Overview
This article provides an overview of the diagnosis, management, and technological advancements associated with posterior STEMI, a type of heart attack that results from blood flow obstruction to the heart's back wall. It underscores the necessity of recognizing atypical symptoms and utilizing advanced diagnostic tools, such as additional ECG leads and AI-driven analysis. Furthermore, it discusses the implementation of timely reperfusion therapy, which is crucial for enhancing patient outcomes. The article highlights the pivotal role of technology in advancing clinical practices.
Introduction
Understanding the nuances of posterior ST-segment elevation myocardial infarction (STEMI) is critical for healthcare professionals. Its atypical symptoms and subtle ECG changes can easily be overlooked, leading to misdiagnosis. This article delves into the essential characteristics, diagnostic techniques, and management strategies vital for effective intervention in cases of posterior STEMI. Furthermore, with the rise of advanced technologies and AI-driven tools, we must consider how these innovations can reshape the landscape of diagnosis and treatment for this often-misunderstood condition.
Define Posterior STEMI: Key Characteristics and Clinical Importance
Rear ST-segment elevation myocardial infarction occurs when blood flow to the back wall of the heart is hindered, usually due to blockage of the left circumflex artery or a branch of the right coronary artery. Key characteristics include:
- ECG Changes: The presence of ST-segment elevation in posterior leads (V7-V9) is diagnostic. In anterior leads, ST-segment depression and tall R-waves may be observed, indicating underlying ischemia. The integration of wearable technology with Neural Cloud Solutions' MaxYield™ platform enhances the efficiency of ECG analysis, allowing for automated labeling that reduces the time spent on noise filtering and annotating, thus improving diagnostic accuracy.
- Clinical Presentation: Symptoms can be atypical, often manifesting as vague discomfort rather than classic chest pain. For instance, a case study highlighted a 48-year-old male who presented with isolated left arm numbness and weakness, mimicking an acute stroke. This underscores the importance of recognizing non-traditional symptoms and maintaining a in the emergency department. The MaxYield™ platform aids in addressing challenges such as physiological variability and signal artifacts, ensuring a consistently clean signal for better clinical decision-making.
- Incidence: The posterior stemi accounts for approximately 15-20% of all STEMIs, with an isolated incidence of about 3.3%. It often co-occurs with inferior or lateral myocardial infarctions, complicating the diagnosis of posterior stemi.
Identifying these traits is crucial for prompt intervention, as late diagnosis can result in greater myocardial damage and worse outcomes for individuals. For example, an individual with a troponin level that rose from 12.6 ng/L to 8518 ng/L within four hours illustrates the critical nature of prompt diagnosis and treatment. Emergency doctors must uphold a strong level of suspicion for back myocardial infarction, particularly in situations showing unusual symptoms, to guarantee effective management and enhance patient outcomes.

