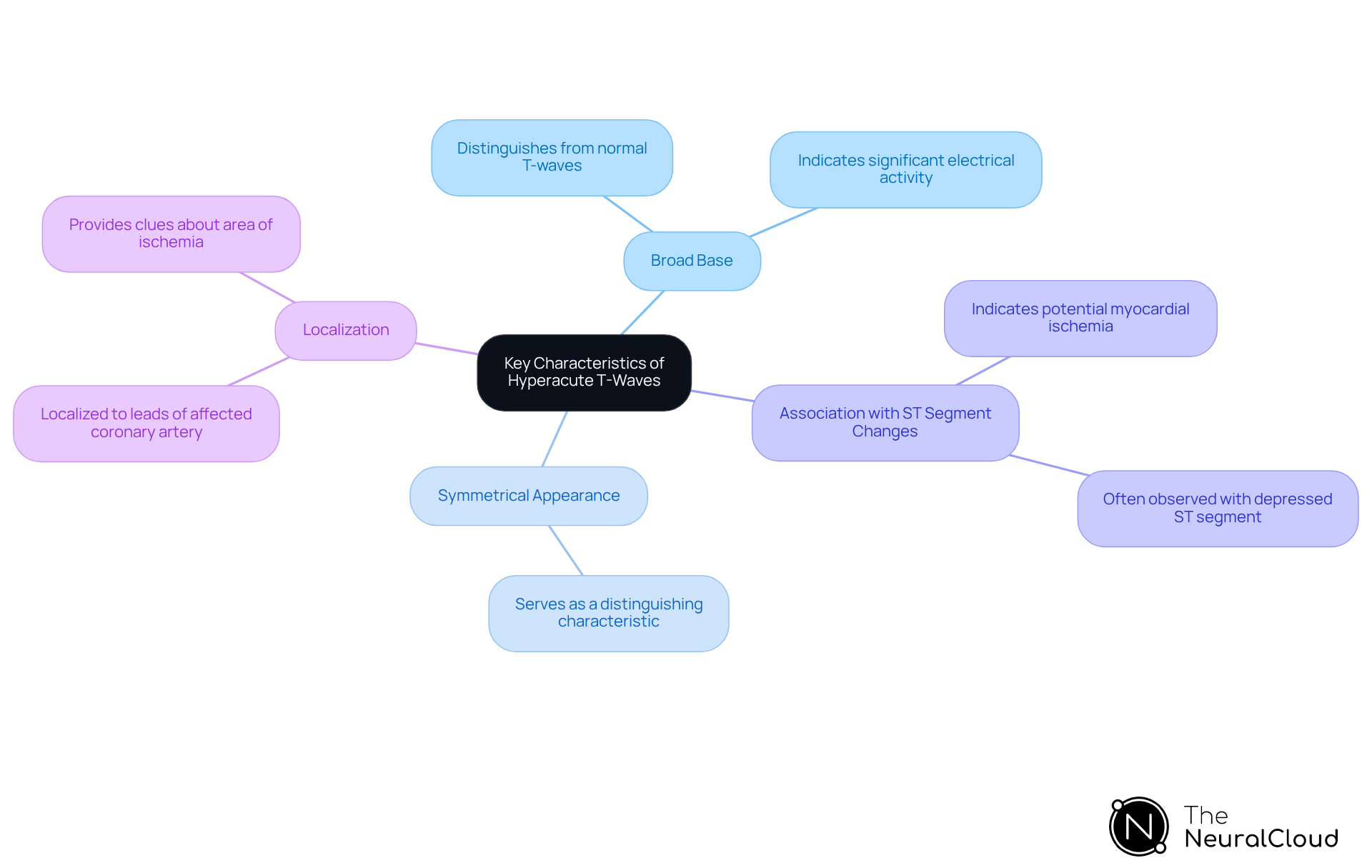
Key characteristics of hyperacute T-waves include:
- Broad Base: Hyperacute T-waves typically exhibit a wide base, which distinguishes them from normal T-waves. The of hyperacute T-waves indicates that these waveforms are often taller than normal, reflecting significant electrical activity in the myocardium.
- Symmetrical Appearance: Unlike other T-wave irregularities, hyperacute T-waves are typically symmetrical, serving as a distinguishing characteristic.
- Association with ST Segment Changes: Hyperacute T-waves are frequently observed alongside a depressed ST segment, which can further indicate myocardial ischemia.
- Localization: Hyperacute T-waves are often localized to the leads corresponding to the affected coronary artery, providing clues about the area of ischemia.
