Overview
The article provides an overview of inferior infarction, a type of myocardial infarction that impacts the heart's lower wall, primarily resulting from blockage in the right coronary artery. It highlights the critical need for recognizing specific ECG changes and clinical symptoms, which are essential for accurate diagnosis. Furthermore, the article discusses advanced technologies, such as AI-driven ECG analysis and telemedicine, which significantly enhance diagnostic accuracy. These innovations not only improve patient outcomes but also streamline the management of this condition, making it crucial for healthcare professionals to stay informed about these developments.
Introduction
Understanding inferior infarction is crucial for healthcare professionals, as it constitutes a significant portion of myocardial infarctions that can result in critical health outcomes. This article explores the diagnostic criteria, management strategies, and the role of advanced technology in improving the identification and treatment of inferior infarction. Given the complexities of ECG interpretation and the urgency of timely intervention, it raises an important question: how can clinicians ensure they are equipped with the most effective tools and knowledge to address this life-threatening condition?
Understand Inferior Infarction: Definition and Importance
An inferior infarction is a type of myocardial event (MI) that primarily impacts the bottom wall of the heart, often resulting from the blockage of the right coronary artery (RCA). This condition reduces blood flow and oxygen supply to the myocardium, leading to ischemia and potential necrosis if not promptly addressed.
Recognizing inferior infarction is crucial, as it constitutes a significant portion of all myocardial infarctions (MIs) and may present with distinct clinical signs and specific ECG changes. For example, the Marquette 12SL ACS tool has shown a 25% relative improvement in detecting acute inferior infarction in women under 60, emphasizing the need for tailored diagnostic strategies.
Moreover, this tool has enhanced emergency physicians' interpretation of acute myocardial infarction by 50%, demonstrating its effectiveness in clinical environments. The implementation of gender-specific interpretation standards has also increased sensitivity for identifying acute anterior MI from 42% to 48%, resulting in a 50% reduction in false positive admissions for patients with chest pain and a 31% decrease in CCU admissions for non-AMI patients.