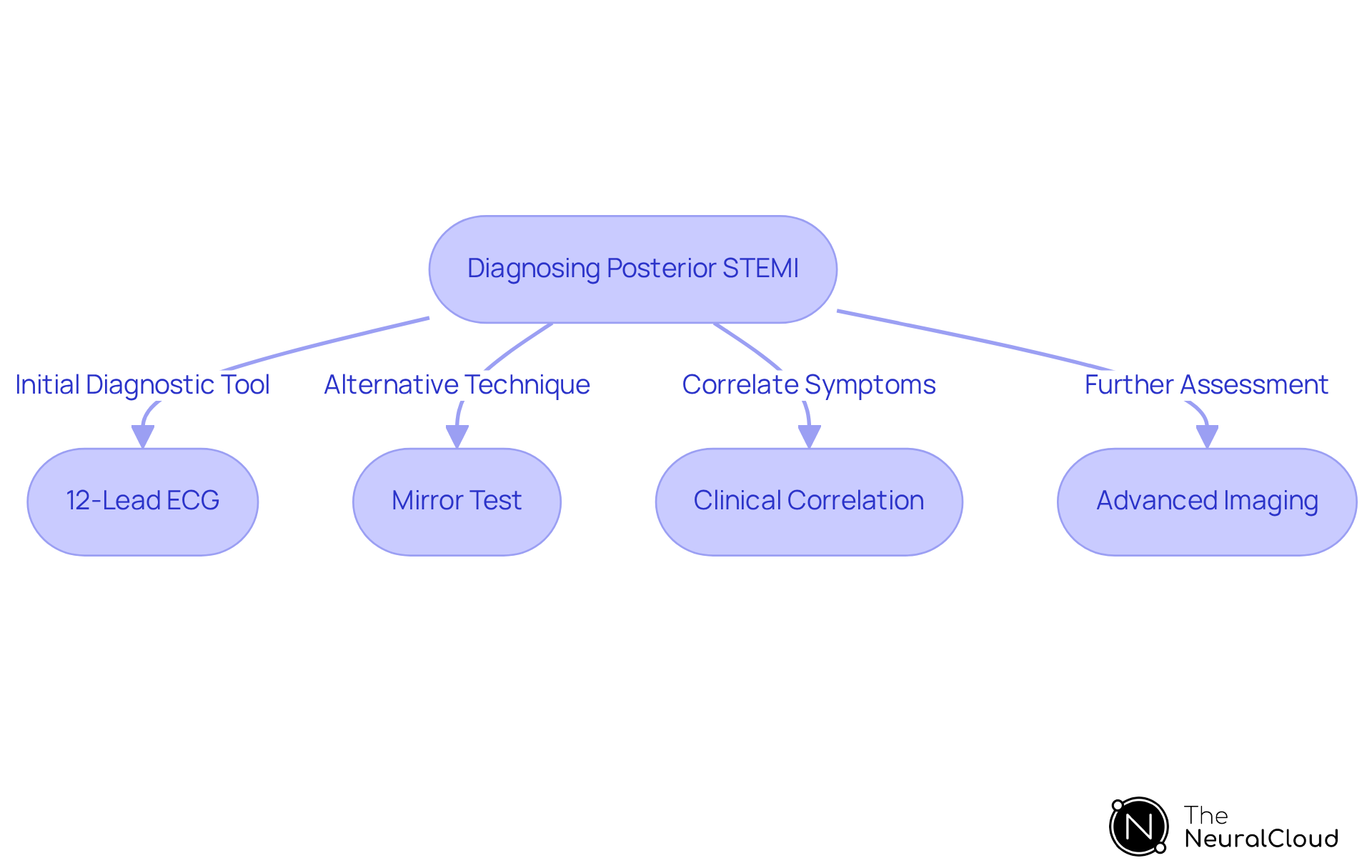
Diagnose Posterior STEMI: Essential Techniques and Tools
Diagnosing posterior stemi requires a multifaceted approach that utilizes several key techniques and tools.
- 12-Lead ECG: A standard 12-lead ECG is typically the initial diagnostic tool; however, it may not always detect posterior changes. To effectively capture the signs of posterior stemi, should be placed on the back, as conventional leads may miss critical signs of ischemia. This approach enhances the accuracy of the diagnosis, ensuring that no vital information is overlooked.
- Mirror Test: This innovative technique involves flipping the ECG to evaluate anterior leads for indirect indicators of ischemia, such as ST-segment depression. By using this technique, underlying problems that a standard 12-lead ECG might miss can be uncovered, particularly in cases of posterior stemi myocardial infarction. This method provides a valuable alternative for assessing potential issues that may not be immediately apparent.
- Clinical Correlation: Correlating ECG findings with clinical symptoms is crucial. A high level of suspicion is particularly important in individuals presenting with unusual symptoms such as nausea or epigastric pain, which can frequently accompany posterior stemi. This correlation ensures that the diagnostic process is thorough and considers all relevant factors.
