Overview
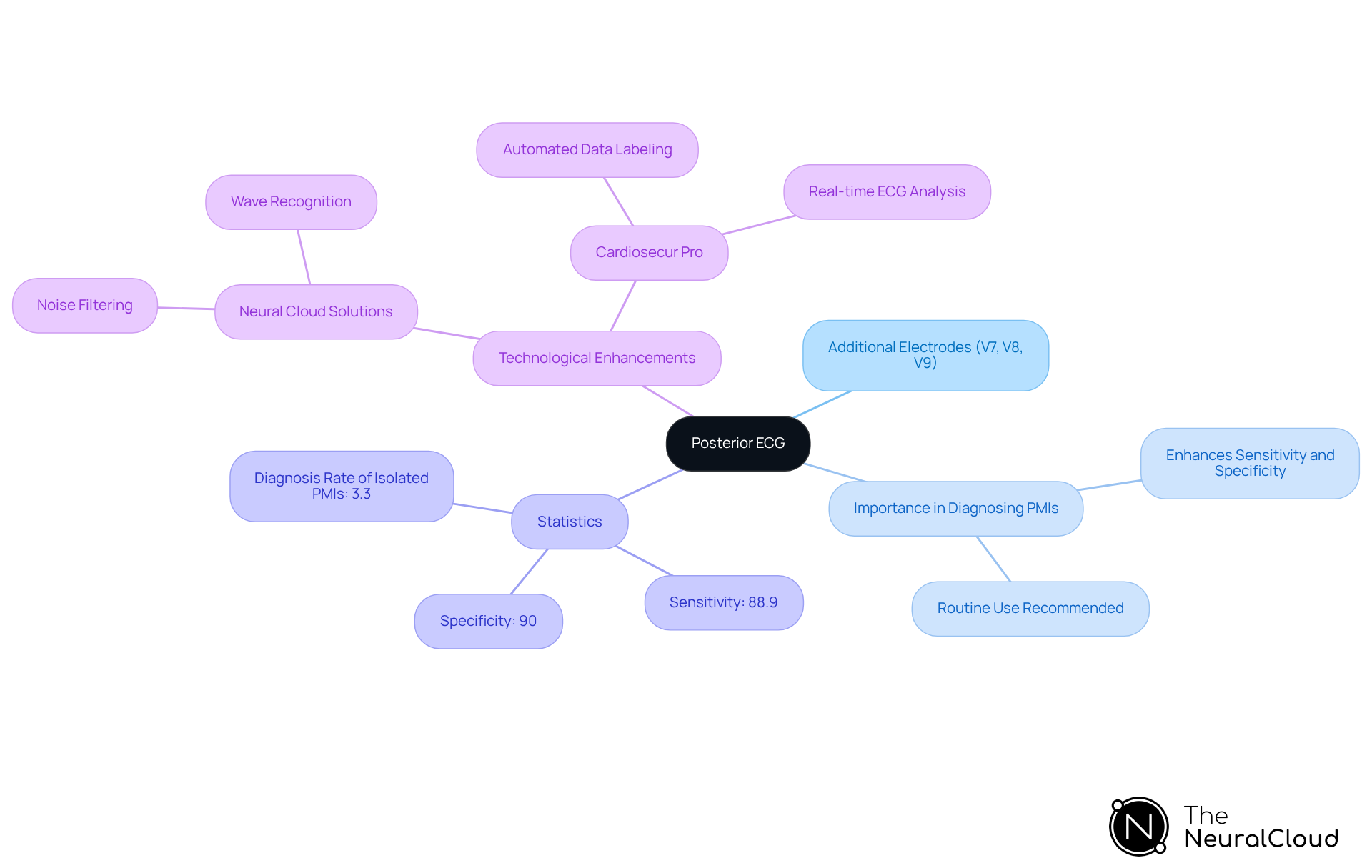
The article provides an overview of the techniques and AI insights related to posterior ECG, underscoring its critical role in accurately diagnosing myocardial infarctions that standard ECGs may overlook.
It details how the addition of extra electrodes improves diagnostic sensitivity and specificity, enhancing the overall effectiveness of ECG analysis.
Furthermore, the integration of advanced AI technologies facilitates streamlined ECG interpretation, which ultimately leads to better patient outcomes and informed clinical decision-making.