Understanding these factors is vital for , ultimately improving patient outcomes and optimizing resource allocation in cardiology departments. Additionally, the MaxYield™ platform by Neural Cloud Solutions automates and refines ECG analysis, addressing inefficiencies in traditional methods while providing healthcare professionals with precise cardiac insights.

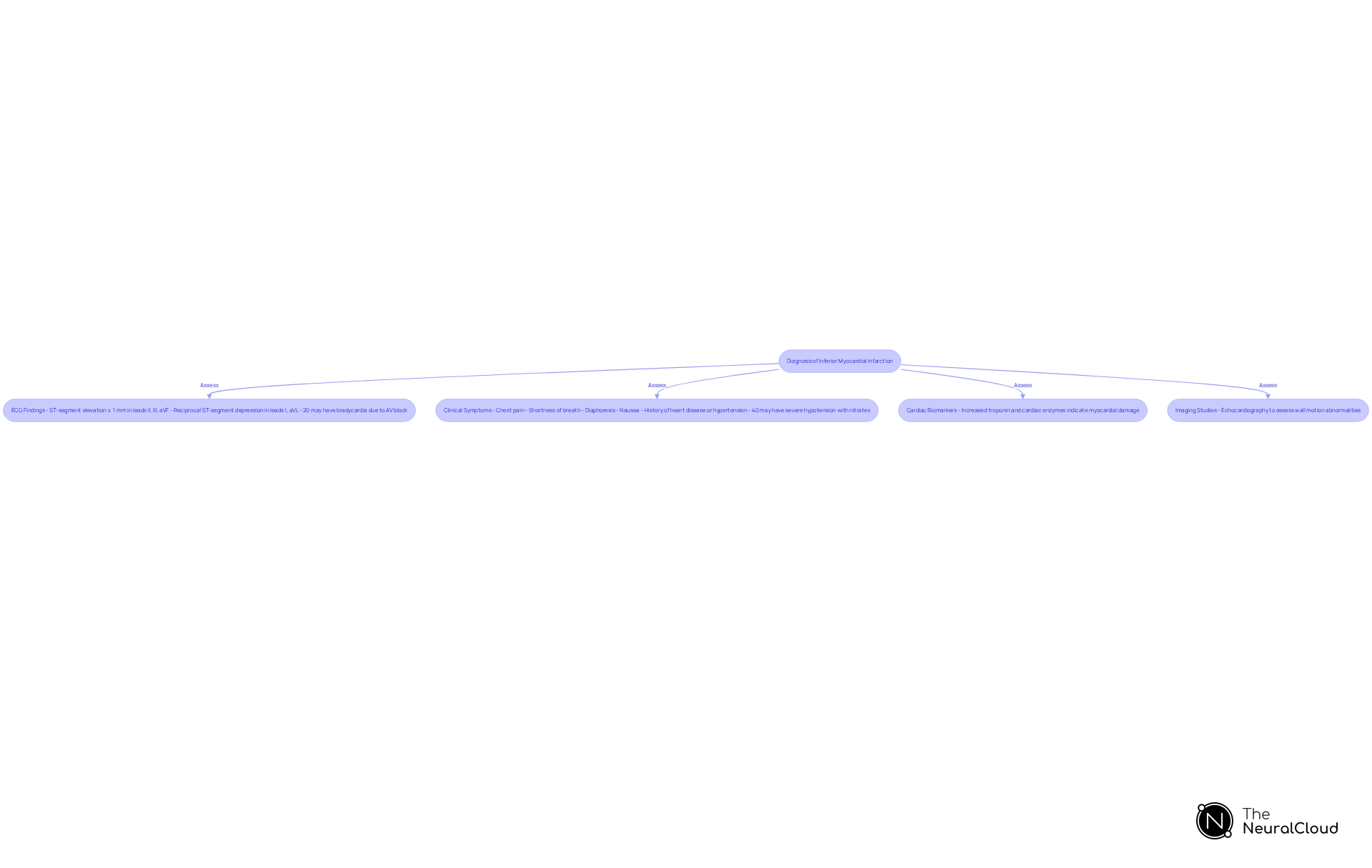
Identify Diagnostic Criteria for Inferior Infarction
To , healthcare providers should focus on specific ECG changes and clinical symptoms. Key diagnostic criteria include:
- ECG Findings: Look for ST-segment elevation of at least 1 mm in leads II, III, and aVF, indicating inferior wall involvement. Reciprocal ST-segment depression may also be observed in lateral leads (I and aVL). Furthermore, it is crucial to recognize that 20% of individuals may encounter significant bradycardia due to second or third-degree AV block, complicating the clinical picture.
- Clinical Symptoms: Patients may present with chest pain, shortness of breath, diaphoresis, and nausea. Evaluating the individual's history and risk factors, such as previous heart disease or hypertension, is important. Additionally, 40% of patients with simultaneous right ventricular damage may experience severe hypotension in response to nitrates, highlighting the need for careful monitoring during diagnosis and management.
- Cardiac Biomarkers: Increased concentrations of troponin and other cardiac enzymes can assist in diagnosing myocardial damage, offering crucial information regarding heart injury.
- Imaging Studies: Echocardiography may be utilized to assess wall motion abnormalities and confirm the diagnosis.
The MaxYield™ platform enhances ECG analysis by automating the labeling of ECG waveforms, allowing for more efficient identification of key features during the diagnostic process. By systematically assessing these criteria, clinicians can accurately identify suboptimal tissue damage and initiate suitable management strategies. The continuous learning model of the MaxYield™ platform enhances algorithm accuracy and efficiency over time, further supporting healthcare professionals in their diagnostic efforts.
