Overview
The article provides a comprehensive overview of the diagnosis and management of inferior infarcts, which are characterized by a blockage in the right coronary artery that leads to reduced blood flow to the heart's lower wall. It highlights the critical role of timely diagnosis, emphasizing the significance of ECG findings and a thorough medical history.
Immediate treatment protocols, including reperfusion therapy and medication management, are discussed as essential strategies to enhance patient outcomes. Evidence supports the notion that prompt intervention results in improved clinical results, reinforcing the urgency of effective management in these cases.
Introduction
An inferior infarct, often resulting from a blockage in the right coronary artery, presents significant challenges in both diagnosis and management. Understanding its key characteristics—such as symptoms, ECG findings, and the importance of timely intervention—can drastically improve patient outcomes. The complexity of symptoms, particularly in women, coupled with the critical need for rapid diagnosis, raises the question: how can healthcare professionals ensure they are prepared to effectively manage this condition? This guide provides a comprehensive, step-by-step approach to diagnosing and treating inferior infarcts. It equips clinicians with the knowledge and tools necessary to navigate this critical aspect of cardiac care.
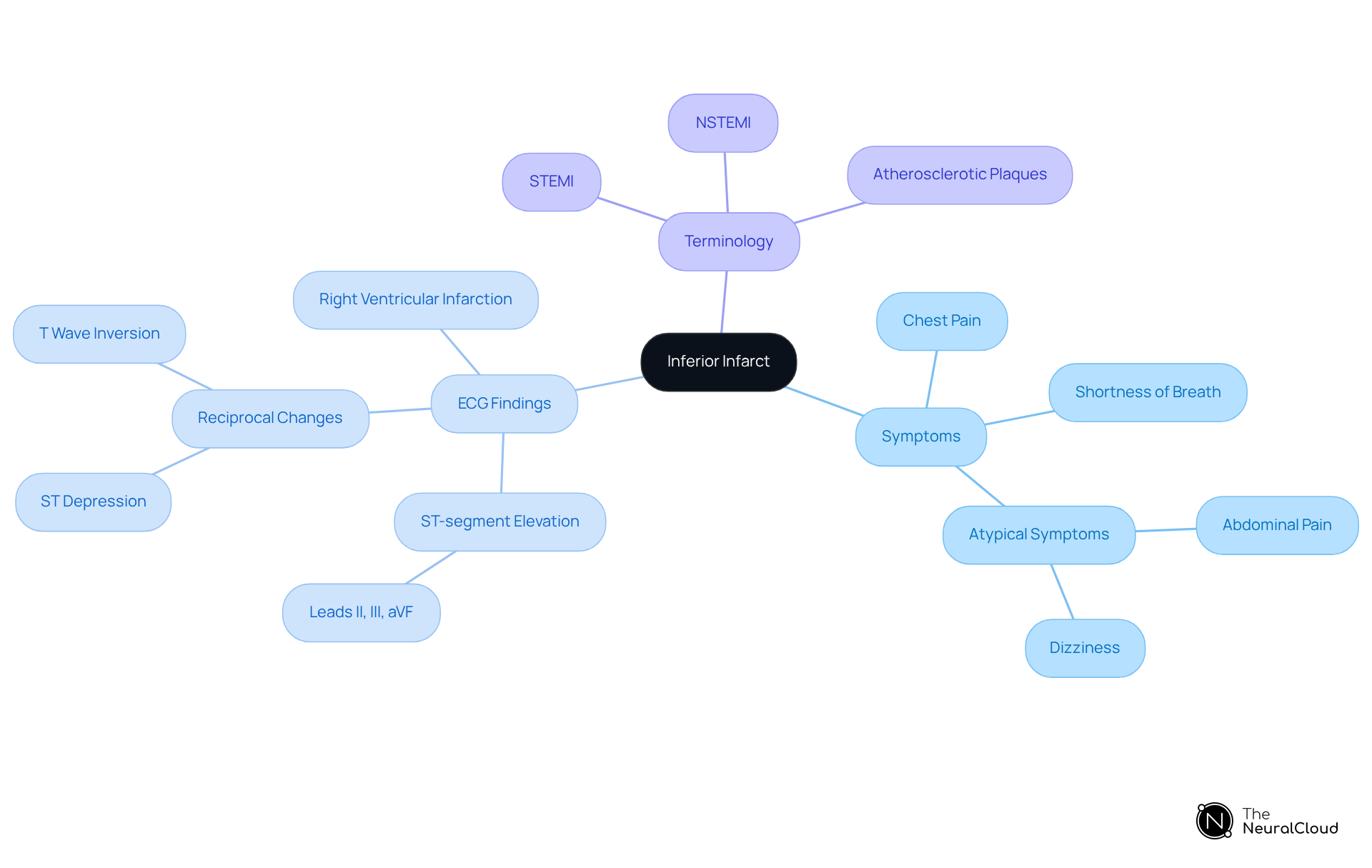
Define Inferior Infarct: Key Characteristics and Terminology
An inferior infarct occurs due to a blockage in the right coronary artery (RCA), leading to reduced blood flow to the lower wall of the heart. Key characteristics include symptoms, [ECG findings](https://theneuralcloud.com/post/10-essential-ecg-measurements-for-health-tech-developers), and terminology.
