Overview
This article provides an overview of the diagnosis, management, and clinical implications of Left Bundle Branch Block (LBBB) in cardiac health. LBBB is clinically significant due to its association with serious cardiac conditions, making accurate diagnosis crucial. Key diagnostic criteria are outlined to assist healthcare professionals in identifying LBBB effectively. Treatment options, including Cardiac Resynchronization Therapy (CRT), are discussed, highlighting their role in improving patient outcomes. Furthermore, the article emphasizes the importance of advanced technologies, such as artificial intelligence (AI), in enhancing diagnostic accuracy and overall patient care.
Introduction
Left Bundle Branch Block (LBBB) is more than a technical term in cardiology; it signifies a critical disruption in the heart's electrical conduction system, which can lead to serious health implications. Understanding LBBB is essential for healthcare professionals, as it frequently indicates underlying cardiac conditions and complicates the diagnosis of acute myocardial infarction. This article examines the complexities of LBBB, outlining its:
- Diagnostic criteria
- Management strategies
- Latest advancements in treatment options
Clinicians must effectively navigate the challenges posed by LBBB to enhance patient outcomes and ensure timely interventions.
Define Left Bundle Branch Block (LBBB) and Its Clinical Importance
Left Bundle Branch Block (LBBB) is a cardiac conduction condition that manifests as a delay or obstruction in the electrical signals traveling through the left bundle branch of the heart's conduction system. This disruption leads to asynchronous ventricular contraction, which can result in various clinical issues, including heart failure and an increased risk of arrhythmias. The clinical significance of LBBB is considerable, as it often signals underlying cardiac diseases such as coronary artery disease or cardiomyopathy. Notably, the LBBB ECG can complicate the identification of acute myocardial infarction, necessitating that clinicians consider its impact on management and prognosis.
Research indicates that individuals with LBBB, particularly those with a QRS duration of 150 milliseconds or greater, face worse outcomes in cardiac failure scenarios. These patients are at a heightened risk of cardiac failure and mortality, underscoring the importance of timely diagnosis and intervention. Cardiac resynchronization therapy (CRT) has been shown to improve hemodynamics and ventricular systolic function in patients with LBBB, especially those with reduced ejection fraction. For instance, studies have demonstrated significant improvements in cardiac function and overall well-being following left bundle branch pacing (LBBP) in patients suffering from heart failure associated with LBBB.
Additionally, LBBB can lead to substantial left ventricular dyssynchrony, a critical factor in the development of acute heart failure. The presence of LBBB complicates the clinical picture, as it may obscure signs of myocardial infarction and indicate underlying cardiac pathology. Therefore, understanding the clinical implications of LBBB is essential for healthcare professionals, as it directly influences patient management strategies and outcomes.