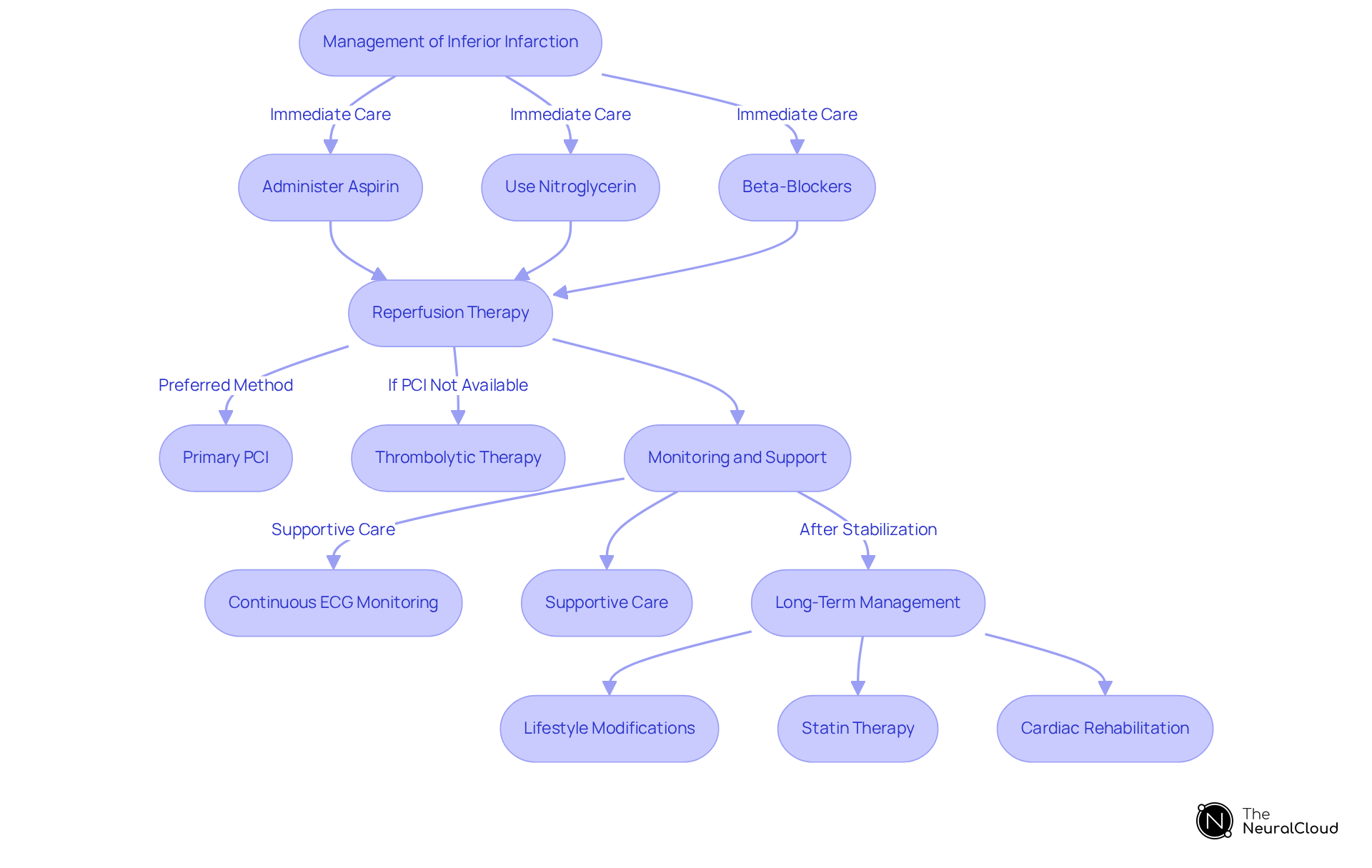
Implement Management Strategies for Inferior Infarction
Management of inferior infarction involves a combination of pharmacological and procedural interventions.
Immediate care includes administering aspirin and other antiplatelet agents to prevent further clot formation. Nitroglycerin may be used to relieve chest pain, while beta-blockers can help reduce myocardial oxygen demand.
Reperfusion therapy is crucial; primary percutaneous coronary intervention (PCI) is the preferred method for restoring blood flow in individuals presenting within 12 hours of symptom onset. If PCI is not available, thrombolytic therapy may be considered, provided there are no contraindications.
Monitoring and support are essential, with continuous ECG monitoring to detect any arrhythmias or complications. Supportive care, including oxygen therapy and fluid management, should be provided as needed.
Long-term management should follow stabilization, where individuals are evaluated for secondary prevention strategies. These may include lifestyle modifications, statin therapy, and .
By implementing these management techniques, healthcare workers can effectively address inferior infarction and improve patient outcomes.