By addressing these innovations, the article highlights the importance of evolving diagnostic methods in contemporary healthcare.
Introduction
The landscape of electrocardiography is evolving, particularly with the emergence of posterior ECG techniques that aim to improve diagnostic accuracy in cardiac care. This innovative approach incorporates additional electrodes on the patient's back, effectively addressing the critical limitation of standard ECGs, which often overlook signs of posterior myocardial infarctions.
As developers seek to integrate these advanced techniques into their applications, the challenge lies in the effective utilization of AI-driven tools to streamline analysis and enhance patient outcomes.
The fusion of innovative ECG methods and cutting-edge technology has the potential to significantly redefine cardiac diagnostics.
Define Posterior ECG: Key Concepts and Importance
A posterior ECG is a specialized electrocardiogram that employs additional electrodes (V7, V8, and V9) positioned on the patient's back to identify irregularities in the heart's rear wall. This technique is critical, as standard 12-lead ECGs frequently overlook posterior ECG signs of myocardial infarctions (PMIs), which can result in delayed diagnosis and treatment.
By incorporating rear electrodes, the posterior ECG significantly enhances the sensitivity and specificity of evaluations, allowing for more accurate detection of cardiac events. Research indicates that using rear leads can elevate the diagnosis rate of isolated posterior myocardial infarction to approximately 3.3% among acute myocardial infarction patients when assessed with posterior ECG. Furthermore, the sensitivity for diagnosing acute myocardial infarction using posterior ECG has been reported at 88.9%, with a specificity of 90%.
Understanding these fundamental aspects of posterior ECG is crucial for developers seeking to integrate this methodology into their applications, ensuring the delivery of that meet clinical requirements. Regular application of posterior ECG leads is recommended for patients suspected of experiencing acute myocardial infarction, as timely thrombolytic treatment can significantly reduce mortality rates.
Advanced technologies such as Neural Cloud Solutions, which excel in noise filtering and wave recognition, can enhance the analysis of posterior ECGs. MaxYield™ automates the labeling of critical data, enabling developers to convert noisy recordings into clear insights, thereby facilitating confident clinical decision-making.