Symptoms: Patients typically present with chest pain, shortness of breath, and diaphoresis. Notably, women may exhibit atypical symptoms such as abdominal pain or dizziness, complicating diagnosis.
ECG Findings: The hallmark of lower MIs is in leads II, III, and aVF, indicating lower wall involvement. Reciprocal changes, such as ST depression and T wave inversion in leads I and aVL, are also common. In some cases, marked ST elevation in these leads may suggest right ventricular infarction, necessitating the use of right-sided leads for confirmation.
Terminology: Inferior infarct classifications include STEMI (ST-Elevation Myocardial Infarction) or NSTEMI (Non-ST-Elevation Myocardial Infarction) depending on the specific ECG findings. Approximately 70% of fatal acute myocardial infarction (AMI) cases are attributed to occlusion caused by atherosclerotic plaques, underscoring the importance of timely intervention. Individuals who undergo percutaneous coronary intervention (PCI) within 90 minutes of arrival have better outcomes, highlighting the critical need for efficient clinical workflows.
Comprehending these traits is essential for the quick diagnosis and management of inferior infarcts, as timely intervention can greatly enhance individual outcomes. Recent studies suggest that individuals who undergo PCI within 90 minutes of arrival have better outcomes, emphasizing the necessity for efficient clinical workflows. The MaxYield™ platform can enhance diagnostic yield by automating ECG analysis, allowing healthcare professionals to focus on critical decision-making.
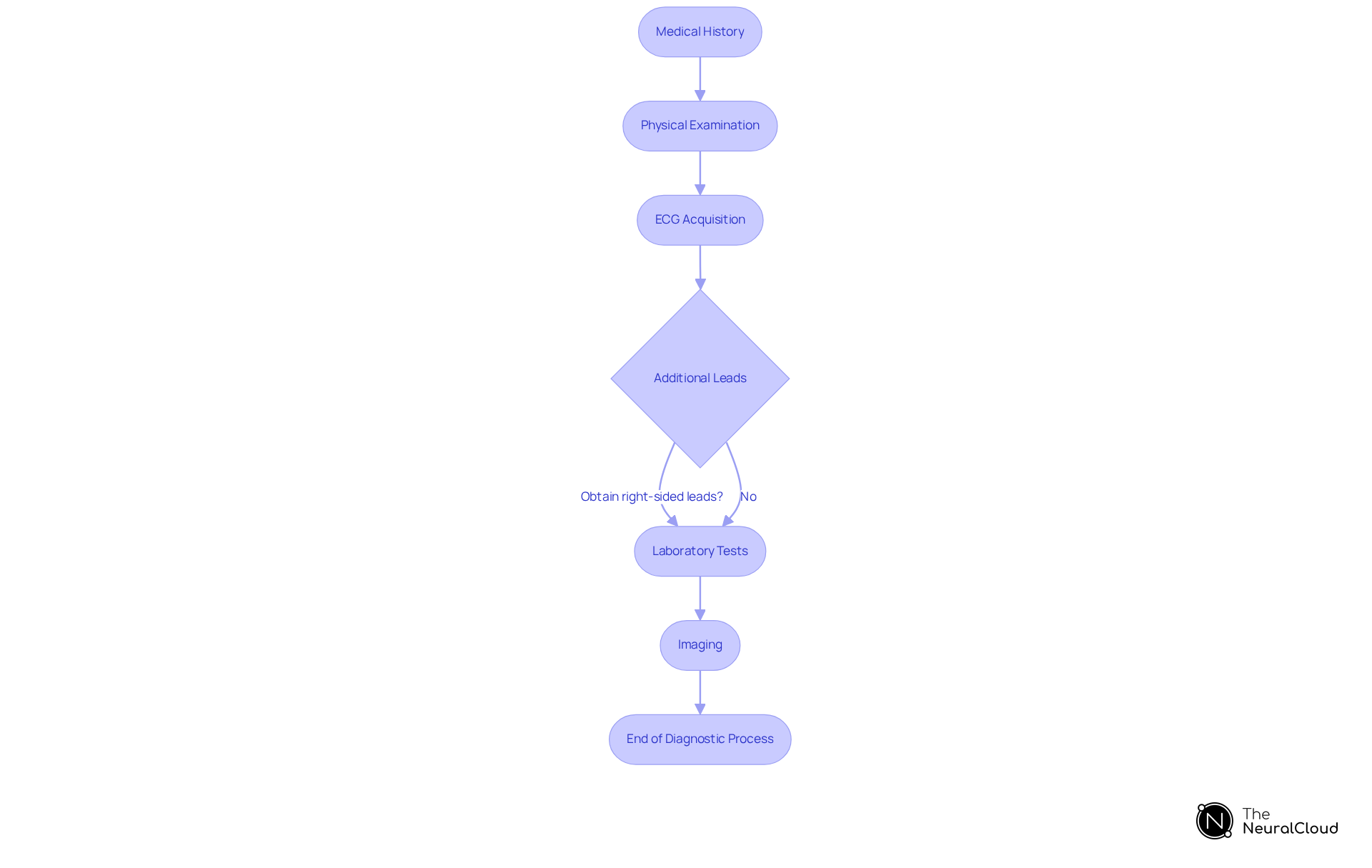
Diagnose Inferior Infarct: Step-by-Step Diagnostic Process
To accurately diagnose an inferior myocardial infarction, follow these structured steps:
- Medical History: Gather comprehensive details about symptoms, particularly the characteristics and duration of chest pain, as this can provide essential insights into the individual's condition.
- Physical Examination: Evaluate vital signs and conduct a thorough cardiovascular examination to identify any signs of heart failure or arrhythmias, which may indicate the severity of the situation.
- ECG Acquisition: Secure a 12-lead ECG within 10 minutes of the patient's presentation. Focus on identifying:
- ST-segment elevation in leads II, III, and aVF, indicative of inferior STEMI.
- Reciprocal ST-segment depression in leads I and aVL, which can further support the diagnosis.
- Additional Leads: If inferior STEMI is suspected, consider obtaining right-sided leads (V3R and V4R) to assess for potential right ventricular involvement, as this can significantly impact management strategies.
- Laboratory Tests: Order cardiac biomarkers, such as troponin, to confirm heart damage. A rise in troponin levels typically occurs within 2-3 hours of heart muscle injury, peaking within 1-2 days, making it a vital component of the diagnostic process.
- Imaging: If necessary, perform echocardiography to assess for wall motion abnormalities, which can provide further insight into the extent of heart tissue damage.
Incorporating the Sgarbossa criteria can enhance diagnostic accuracy, particularly in individuals with left bundle branch block (LBBB), where the sensitivity of the original criteria is only 49%, but its specificity exceeds 90%. As Dmitriy Scherbak notes, "Left bundle branch block (LBBB) is a cardiac conduction disorder that affects the left bundle branch of the heart's conduction system, leading to delayed or abnormal electrical impulses through the ventricles." By adhering to this organized method, healthcare specialists can ensure precise diagnosis and timely treatment, ultimately improving outcomes for individuals experiencing inferior infarct.