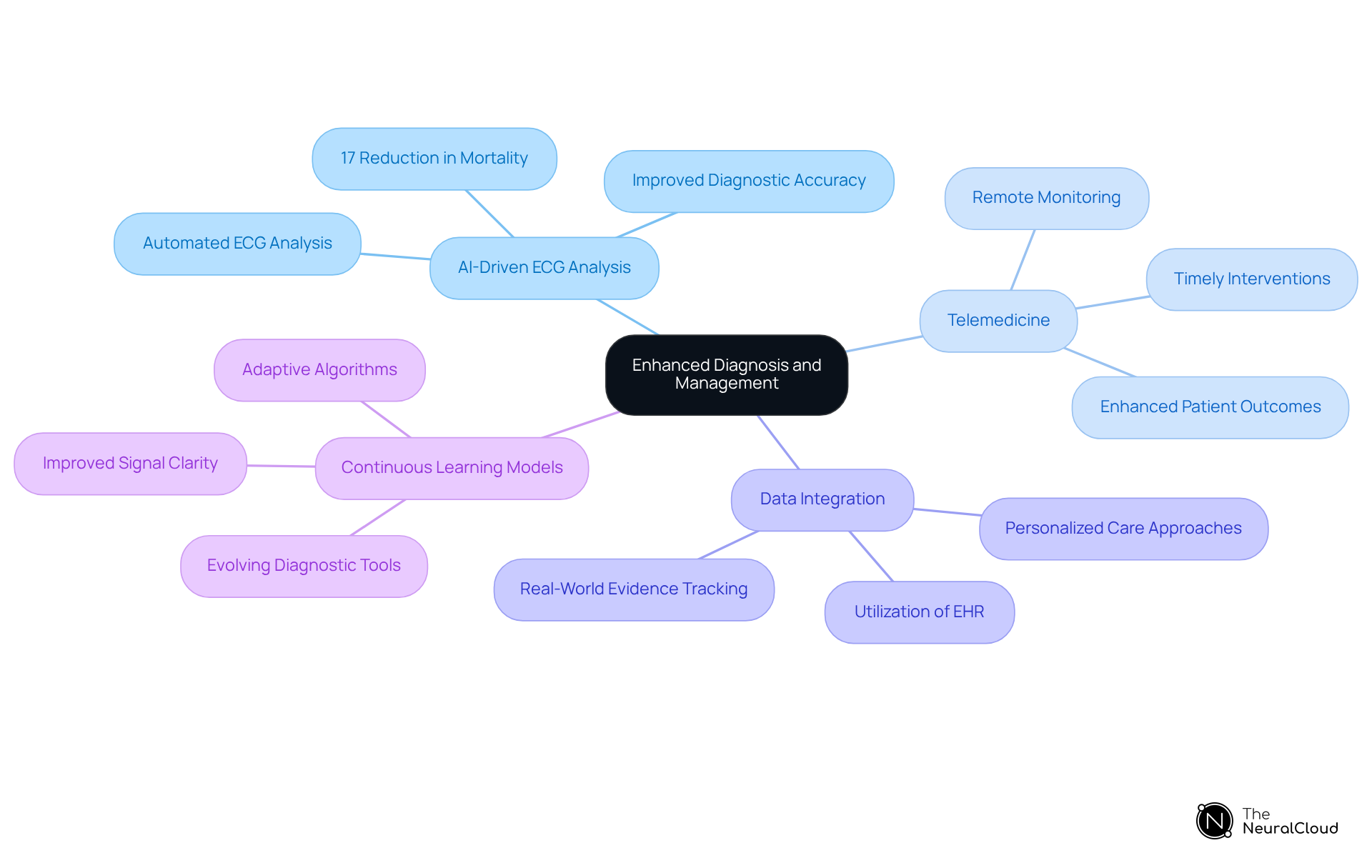
Utilize Advanced Technology for Enhanced Diagnosis and Management
Integrating advanced technology into the diagnosis and management of substandard myocardial damage can greatly improve accuracy and efficiency. The challenges in ECG analysis often stem from manual interpretation, which can be time-consuming and prone to errors. To address these challenges, leveraging technology is essential. Here are effective strategies to enhance diagnostic capabilities:
- AI-Driven ECG Analysis: Platforms like Neural Cloud Solutions' MaxYield™ automate ECG data evaluation, quickly detecting vital characteristics associated with lower heart attacks. This automation reduces the time clinicians spend on manual interpretation while enhancing diagnostic accuracy. Research shows that AI-generated ECG alerts can result in a 17% decrease in all-cause mortality, particularly significant for individuals experiencing lower myocardial damage.
