Overview
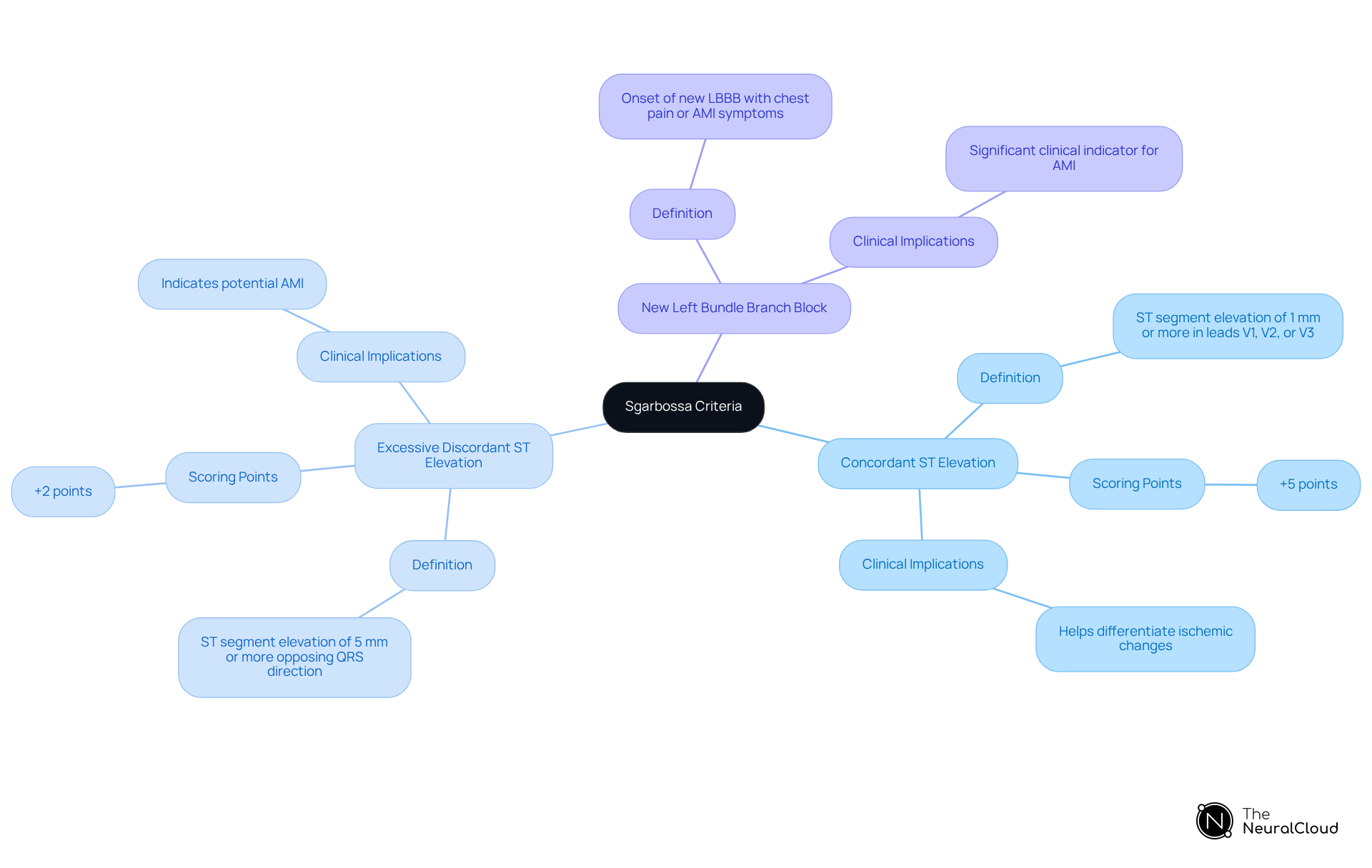
The Sgarbossa criteria are vital for the accurate diagnosis of acute myocardial infarction (AMI) in patients with left bundle branch block (LBBB). These criteria encompass three essential components:
- Concordant ST elevation
- Excessive discordant ST elevation
- New LBBB
Understanding and applying these criteria significantly enhance diagnostic accuracy. They assist in distinguishing true ischemic changes from those induced by LBBB. Ultimately, this improved differentiation can lead to better patient outcomes.