Diagnose LBBB: Key ECG Criteria and Methodologies
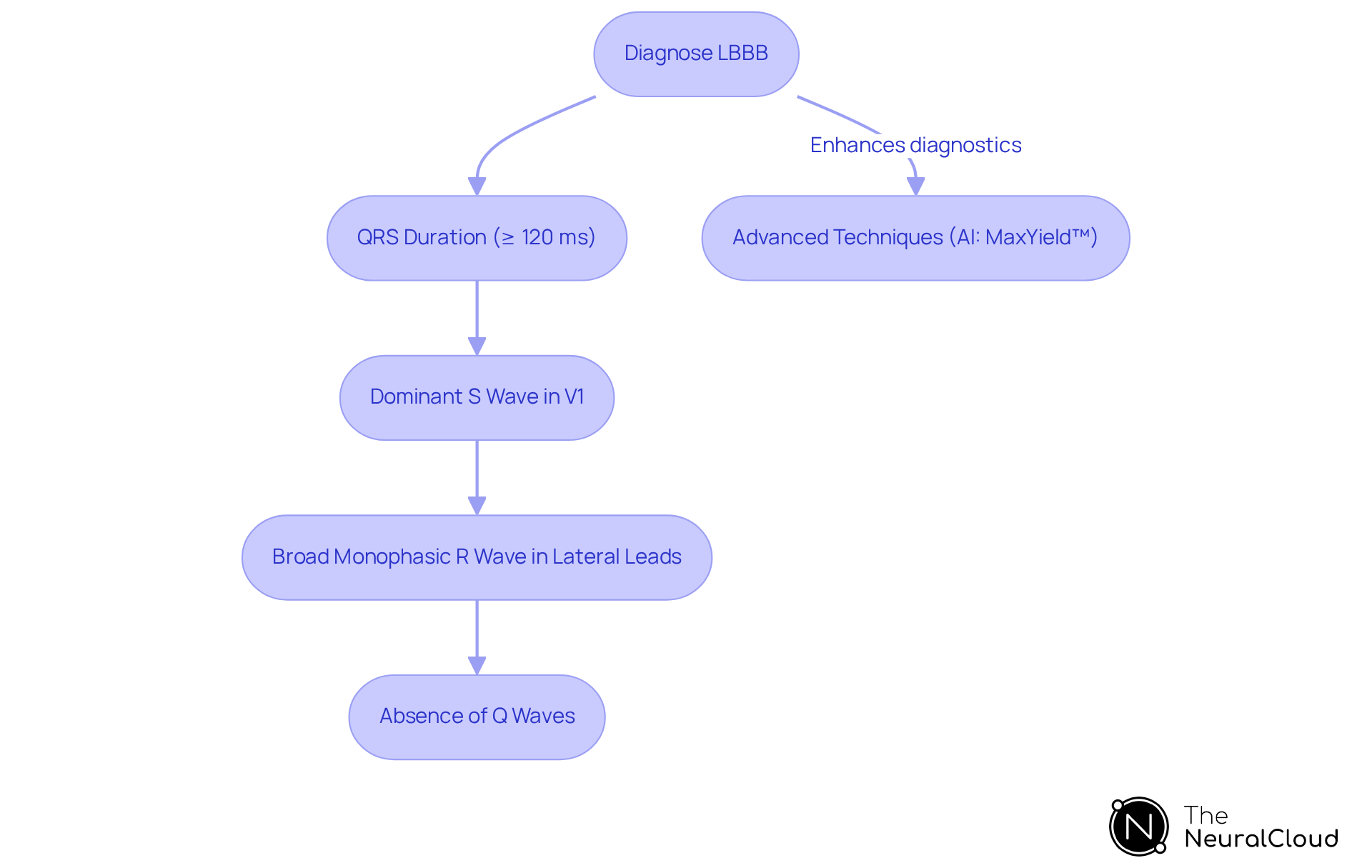
Diagnosing Left Bundle Branch Block (LBBB) necessitates adherence to specific ECG criteria, which include:
- QRS Duration: A QRS duration of 120 milliseconds or greater is essential for diagnosing complete LBBB. Studies indicate that a QRS duration (QRSd) ≥ 120 ms is associated with increased risks for all-cause and cardiovascular deaths.
- Dominant S Wave in V1: The presence of a dominant S wave in lead V1 is a characteristic of left bundle branch block.
- Broad Monophasic R Wave in Lateral Leads: Typically, a broad monophasic R wave is observed in leads I, aVL, V5, and V6.
- Absence of Q Waves: There should be no Q waves present in the lateral leads.
These criteria are vital for distinguishing left bundle branch block from other conditions, such as right bundle branch block and left ventricular hypertrophy.
The incorporation of advanced techniques, particularly AI algorithms like MaxYield™, significantly enhances the precision of LBBB ECG detection. MaxYield™ utilizes advanced noise filtering and distinct wave recognition to analyze complex ECG patterns, minimizing the potential for human error and improving diagnostic accuracy. This technology can swiftly isolate ECG waves from recordings affected by baseline wander, movement, and muscle artifact, while also recovering previously obscured sections of lengthy Holter and patch monitor recordings. Research has demonstrated that AI models can achieve a positive predictive accuracy of 80% and a negative predictive accuracy of 90.4% in recognizing underlying cardiovascular conditions, including LBBB ECG.
Clinicians must consider the individual's clinical history and symptoms when interpreting ECG results, ensuring a comprehensive assessment that transcends the ECG findings alone. It is important to note that left bundle branch block always signifies pathology, yet it is common in older individuals; incidental discoveries of left bundle branch block on ECG in asymptomatic elderly individuals do not necessitate immediate concern. This holistic approach, augmented by technologies like MaxYield™, is essential for effective diagnosis and management of cardiac conditions.
Manage LBBB: Treatment Options and Clinical Considerations
Management of Left Bundle Branch Block (LBBB) primarily focuses on addressing underlying cardiac conditions and improving patient symptoms through a multifaceted approach:
-
Cardiac Resynchronization Therapy (CRT): CRT is often indicated for patients with symptomatic heart failure and LBBB, particularly those with a QRS duration of 150 ms or more. This therapy restores synchrony in ventricular contractions, significantly improving cardiac output and reducing symptoms. Recent studies suggest that CRT can reduce the rate of mortality or hospitalization due to heart failure to 22.2% compared to 30.8% for biventricular pacing, highlighting its effectiveness in improving outcomes for individuals.