Identifying these traits is essential for distinguishing sharp waves from other conditions, such as hyperkalemia, which can exhibit peaked waves but have different clinical implications.
Guide to Interpreting Hyperacute T-Waves in ECGs
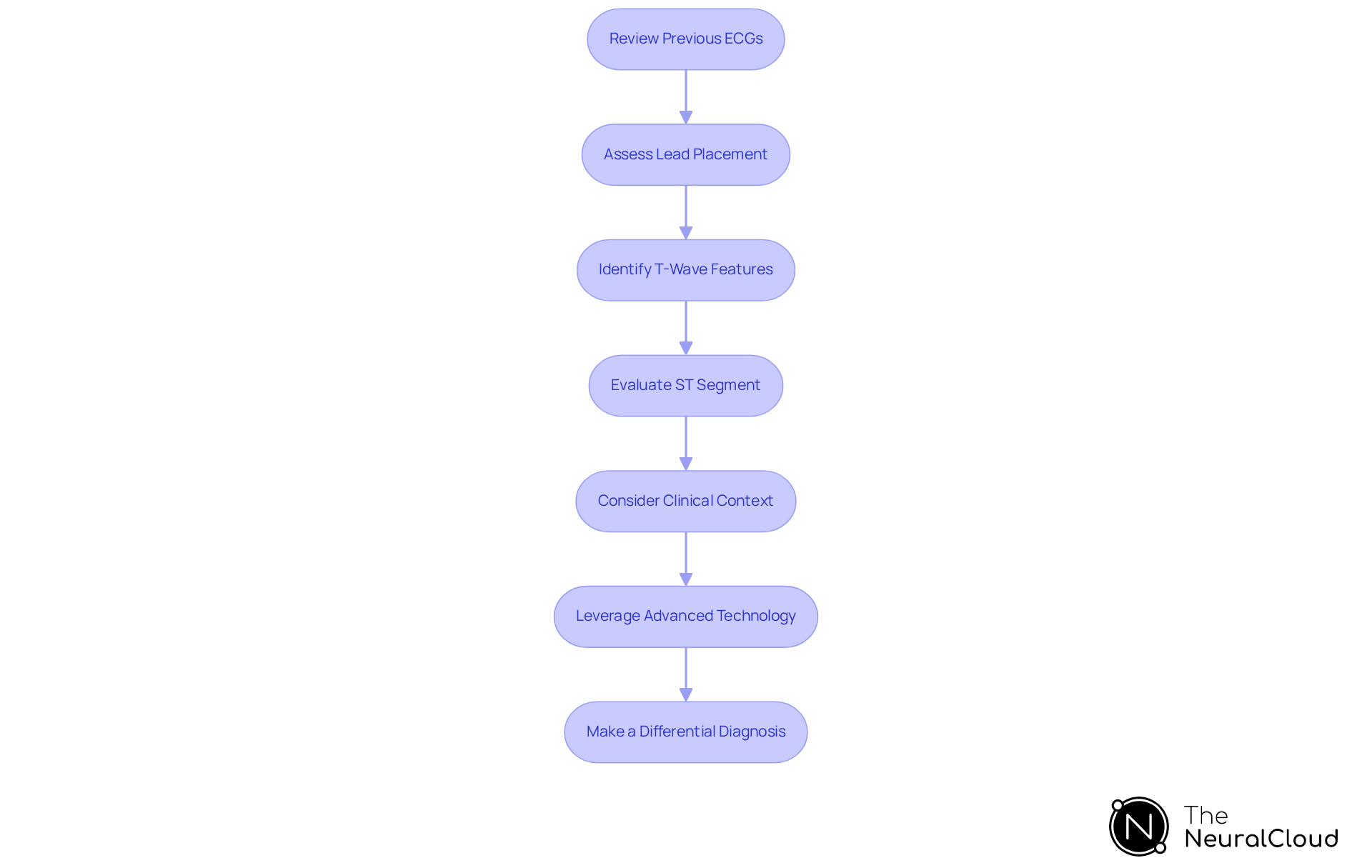
To effectively interpret hyperacute T-waves in ECGs, follow these steps:
- Review Previous ECGs: Compare the current ECG with previous recordings to identify any changes in T-wave morphology. Early detection of alterations can be crucial for diagnosis.
- Assess Lead Placement: Ensure that the ECG leads are correctly positioned. Misplacement can lead to significant misinterpretation of T-wave changes, with studies indicating that improper lead placement contributes to a notable percentage of ECG misinterpretations.