- Advanced Imaging: When ECG findings are inconclusive, advanced imaging techniques such as echocardiography or cardiac MRI can be employed to assess myocardial perfusion and identify wall motion abnormalities. These imaging techniques provide further insights that can verify or exclude a posterior stemi, significantly enhancing diagnostic accuracy.
Employing these diagnostic instruments efficiently can lead to the early detection and management of posterior stemi, greatly improving outcomes for individuals. For instance, studies suggest that prompt ECG evaluations within 10 minutes of individual presentation are essential for enhancing treatment pathways and reducing myocardial damage.
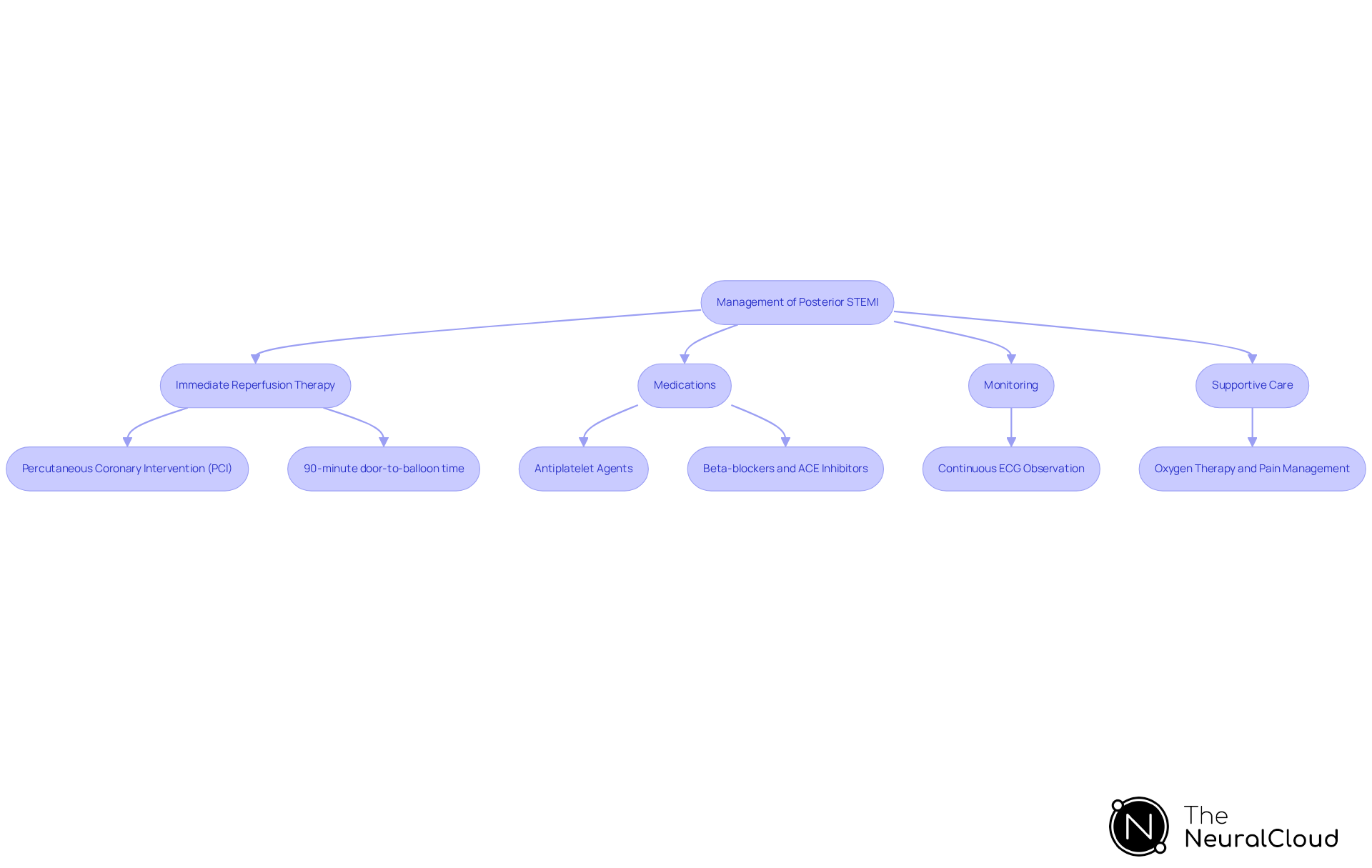
Manage Posterior STEMI: Treatment Protocols and Interventions
Management of posterior stemi adheres to established protocols designed to optimize patient outcomes.