Introduction
Mastering the Sgarbossa criteria is essential for clinicians who navigate the complexities of ECG interpretation, especially when diagnosing acute myocardial infarction (AMI) in the presence of left bundle branch block (LBBB). This guide explores the critical components of the Sgarbossa criteria, providing insights that can significantly enhance diagnostic accuracy and improve patient outcomes. However, healthcare professionals may face challenges in effectively implementing these criteria, including inter-observer variability and the risk of misinterpretation. Clinicians must consider strategies to overcome these obstacles, ensuring precise and timely diagnoses.
Understand the Sgarbossa Criteria
The Sgarbossa criteria are essential ECG indicators that help clinicians diagnose acute myocardial infarction (AMI) in patients with left bundle branch obstruction. These criteria encompass three pivotal components that are crucial for accurate assessment.
- Concordant ST Elevation is characterized by ST segment elevation of 1 mm or more in leads V1, V2, or V3, aligning with the direction of the QRS complex, and is assigned +5 points in scoring.
- Excessive Discordant ST Elevation denotes ST segment elevation of 5 mm or more that opposes the direction of the QRS complex, contributing +2 points to the overall score.
- New Left Bundle Branch Block refers to the onset of a new left bundle branch block occurring alongside chest pain or other AMI-related symptoms, marking a significant clinical indicator.
Understanding these components is vital for , particularly when applying the Sgarbossa criteria, as they help differentiate genuine ischemic changes from those potentially misattributed to LBBB. Recent studies reveal that a score of ≥ 3 based on the Sgarbossa criteria demonstrates a sensitivity of 36% and specificity of 96% in the validation sample, while the derivation sample showed a sensitivity of 78% and specificity of 90%. This underscores their clinical relevance. Moreover, the revised Sgarbossa criteria have been validated for clinical use, addressing the limitations of the original standards, particularly concerning excessive discordance.