- Telemedicine: The introduction of telehealth solutions enables remote monitoring and consultations, allowing for timely interventions for individuals at risk of inferior infarction. This method has demonstrated effectiveness in managing myocardial infarction, as it allows healthcare providers to respond quickly to alterations in individual conditions. According to healthcare experts, telemedicine has significantly enhanced outcomes for individuals by ensuring prompt care delivery.
- Data Integration: Utilizing electronic health records (EHR) alongside helps track patient outcomes and refine management strategies based on real-world evidence. This integration supports a more personalized approach to care, improving overall treatment efficacy.
- Continuous Learning Models: Employing systems that learn from each case enhances the algorithms used in ECG analysis, ensuring that diagnostic tools evolve with new clinical insights. This adaptability is crucial for maintaining high standards of care in a rapidly changing medical landscape, particularly in addressing challenges such as noise and signal artifacts that can obscure true ECG signals.
By embracing these technological advancements, healthcare professionals can significantly enhance their diagnostic capabilities and improve the management of inferior infarction.
Conclusion
Understanding and managing inferior infarction is essential for enhancing patient outcomes in cardiovascular health. This type of myocardial infarction, which primarily impacts the heart's lower wall, necessitates prompt diagnosis and intervention to avert severe complications. By utilizing tailored diagnostic strategies and advanced technologies, healthcare professionals can significantly improve their capacity to recognize and effectively treat this condition.
The article underscores critical diagnostic criteria, including:
- Specific ECG changes
- Clinical symptoms
- The significance of cardiac biomarkers
Furthermore, it emphasizes the necessity of immediate and long-term management strategies, such as:
- Pharmacological interventions
- Lifestyle modifications
The incorporation of advanced technologies, including AI-driven ECG analysis and telemedicine, further empowers clinicians to provide timely and accurate care.
Ultimately, mastering the diagnosis and management of inferior infarction transcends merely addressing a medical condition; it is fundamentally about saving lives and optimizing healthcare resources. By remaining informed about current practices and adopting innovative solutions, healthcare providers can substantially improve their approach to inferior infarction, resulting in better patient outcomes and a healthier society.
Frequently Asked Questions
What is an inferior infarction?
An inferior infarction is a type of myocardial infarction (MI) that primarily affects the bottom wall of the heart, often caused by the blockage of the right coronary artery (RCA), leading to reduced blood flow and oxygen supply to the myocardium.
Why is recognizing inferior infarction important?
Recognizing inferior infarction is crucial because it represents a significant portion of all myocardial infarctions and may present with distinct clinical signs and specific ECG changes, which are essential for timely intervention.
How does the Marquette 12SL ACS tool assist in detecting inferior infarction?
The Marquette 12SL ACS tool has shown a 25% relative improvement in detecting acute inferior infarction in women under 60, highlighting the importance of tailored diagnostic strategies.
What impact has the Marquette 12SL ACS tool had on emergency physicians?
This tool has improved emergency physicians' interpretation of acute myocardial infarction by 50%, enhancing diagnostic accuracy in clinical environments.
How have gender-specific interpretation standards affected the diagnosis of acute anterior MI?
The implementation of gender-specific interpretation standards has increased sensitivity for identifying acute anterior MI from 42% to 48%, resulting in a 50% reduction in false positive admissions for patients with chest pain.
What are the benefits of understanding inferior infarction for patient outcomes?
Understanding inferior infarction is vital for timely intervention, which ultimately improves patient outcomes and optimizes resource allocation in cardiology departments.
What is the MaxYield™ platform and its role in ECG analysis?
The MaxYield™ platform by Neural Cloud Solutions automates and refines ECG analysis, addressing inefficiencies in traditional methods while providing healthcare professionals with precise cardiac insights.