As noted by N Salehi, 'Given the high sensitivity and specificity of utilizing rear electrodes, we recommend the routine application of posterior ECG in individuals suspected of experiencing acute MI, as thrombolytic treatment for such individuals will decrease the mortality rate.
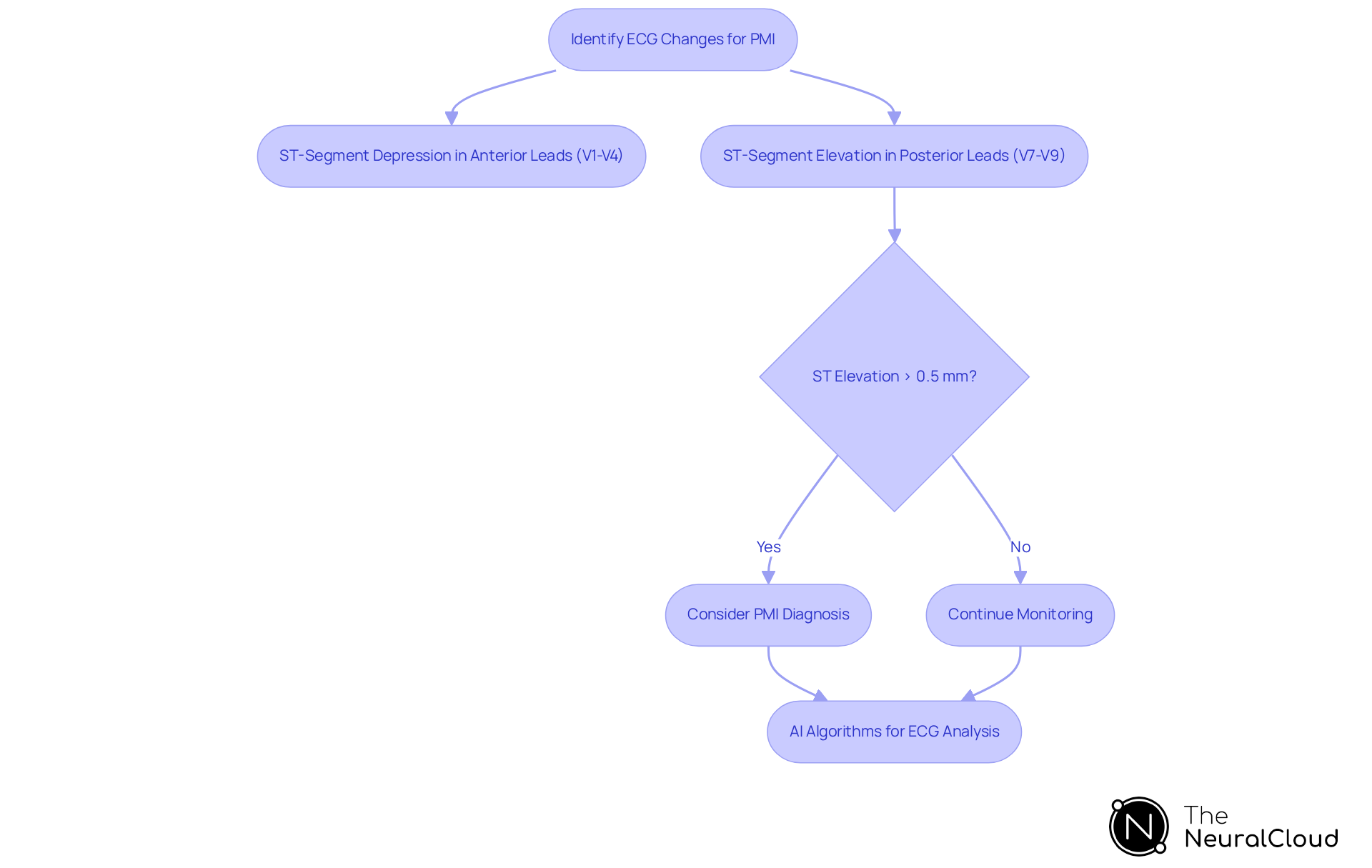
Identify ECG Changes in Posterior Myocardial Infarction
In the context of subsequent myocardial infarction (PMI), the electrocardiogram (ECG) typically displays ST-segment depression in the anterior leads (V1-V4), accompanied by prominent R waves in these channels. Notably, ST-segment elevation in the posterior ECG leads (V7-V9) serves as a crucial diagnostic indicator for PMI, with established criteria requiring ST elevation (STE) of at least 0.5 mm in any posterior lead. Clinicians must remain vigilant for these subtle ECG changes, as they are often overlooked. Recent research suggests that as many as 6% of posterior myocardial infarctions may go undetected even with the 0.5 mm ST elevation threshold, emphasizing the necessity for increased awareness in posterior ECG interpretation. Additionally, significant ST depression (greater than 2 mm) has been documented in leads V2-V3 during PMI, which complicates the diagnostic process.
For developers of AI algorithms focused on ECG interpretation, the precise detection of these patterns is vital, as it can significantly impact clinical decision-making. The 'Neural Cloud Solutions' platform enhances this process by automating ECG analysis, adeptly filtering ECG signals through noise and isolating key features in each heartbeat, including P-wave, QRS complex, and T-wave onsets and offsets. By employing advanced AI-driven techniques, MaxYield™ continuously refines its algorithms to boost accuracy and efficiency over time, ensuring that subtle yet critical ECG changes are not overlooked.
This innovative approach not only addresses the challenges faced in ECG analysis but also provides healthcare professionals with a powerful tool to . The features of the MaxYield™ platform, such as automated signal processing and enhanced pattern recognition, translate into significant advantages for clinicians, enabling them to make informed decisions based on comprehensive and reliable data.