- Immediate Reperfusion Therapy: The cornerstone of treatment for a posterior stemi is reperfusion therapy, ideally achieved through percutaneous coronary intervention (PCI). Timely initiation is crucial to restore blood flow and minimize myocardial damage, with a of 90 minutes or less being essential for effective outcomes.
- Medications: Administering antiplatelet agents, such as aspirin and clopidogrel, alongside anticoagulants, is essential to prevent further clot formation. Additionally, beta-blockers and ACE inhibitors may be indicated to enhance heart function and alleviate workload on the myocardium. As emphasized by Helen Jahn, the updated guidelines prefer the use of ACE inhibitors or ARBs in individuals with reduced ejection fraction, diabetes, or hypertension.
- Monitoring: Continuous ECG observation is essential for identifying arrhythmias or any significant changes in the individual's condition, allowing for prompt intervention if required. The guidelines emphasize the application of electrocardiography (ECG) as the foundation for the early identification of posterior stemi. Leveraging advanced AI technology, such as Neural Cloud Solutions' MaxYield™, can enhance this monitoring process by transforming lengthy and noisy ECG recordings into clean, crisp signals, thereby improving the accuracy and reliability of arrhythmia detection. This not only aids in timely interventions but also contributes to operational cost reductions by streamlining the monitoring process.
- Supportive Care: Providing oxygen therapy, effective pain management, and fluid resuscitation as needed is critical. Ensuring the individual is stable before transferring to a higher level of care is also a key component of comprehensive management. The integration of automated ECG labeling and data extraction through MaxYield™ can streamline these processes, reducing operational costs and allowing healthcare professionals to focus on critical decision-making tasks, ultimately enhancing productivity.