- Identify T-Wave Features: Look for broad-based, symmetrical T-forms with increased amplitude, particularly in the anterior leads (V2-V4), where sharply peaked T-forms are most prominent. These characteristics are critical indicators of potential myocardial ischemia.
- Evaluate ST Segment: Check for any associated ST segment changes, such as elevation or depression. These can further support the diagnosis of myocardial ischemia. The presence of ST segment alterations alongside hyperacute T-waves is often indicative of acute coronary syndrome.
- Consider Clinical Context: Correlate the ECG findings with the individual's clinical presentation, including symptoms of chest pain, shortness of breath, or risk factors for coronary artery disease. This comprehensive method ensures that the ECG interpretation aligns with the individual's overall clinical picture.
- Leverage Advanced Technology: Utilize Neural Cloud Solutions' MaxYield™ platform, which employs a continuous learning model to enhance ECG analysis accuracy and efficiency. This filters noise and improves diagnostic yield, allowing clinicians to focus on critical T-wave characteristics without the burden of manual tasks. For practical application, clinicians can access user manuals that provide step-by-step guidance on utilizing the platform effectively in various clinical scenarios.
- Make a Differential Diagnosis: Differentiate rapid wave changes from other wave irregularities, such as those observed in hyperkalemia or pericarditis. Accurate differentiation is essential to avoid misdiagnosis and ensure appropriate management.
By following this guide and utilizing advanced AI technology, clinicians can improve their capacity to identify and interpret acute heart wave patterns, resulting in timely and efficient care management. Case studies have shown that early identification of hyperacute T-waves can significantly impact treatment outcomes in patients presenting with acute chest pain, as illustrated in the case titled 'Hyperacute T-waves: Distinguishing Early MI from Other Big T Wave Abnormalities.
Conclusion
Recognizing hyperacute T-waves is essential for effective cardiac care, especially in cases of acute myocardial ischemia. These distinctive waveforms serve as critical indicators that can significantly expedite the diagnosis and treatment of conditions such as myocardial infarction. By understanding the characteristics and implications of hyperacute T-waves, healthcare professionals can enhance their diagnostic skills and ultimately improve patient outcomes.
This article explores the defining features of hyperacute T-waves, including their broad base, symmetrical appearance, and association with ST segment changes. It underscores the importance of careful interpretation of ECGs, which involves reviewing previous readings and considering the clinical context. The integration of advanced technologies, such as AI-driven ECG analysis, is highlighted as a means to increase diagnostic accuracy and efficiency, enabling clinicians to focus on crucial T-wave characteristics.
In summary, the significance of hyperacute T-waves in acute cardiac care is paramount. By prioritizing the recognition and interpretation of these waveforms, clinicians can ensure timely interventions that are vital for patient survival and recovery. Embracing innovative tools and adhering to best practices in ECG analysis will empower healthcare providers to make informed decisions, ultimately leading to better management of acute coronary syndromes and improved patient outcomes.
Frequently Asked Questions
What are hyperacute T-waves?
Hyperacute T-waves are characterized by broad, symmetrical shapes with increased amplitude, typically observed in the early stages of myocardial ischemia.
What is the clinical significance of hyperacute T-waves?
Hyperacute T-waves are critical indicators for diagnosing acute coronary occlusion and their detection is crucial for directing prompt interventions, particularly in cases of suspected myocardial infarction (MI).
How do hyperacute T-waves relate to ST-segment changes?
Hyperacute T-waves often accompany a depressed ST segment and can precede ST-segment elevation, marking them as significant in the assessment of myocardial ischemia.
How does the identification of hyperacute T-waves impact patient outcomes?
Research indicates that identifying hyperacute T-waves can lead to a diagnosis up to three hours faster than conventional techniques, significantly influencing patient outcomes.
What do cardiologists say about the importance of hyperacute T-waves?
Cardiologists emphasize that recognizing hyperacute T-waves as STEMI equivalents is crucial for prompt intervention, which enhances patient outcomes.
What advancements are being integrated to improve the detection of hyperacute T-waves?
Advanced technologies, such as AI-driven ECG models, are being integrated to enhance diagnostic accuracy and aid in detecting subtle ischemic patterns that may be difficult to identify through standard evaluations.
Why is recognizing hyperacute T-waves essential in acute cardiac care?
Recognizing hyperacute T-waves is essential for the prompt and effective management of acute coronary blockage, underscoring their role in the electrocardiographic assessment of patients presenting with chest pain.