-
Pacemaker Therapy: In situations where LBBB ECG leads to significant bradycardia or other conduction abnormalities, the implantation of a pacemaker may be necessary to regulate rhythm. The average acute success rate for left bundle branch area pacing (LBBAP) has been reported at 91.3%, demonstrating its feasibility and safety in clinical practice.
-
Medications: Management of associated conditions such as hypertension or heart failure may involve the use of beta-blockers, ACE inhibitors, or diuretics, which can help stabilize the individual's condition and improve overall heart function. It is important to note that approximately 20-40% of individuals may fail to respond to CRT, particularly in cases involving LBBB ECG, highlighting the challenges in treatment efficacy.
-
Lifestyle Modifications: Motivating individuals to embrace heart-healthy lifestyle adjustments, such as a balanced diet and consistent exercise, is essential in managing left bundle branch block and improving overall cardiovascular health.
Clinicians should regularly observe individuals with left bundle branch block for any changes in symptoms or cardiac function, adjusting treatment strategies as necessary to optimize outcomes. The integration of advanced technologies, such as the MaxYield™ platform from Neural Cloud Solutions, facilitates ongoing monitoring and analysis of LBBB ECG data, which enhances the management of patients with LBBB and ensures timely interventions. MaxYield™ enables rapid labeling of ECG waveforms and automates data processing, allowing healthcare professionals to analyze more data in less time and improve diagnostic clarity. Additionally, the platform's neural network models for complex signal processing can help identify key features in ECG data, supporting the discovery of new digital biomarkers that enhance treatment strategies. As Dr. Vijayaraman noted, "Conduction-system pacing, especially the left bundle branch area pacing, has been shown to be a safe, physiologic, and effective alternative to biventricular pacing.

Conclusion
Left Bundle Branch Block (LBBB) represents a significant cardiac condition that requires careful consideration due to its implications for heart function and patient management. This article emphasizes the necessity of recognizing LBBB not merely as a standalone diagnosis, but also as a potential indicator of underlying cardiac issues that can considerably impact patient outcomes. It is vital to comprehend LBBB's effect on ventricular contraction and its association with severe conditions such as heart failure and arrhythmias for effective clinical practice.
The discussion outlines essential diagnostic criteria for LBBB on ECG, including QRS duration and specific wave patterns. These factors are crucial for accurate identification and differentiation from other cardiac conditions. Furthermore, the integration of advanced technologies, such as AI-driven tools, enhances diagnostic accuracy, facilitating more timely and effective management strategies. Treatment options, particularly cardiac resynchronization therapy and lifestyle modifications, are integral to improving patient prognosis and quality of life.
In summary, managing LBBB necessitates a comprehensive approach that combines precise diagnosis, targeted treatment, and continuous monitoring. Clinicians are encouraged to utilize innovative technologies and adhere to established guidelines to optimize care for patients with LBBB. By adopting these strategies, healthcare professionals can significantly enhance outcomes and improve the overall management of this complex condition, ultimately leading to better health for affected individuals.
Frequently Asked Questions
What is Left Bundle Branch Block (LBBB)?
Left Bundle Branch Block (LBBB) is a cardiac conduction condition characterized by a delay or obstruction in the electrical signals traveling through the left bundle branch of the heart's conduction system, leading to asynchronous ventricular contraction.
Why is LBBB clinically significant?
LBBB is clinically significant because it often indicates underlying cardiac diseases such as coronary artery disease or cardiomyopathy and can complicate the identification of acute myocardial infarction.
What are the potential clinical issues associated with LBBB?
Potential clinical issues associated with LBBB include heart failure, an increased risk of arrhythmias, and worse outcomes in cardiac failure scenarios, particularly in patients with a QRS duration of 150 milliseconds or greater.
How does LBBB affect patient outcomes?
Patients with LBBB, especially those with a longer QRS duration, face a heightened risk of cardiac failure and mortality, emphasizing the need for timely diagnosis and intervention.
What treatment options are available for patients with LBBB?
Cardiac resynchronization therapy (CRT) can improve hemodynamics and ventricular systolic function in patients with LBBB, particularly those with reduced ejection fraction. Left bundle branch pacing (LBBP) has also shown significant improvements in cardiac function and overall well-being in heart failure patients associated with LBBB.
How does LBBB contribute to left ventricular dyssynchrony?
LBBB can lead to substantial left ventricular dyssynchrony, which is a critical factor in the development of acute heart failure.
What challenges does LBBB present in clinical diagnosis?
The presence of LBBB can obscure signs of myocardial infarction and complicate the clinical picture, making it essential for healthcare professionals to understand its implications for patient management and outcomes.