It is crucial to acknowledge challenges in implementing these criteria, such as inter-observer variability, which necessitates extensive training for accurate application. Familiarizing yourself with the Sgarbossa criteria enhances your ability to apply them effectively in real-world clinical scenarios, ultimately leading to improved patient outcomes.
Apply the Sgarbossa Criteria in ECG Interpretation
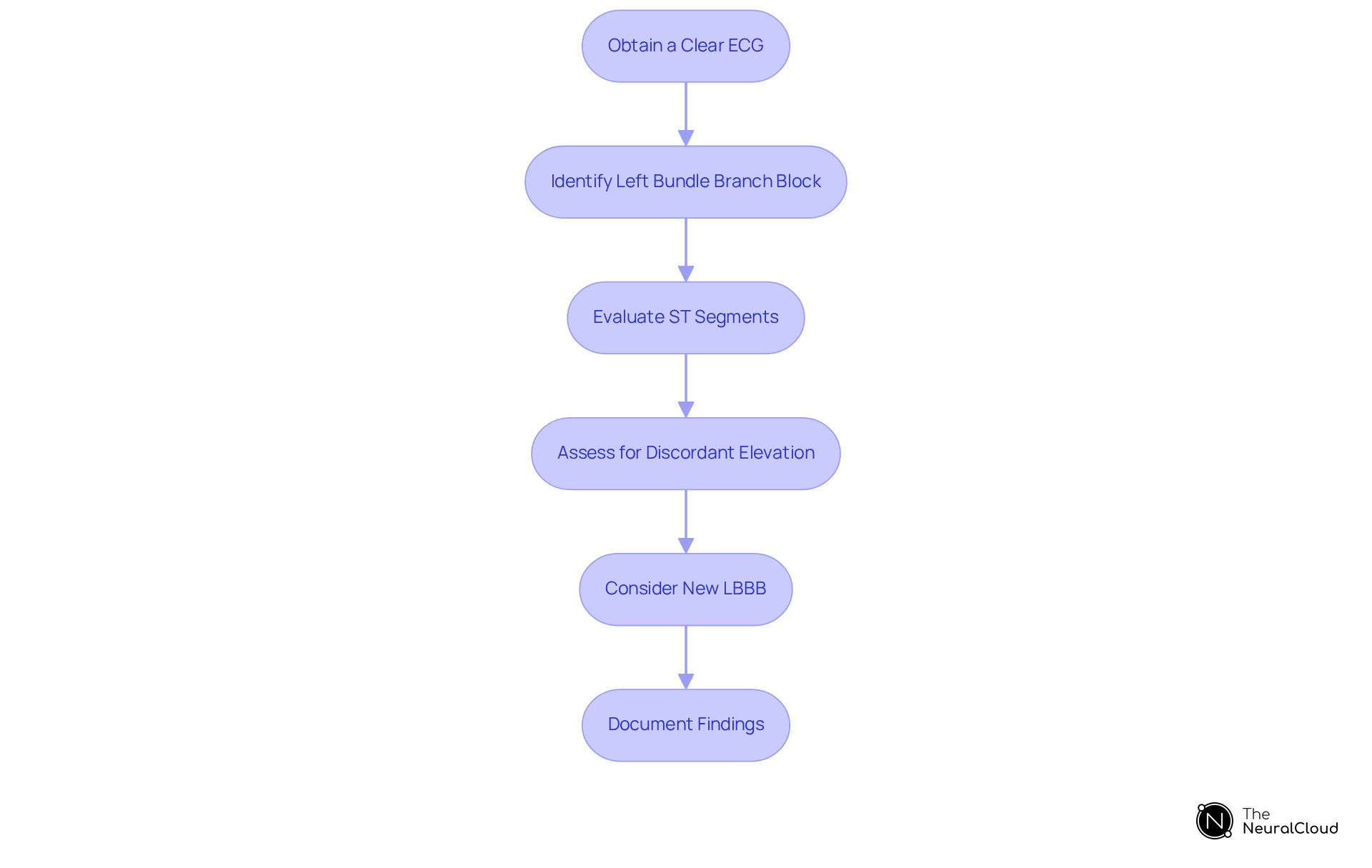
To effectively apply the Sgarbossa Criteria in ECG interpretation, follow these best practices:
- Obtain a Clear ECG: Utilize the MaxYield™ platform to enhance signal clarity and minimize artifacts. This ensures the ECG is free from noise that could obscure critical data. The platform's specifically address noise and signal artifacts, which improves the accuracy of cardiac insights.
- Identify Left Bundle Branch Block: Recognize the hallmark features of Left Bundle Branch Block, including a widened QRS complex exceeding 120 ms and a characteristic pattern observable in leads I, aVL, V5, and V6.
- Evaluate ST Segments: Assess for ST segment elevation in leads V1, V2, or V3. It is crucial to confirm that any observed elevation is concordant with the QRS complex for accurate interpretation.
- Assess for Discordant Elevation: Look for ST segment elevation of 5 mm or more that is discordant to the QRS complex. This is a significant indicator for diagnosing Acute Myocardial Infarction (AMI).
- Consider New LBBB: In cases where a patient presents with chest pain and a new LBBB, apply the criteria to assess for possible AMI.
- Document Findings: Clearly record your observations and interpretations, ensuring that all relevant criteria are noted for further review by colleagues or specialists.
By adhering to these steps, clinicians can effectively utilize the Sgarbossa criteria in conjunction with the advanced capabilities of the MaxYield™ platform to enhance diagnostic accuracy, particularly in complex cases. The automation of ECG analysis streamlines the process, allowing healthcare professionals to focus on critical decision-making, ultimately improving patient outcomes. For instance, the MaxYield™ platform processes over 200,000 heartbeats in under five minutes, significantly enhancing workflow efficiency and enabling timely interventions.