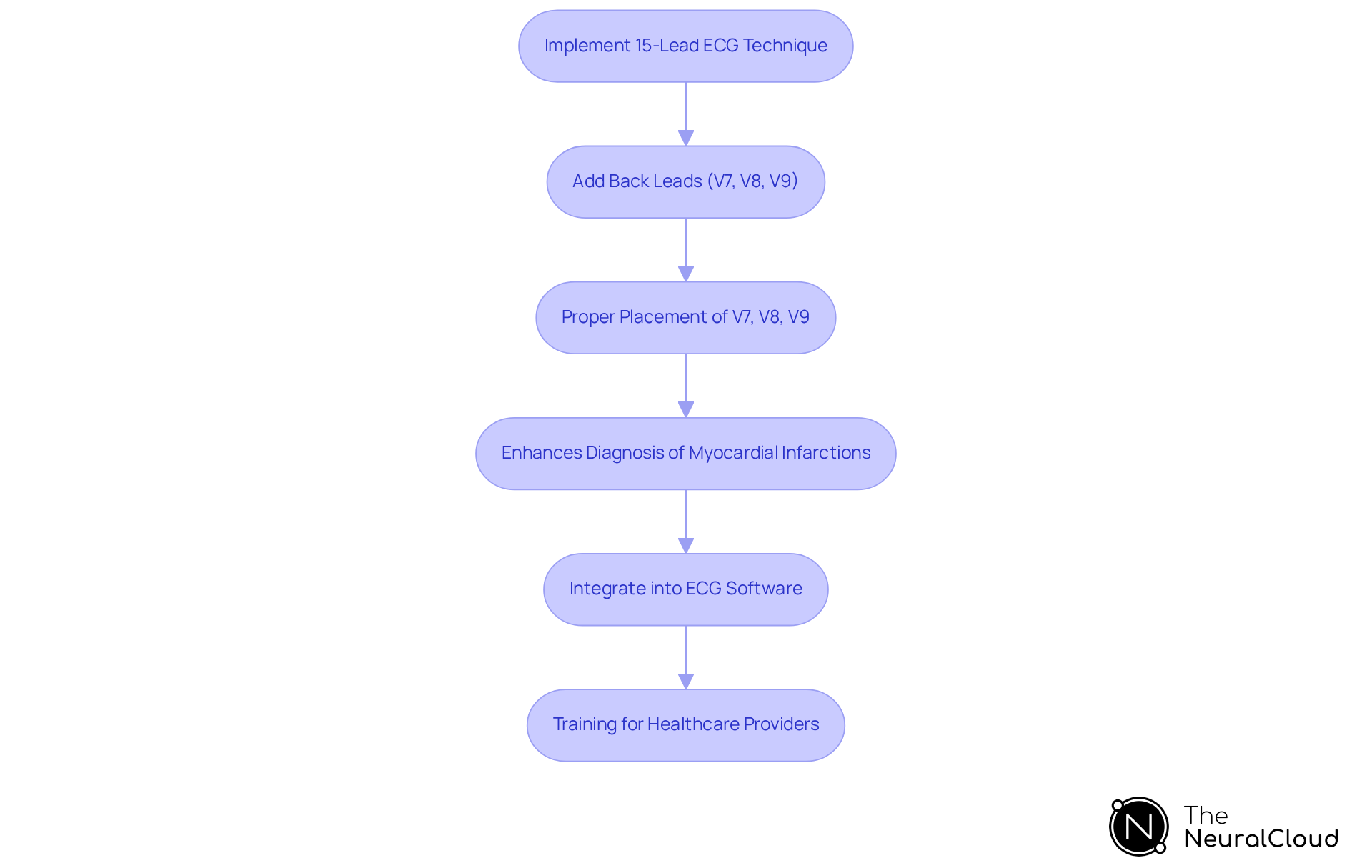
Implement 15-Lead ECG Technique for Enhanced Diagnosis
To implement the 15-lead ECG technique, clinicians add three back leads (V7, V8, and V9) to the standard 12-lead setup, creating a posterior ECG. This expanded configuration significantly improves visualization of the heart's rear wall, which is often compromised during myocardial infarctions, as shown by the posterior ECG. Proper placement is essential:
- V7 should be located at the left back axillary line
- V8 at the left scapula
- V9 at the left paraspinal area
This method not only enhances the detection of rear myocardial infarctions but also increases the overall diagnostic precision of posterior ECG readings.
Research indicates that the inclusion of these electrodes can enhance sensitivity for identifying ST-segment elevation in acute myocardial infarction instances. The 15-electrode ECG has demonstrated a significant improvement in diagnostic precision, with 15.1% of patients requiring posterior ECG leads for STEMI diagnosis. This underscores the . Ioannis Vogiatzis noted that the use of the posterior ECG contributes to a faster and more accurate diagnosis of STEMI, which facilitates prompt reperfusion therapy.