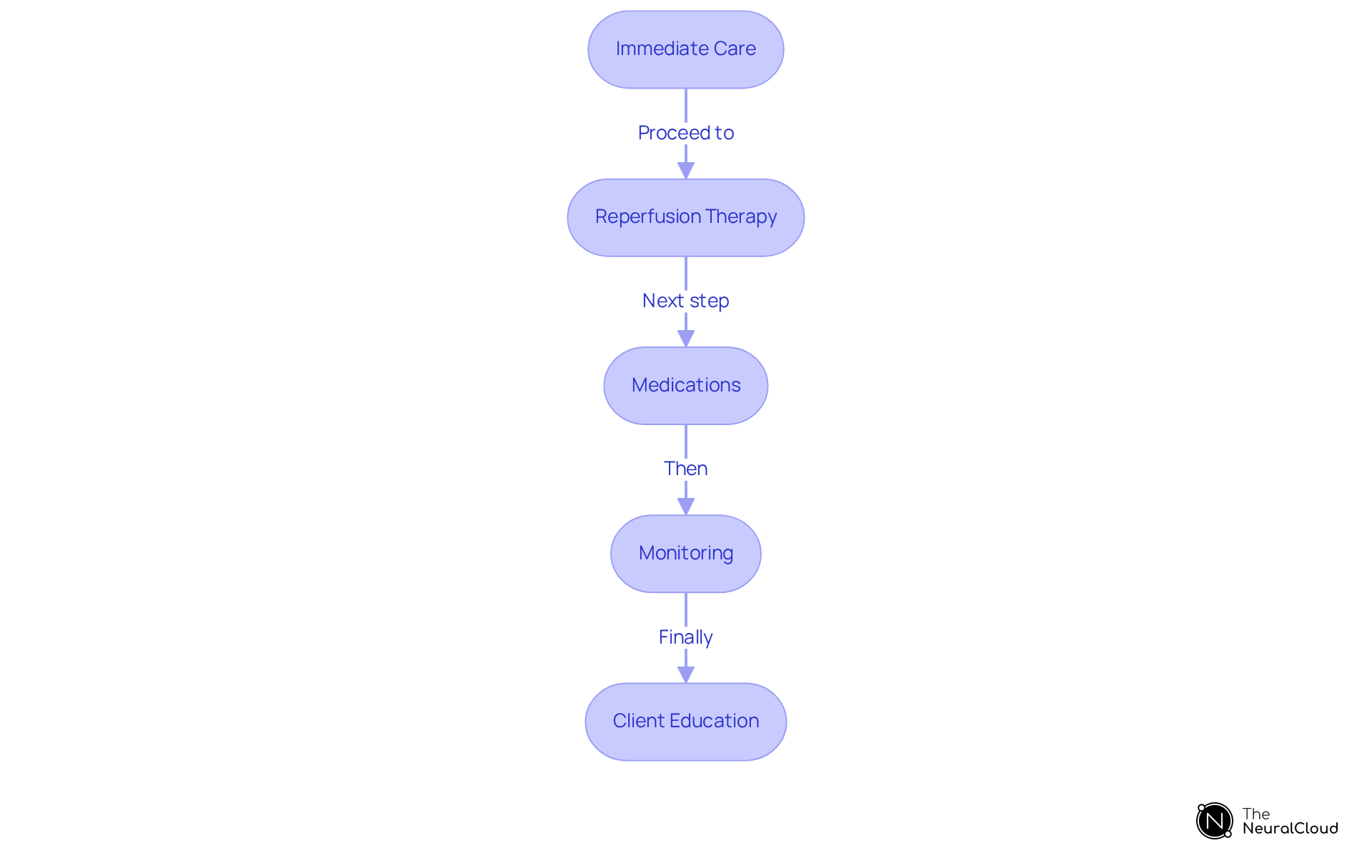
Manage Inferior Infarct: Treatment Protocols and Best Practices
Management of an inferior infarct involves several critical steps to optimize patient outcomes.
Immediate Care: Administer aspirin and nitroglycerin promptly to alleviate chest pain and enhance coronary blood flow. Aspirin is integral to antiplatelet therapy, significantly reducing vascular death after acute MI.
Reperfusion Therapy: Upon confirmation of STEMI, initiate reperfusion therapy without delay. Primary Percutaneous Coronary Intervention (PCI) is the preferred method if it can be performed within 90 minutes of the patient's arrival. This approach has been shown to reduce non-fatal reinfarction rates significantly compared to thrombolytic therapy. Thrombolytic Therapy should be considered if PCI is unavailable and the individual presents within 12 hours of symptom onset. Timely use of can enhance results, especially in individuals at high risk.
Medications: Initiate beta-blockers, ACE inhibitors, and statins as part of the long-term management strategy. These medications are essential for lowering mortality and preventing reinfarction, with beta-blockers showing considerable advantages in individuals with heart failure after MI. It is recommended to start beta-blockers within 24 hours post-MI.