Troubleshoot Common Issues in ECG Interpretation
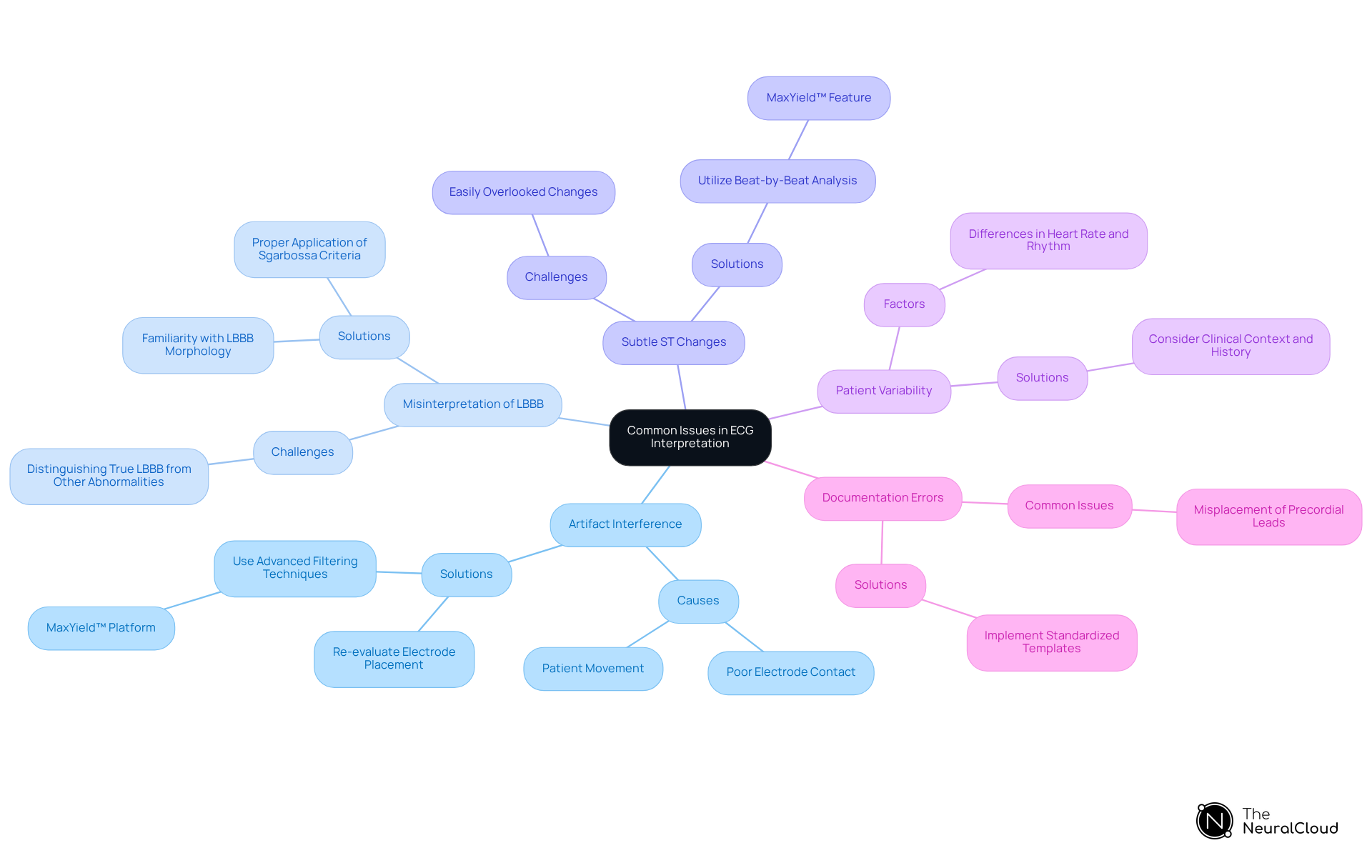
When interpreting ECGs, clinicians may encounter several common issues that can impact diagnostic accuracy according to the .
- Artifact Interference: Artifacts can significantly distort ECG readings. To mitigate this, it is essential to ensure that the ECG is free from noise by re-evaluating electrode placements and employing advanced filtering techniques, such as those available in the MaxYield™ platform. This platform effectively addresses noise and signal artifacts. Notably, MaxYield™ processes over 200,000 heartbeats in under five minutes, enhancing the speed and clarity of ECG analysis.
- Misinterpretation of Left Bundle Branch Block: Distinguishing between true Left Bundle Branch Block and other conduction abnormalities can be complex. Familiarity with the specific morphology of LBBB is crucial to avoid misdiagnosis, as improper interpretation of the Sgarbossa criteria can result in unnecessary interventions. As noted by Antonio Bayés De Luna, the presence of artifacts in ECG recordings may induce important diagnostic errors leading to unnecessary therapeutic interventions.