Following these protocols can greatly increase the chances of positive results for patients facing back myocardial infarction, particularly with developments in pharmacology and the significance of dual antiplatelet therapy, along with cutting-edge technologies that improve ECG analysis effectiveness.
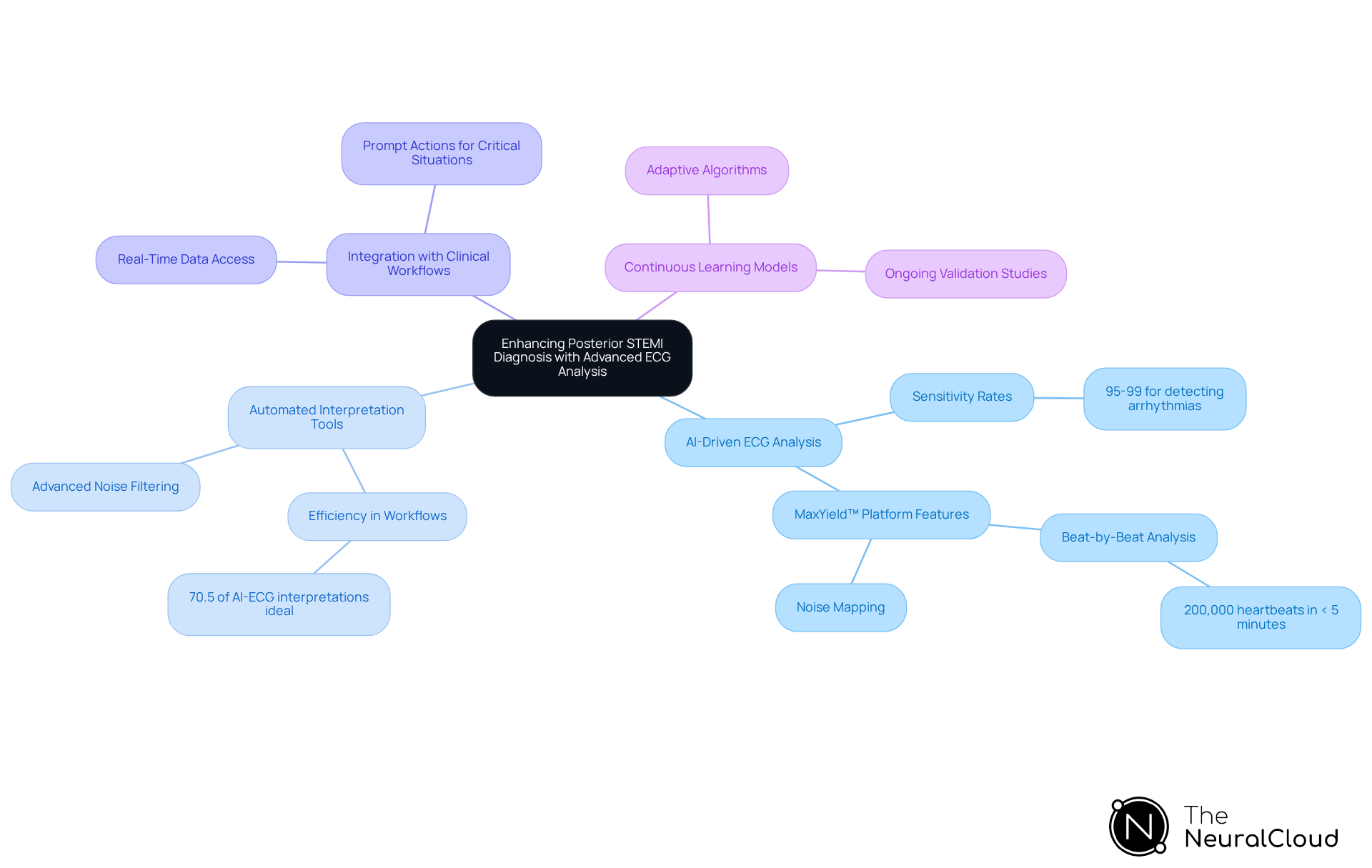
Leverage Technology: Enhancing Posterior STEMI Diagnosis with Advanced ECG Analysis
Leveraging technology in the diagnosis of posterior STEMI can significantly enhance clinical outcomes:
- AI-Driven ECG Analysis: The application of AI algorithms improves the detection of subtle ECG changes associated with posterior STEMI, thereby reducing the likelihood of missed diagnoses. Studies indicate that AI-ECG algorithms can achieve sensitivity rates of 95-99% for detecting arrhythmias, surpassing traditional methods that typically range from 70-80% accuracy. Neural Cloud Solutions' MaxYield™ platform exemplifies this advancement by mapping ECG signals through noise, isolating key features in every heartbeat, and delivering beat-by-beat analysis of 200,000 heartbeats in less than 5 minutes. This includes detailed outputs such as P-wave, QRS complex, and T-wave onsets and offsets.
- Automated Interpretation Tools: Platforms like MaxYield™ automate the labeling of ECG waveforms, allowing clinicians to concentrate on critical decision-making rather than time-consuming manual analysis. This automation streamlines workflows and enhances diagnostic precision, as evidenced by the ability of AI tools to identify patterns that may be overlooked by human interpreters. Notably, 1058 (70.5%) of AI-ECG interpreted ECGs were considered ideal and did not require edits, demonstrating the effectiveness of these automated tools in clinical settings. MaxYield™'s advanced noise filtering and wave recognition capabilities further support this efficiency.