Monitoring: Continuous ECG monitoring is vital to detect arrhythmias or complications early. Approximately 90% of individuals with acute MI develop some form of cardiac arrhythmias, making vigilant monitoring essential.
Client Education: Involve individuals in conversations regarding lifestyle adjustments, such as quitting smoking, altering diets, and enhancing physical activity. These changes are critical for secondary prevention and improving long-term cardiovascular health.
By applying these management strategies, healthcare providers can enhance patient care and significantly improve outcomes for those experiencing an inferior infarct.
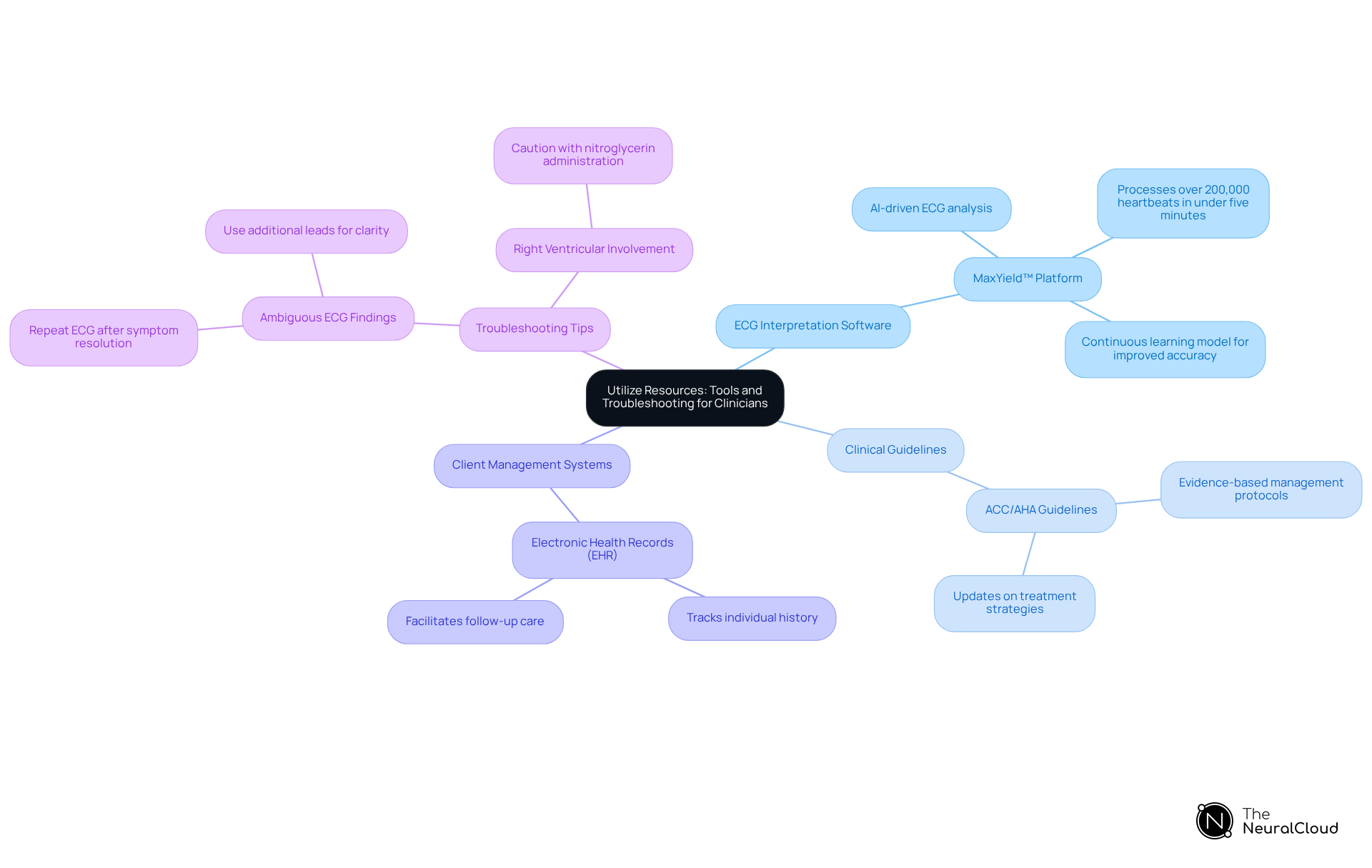
Utilize Resources: Tools and Troubleshooting for Clinicians
Clinicians can utilize a variety of resources and tools to aid in the diagnosis and management of inferior myocardial infarction:
-
ECG Interpretation Software: The MaxYield™ platform from Neural Cloud Solutions leverages AI-driven ECG analysis tools to significantly enhance diagnostic accuracy and efficiency. It automates the labeling of ECG waveforms and features a continuous learning model that evolves its algorithms over time, ensuring improved accuracy. MaxYield™ can process over 200,000 heartbeats in under five minutes, which is crucial for timely decision-making. Studies indicate that diagnostic accuracies of AI systems often range from 86.7% to 99.9%, reinforcing the effectiveness of such tools in clinical settings.