- Subtle ST Changes: ST segment changes may sometimes be subtle and easily overlooked. Utilizing the beat-by-beat analysis feature of MaxYield™ enhances the visibility of these changes, allowing for more accurate detection of potential ischemic events.
- Patient Variability: Physiological variability, such as differences in heart rate and rhythm, can affect ECG readings. Always consider the patient's clinical context and history when interpreting results, as this can provide critical insights into the observed ECG patterns.
- Documentation Errors: Accurate documentation of findings is crucial. Miscommunication can result in incorrect treatment decisions. The misplacement of precordial lead electrodes is the most frequent error found when 12-lead ECGs are performed, underscoring the significance of proper lead placement in documentation. Implementing standardized templates can streamline documentation processes, ensuring that all relevant information is captured and communicated effectively.
By proactively addressing these common issues, clinicians can enhance their ECG interpretation skills, leading to improved patient outcomes and more effective management of cardiac conditions.
Conclusion
Mastering the Sgarbossa criteria is crucial for clinicians aiming to accurately interpret ECGs, particularly in the context of diagnosing acute myocardial infarction (AMI) in patients with left bundle branch block (LBBB). Understanding the components of concordant ST elevation, excessive discordant ST elevation, and new LBBB enhances diagnostic capabilities, enabling healthcare professionals to differentiate between true ischemic changes and other factors that may mimic them.
The article emphasizes the importance of effectively applying the Sgarbossa criteria through best practices such as:
- Obtaining clear ECGs
- Recognizing left bundle branch block features
- Meticulously assessing ST segments
It also highlights common issues that may arise during ECG interpretation, including:
- Artifact interference
- Misinterpretation of LBBB
While providing strategies to troubleshoot these challenges. Utilizing advanced platforms like MaxYield™ can significantly improve diagnostic accuracy and workflow efficiency, allowing clinicians to focus on critical decision-making.
Ultimately, the effective application of the Sgarbossa criteria not only enhances individual diagnostic skills but also contributes to better patient outcomes in cardiac care. By committing to continuous learning and addressing common pitfalls in ECG interpretation, healthcare professionals can ensure they are well-equipped to make timely and accurate diagnoses, reinforcing the significance of these criteria in clinical practice.
Frequently Asked Questions
What are the Sgarbossa criteria?
The Sgarbossa criteria are essential ECG indicators used to diagnose acute myocardial infarction (AMI) in patients with left bundle branch block (LBBB). They consist of three key components that aid in accurate assessment.
What are the three components of the Sgarbossa criteria?
The three components are: 1. Concordant ST Elevation: ST segment elevation of 1 mm or more in leads V1, V2, or V3, aligned with the QRS complex (+5 points). 2. Excessive Discordant ST Elevation: ST segment elevation of 5 mm or more opposing the QRS complex (+2 points). 3. New Left Bundle Branch Block: The onset of a new left bundle branch block occurring with chest pain or other AMI-related symptoms.
How do the Sgarbossa criteria help in diagnosing AMI?
The Sgarbossa criteria help differentiate genuine ischemic changes from those that may be misattributed to LBBB, thus aiding clinicians in accurately diagnosing AMI.
What is the significance of scoring in the Sgarbossa criteria?
A score of ≥ 3 based on the Sgarbossa criteria has demonstrated a sensitivity of 36% and specificity of 96% in validation samples, while the derivation sample showed a sensitivity of 78% and specificity of 90%, indicating their clinical relevance.
Have the Sgarbossa criteria been revised?
Yes, the revised Sgarbossa criteria have been validated for clinical use, addressing limitations of the original standards, particularly regarding excessive discordance.
What challenges exist in implementing the Sgarbossa criteria?
Challenges include inter-observer variability, which requires extensive training for accurate application of the criteria in clinical settings.
How can familiarity with the Sgarbossa criteria improve patient outcomes?
Familiarity with the Sgarbossa criteria enhances clinicians' ability to apply them effectively in real-world scenarios, ultimately leading to improved patient outcomes.