Developers should consider integrating this technique into their ECG analysis software, such as Neural Cloud Solutions' product. This software automates ECG analysis and enhances cardiac insights through advanced noise reduction and signal mapping. The system maps ECG signals through noise, isolating and labeling key features in every heartbeat, delivering beat-by-beat analysis and transforming noisy recordings into detailed insights. This integration provides clinicians with a more robust diagnostic tool that enhances patient outcomes.
However, it is essential to recognize that additional training for healthcare providers is necessary before the routine use of the 15-lead ECG can be implemented effectively. Furthermore, challenges faced by paramedics in recording the additional leads should be addressed to ensure successful application in emergency settings.
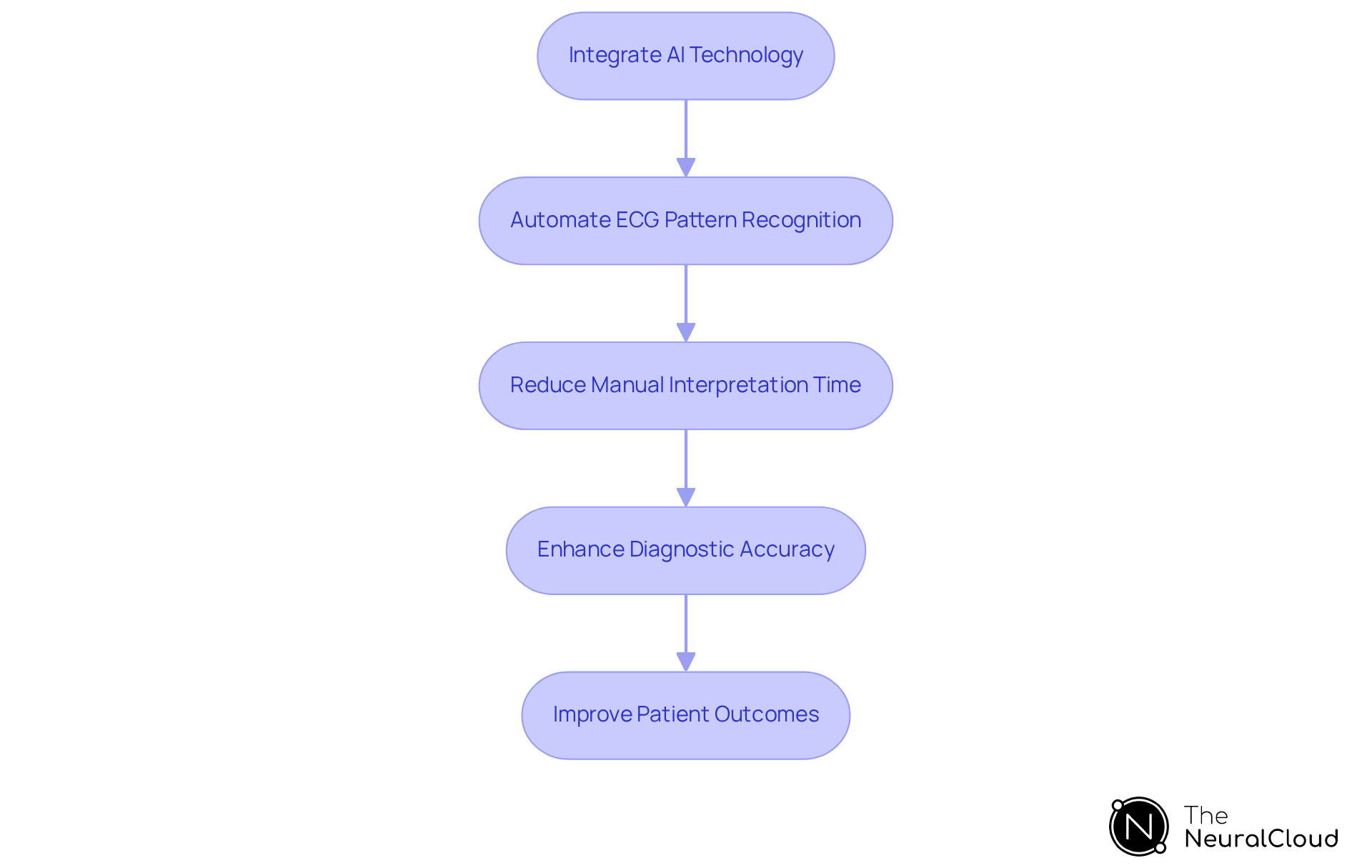
Leverage AI Technology for Improved ECG Analysis and Workflow
Integrating AI technology into ECG analysis addresses significant challenges, streamlining workflows and enhancing diagnostic accuracy. Advanced AI algorithms, such as those offered by Neural Cloud Solutions, automatically identify and categorize ECG patterns. This automation reduces the time clinicians spend on manual interpretation, allowing them to focus on patient care. The system effectively maps ECG signals through noise, isolating and labeling key features in every heartbeat, which facilitates quicker identification of critical conditions like posterior ECG issues.