-
Clinical Guidelines: Refer to the latest ACC/AHA guidelines for comprehensive management protocols and updates on treatment strategies for myocardial infarction. These guidelines offer evidence-based suggestions that are crucial for effective healthcare.
-
Client Management Systems: Utilize electronic health records (EHR) to meticulously track individual history, treatment plans, and follow-up care. This ensures and facilitates better clinical outcomes.
-
Troubleshooting Tips:
- If ECG findings are ambiguous, consider repeating the ECG after symptom resolution or using additional leads to gain a clearer picture of the cardiac status. The MaxYield™ platform can assist in clarifying ECG findings when they are unclear, enhancing diagnostic confidence.
- In situations of right ventricular involvement, exercise caution with nitroglycerin administration to prevent hypotension, which can complicate management.
By leveraging these resources, clinicians can enhance their diagnostic capabilities and improve patient management outcomes.
Conclusion
Understanding and managing inferior infarcts is crucial for improving patient outcomes in cases of myocardial infarction. This article emphasizes the importance of recognizing key characteristics, diagnostic processes, and treatment protocols associated with inferior infarcts. By mastering these elements, healthcare professionals can ensure timely and effective interventions that significantly enhance patient care.
The discussion outlines essential steps in diagnosing inferior infarcts, from gathering medical history and conducting physical examinations to utilizing advanced ECG interpretation tools. It highlights the critical role of prompt reperfusion therapy and the administration of appropriate medications in managing these cases. Additionally, incorporating resources such as clinical guidelines and diagnostic software can further streamline the process, allowing clinicians to make informed decisions swiftly.
Ultimately, the significance of thorough knowledge and adherence to established protocols cannot be overstated. Clinicians are encouraged to stay updated with current guidelines and leverage available tools to enhance their diagnostic and management capabilities. By doing so, they can contribute to better health outcomes for individuals affected by inferior myocardial infarction, reinforcing the importance of prompt and effective care in cardiology.
Frequently Asked Questions
What is an inferior infarct?
An inferior infarct occurs due to a blockage in the right coronary artery (RCA), leading to reduced blood flow to the lower wall of the heart.
What are the common symptoms of an inferior infarct?
Common symptoms include chest pain, shortness of breath, and diaphoresis. Women may exhibit atypical symptoms such as abdominal pain or dizziness.
What are the key ECG findings associated with an inferior infarct?
The hallmark ECG findings include ST-segment elevation in leads II, III, and aVF, indicating lower wall involvement. Reciprocal changes, such as ST depression and T wave inversion in leads I and aVL, are also common.
What does ST-segment elevation in leads II, III, and aVF indicate?
ST-segment elevation in these leads indicates involvement of the lower wall of the heart during an inferior infarct.
What are the classifications of inferior infarcts?
Inferior infarcts can be classified as STEMI (ST-Elevation Myocardial Infarction) or NSTEMI (Non-ST-Elevation Myocardial Infarction) based on specific ECG findings.
What percentage of fatal acute myocardial infarction cases are attributed to atherosclerotic plaque occlusion?
Approximately 70% of fatal acute myocardial infarction cases are attributed to occlusion caused by atherosclerotic plaques.
Why is timely intervention important for patients with inferior infarcts?
Timely intervention is critical as individuals who undergo percutaneous coronary intervention (PCI) within 90 minutes of arrival have better outcomes.
How can the MaxYield™ platform assist in the diagnosis of inferior infarcts?
The MaxYield™ platform can enhance diagnostic yield by automating ECG analysis, allowing healthcare professionals to focus on critical decision-making.