- Integration with Clinical Workflows: Advanced ECG analysis tools can be seamlessly integrated into existing clinical workflows, ensuring healthcare providers have access to accurate data in real-time. This integration enables , which are essential in handling situations such as a specific type of heart attack, where every minute is vital. The integration of MaxYield™ into clinical platforms allows for rapid highlighting of potentially meaningful ECG data, enhancing early detection and timely intervention.
- Continuous Learning Models: AI systems that evolve with new data enhance diagnostic accuracy over time, adapting to emerging patterns in individual presentations. Continuous modifications and validation studies are essential to maintain the relevance and safety of AI algorithms in clinical settings. MaxYield™ embodies this principle through its adaptive algorithms that improve diagnostic yield and accuracy.
By embracing these technological advancements, healthcare professionals can significantly improve their diagnostic capabilities and ultimately enhance patient care specifically in cases of posterior STEMI.
Conclusion
Recognizing and managing posterior STEMI is vital for improving patient outcomes in cases of myocardial infarction. This condition, often characterized by atypical symptoms and subtle ECG changes, requires a high level of clinical suspicion and a comprehensive diagnostic approach. The integration of advanced technology, such as AI-driven ECG analysis, plays a crucial role in enhancing diagnostic accuracy and streamlining workflows, ultimately leading to timely interventions.
The article highlights essential diagnostic techniques, including:
- The use of additional leads
- Innovative methods like the mirror test, which can uncover critical signs of ischemia that standard approaches might miss.
Moreover, the management of posterior STEMI emphasizes the importance of:
- Immediate reperfusion therapy
- The administration of appropriate medications to prevent further complications
- Continuous monitoring and supportive care as key components of effective treatment protocols.
In conclusion, the significance of prompt diagnosis and management of posterior STEMI cannot be overstated. As advancements in technology continue to evolve, healthcare professionals must leverage these tools to enhance their diagnostic capabilities and improve patient care. By staying informed about the latest techniques and integrating innovative solutions like Neural Cloud Solutions' MaxYield™ platform, clinicians can ensure that they are well-equipped to address the challenges posed by posterior STEMI, ultimately saving lives and reducing myocardial damage.
Frequently Asked Questions
What is posterior STEMI?
Posterior ST-segment elevation myocardial infarction (STEMI) occurs when blood flow to the back wall of the heart is hindered, typically due to blockage of the left circumflex artery or a branch of the right coronary artery.
What are the key ECG changes associated with posterior STEMI?
The diagnostic ECG changes for posterior STEMI include ST-segment elevation in posterior leads (V7-V9), along with potential ST-segment depression and tall R-waves in anterior leads, indicating underlying ischemia.
How does the MaxYield™ platform enhance ECG analysis?
The MaxYield™ platform integrates wearable technology to improve the efficiency of ECG analysis by automating labeling, which reduces the time spent on noise filtering and annotating, thereby enhancing diagnostic accuracy.
What are the common clinical presentations of posterior STEMI?
Symptoms can be atypical, often presenting as vague discomfort instead of classic chest pain. For example, an individual may experience isolated left arm numbness and weakness, which can mimic an acute stroke.
What is the incidence of posterior STEMI?
Posterior STEMI accounts for approximately 15-20% of all STEMIs, with an isolated incidence of about 3.3%. It often occurs alongside inferior or lateral myocardial infarctions, complicating the diagnosis.
Why is it important to identify posterior STEMI traits promptly?
Identifying the traits of posterior STEMI is crucial for prompt intervention, as late diagnosis can lead to greater myocardial damage and worse patient outcomes. For instance, a significant rise in troponin levels within a short time underscores the need for urgent diagnosis and treatment.
What should emergency doctors consider when diagnosing posterior STEMI?
Emergency doctors must maintain a high level of suspicion for posterior myocardial infarction, especially in cases with unusual symptoms, to ensure effective management and improve patient outcomes.