The MaxYield™ platform provides beat-by-beat analysis, processing 200,000 heartbeats in under 5 minutes. This rapid analysis empowers healthcare professionals to make informed decisions swiftly. Developers are encouraged to prioritize the creation of AI-driven tools that not only analyze ECG data but also deliver actionable insights. The implementation of MaxYield™ in ECG interpretation has demonstrated improved workflow efficiency, transforming lengthy and noisy ECG recordings into clean, crisp signals.
By leveraging this advanced AI technology, the potential for improved patient outcomes increases significantly. Timely interventions can be based on , which is crucial in critical care settings. As Robert D. Stevens from Johns Hopkins Medicine noted, "The ECG contains a lot of really interesting information not just about the heart but about the cardiovascular system," underscoring the transformative potential of AI in this field. The integration of such technology marks a pivotal advancement in cardiac care, ultimately benefiting both healthcare providers and patients.
Conclusion
The exploration of posterior ECG techniques alongside the integration of AI insights highlights significant advancements in cardiac diagnostics. By employing additional electrodes on the back, healthcare providers enhance their capacity to detect posterior myocardial infarctions, which are frequently overlooked by traditional ECG methods. This specialized approach not only boosts diagnostic accuracy but also enables timely interventions that can save lives.
Key insights from the article emphasize the value of the 15-lead ECG technique, which expands the standard setup to incorporate posterior leads, ultimately providing a more comprehensive view of cardiac health. Furthermore, the impact of AI in streamlining ECG analysis is substantial; advanced algorithms improve the detection of subtle ECG changes, facilitating quicker and more reliable clinical decisions. The combination of these techniques and technologies represents a significant advancement in the battle against cardiovascular diseases.
As the field of cardiology evolves, embracing these innovations is vital for enhancing patient outcomes. Developers are encouraged to prioritize the integration of these advanced techniques and AI tools within their applications, ensuring healthcare professionals are equipped with optimal resources for accurate diagnoses. By doing so, the healthcare community can greatly influence the management of acute myocardial infarctions, leading to improved patient care and reduced mortality rates.
Frequently Asked Questions
What is a posterior ECG?
A posterior ECG is a specialized electrocardiogram that uses additional electrodes (V7, V8, and V9) placed on the patient's back to detect irregularities in the heart's rear wall.
Why is a posterior ECG important?
It is important because standard 12-lead ECGs often miss signs of posterior myocardial infarctions (PMIs), which can lead to delayed diagnosis and treatment.
How does a posterior ECG improve diagnosis?
By incorporating rear electrodes, the posterior ECG enhances the sensitivity and specificity of evaluations, allowing for more accurate detection of cardiac events.
What are the diagnostic rates associated with posterior ECG?
Research shows that the diagnosis rate of isolated posterior myocardial infarction can reach approximately 3.3% among acute myocardial infarction patients when assessed with posterior ECG. The sensitivity for diagnosing acute myocardial infarction is reported at 88.9%, with a specificity of 90%.
When should posterior ECG leads be applied?
Posterior ECG leads are recommended for patients suspected of experiencing acute myocardial infarction, as timely thrombolytic treatment can significantly reduce mortality rates.
What technologies can enhance posterior ECG analysis?
Advanced technologies like Neural Cloud Solutions can improve the analysis of posterior ECGs by excelling in noise filtering and wave recognition.
How does MaxYield™ assist in posterior ECG analysis?
MaxYield™ automates the labeling of critical data, helping developers convert noisy recordings into clear insights, which facilitates confident clinical decision-making.
What is the recommendation from N Salehi regarding posterior ECG?
N Salehi recommends the routine application of posterior ECG in individuals suspected of experiencing acute myocardial infarction, as it can decrease mortality rates through timely thrombolytic treatment.






