Overview
The article provides an overview of the diagnosis and treatment of accelerated junctional rhythm (AJR), which is defined by a heart rate ranging from 60 to 100 beats per minute that originates from the AV junction. It highlights the critical role of ECG analysis in identifying AJR and its underlying causes, such as digoxin toxicity and ischemic heart disease. Furthermore, the article outlines various treatment strategies, which can include:
- Observation
- Adjustments in medication
- In symptomatic cases, potential catheter ablation
By addressing these elements, the article aims to enhance understanding and management of AJR within clinical practice.
Introduction
Understanding accelerated junctional rhythm (AJR) is crucial for healthcare professionals, as it often serves as a window into underlying cardiac conditions. Characterized by a heart rate between 60 and 100 beats per minute, this rhythm can indicate issues ranging from digoxin toxicity to ischemic heart disease.
As the medical community continues to refine diagnostic techniques and treatment strategies, the challenge remains: how can clinicians effectively identify and manage AJR to prevent complications?
This article delves into the intricacies of AJR, offering insights into its diagnosis, clinical significance, and the latest treatment approaches that can enhance patient outcomes.
Define Accelerated Junctional Rhythm: Key Characteristics and Mechanisms
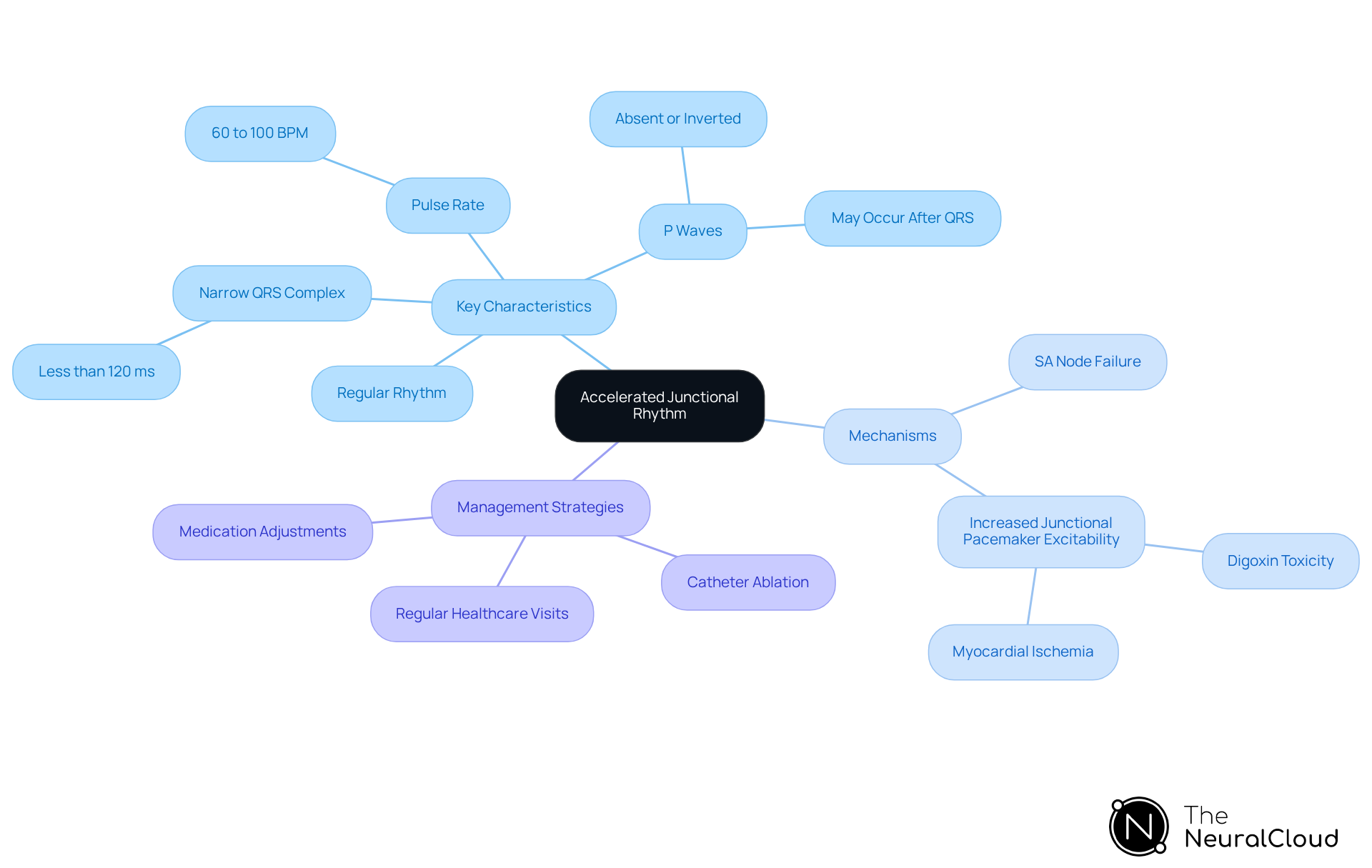
Accelerated junctional rhythm rate is characterized by a pulse rate typically ranging from 60 to 100 beats per minute, originating from the atrioventricular (AV) junction. The accelerated junctional rhythm rate occurs when the automatic firing of the AV node surpasses that of the sinoatrial (SA) node, leading to a pulse rate that is faster than normal. Key features of AJR include:
- Narrow QRS Complex: The duration of the QRS complex is generally less than 120 milliseconds, unless there is a pre-existing bundle branch block.
- P Waves: P waves may be absent, inverted, or occur after the QRS complex, making careful ECG analysis essential. Advanced platforms like MaxYield™ facilitate this analysis by isolating and labeling key features, even in recordings with significant noise. MaxYield™ offers detailed insights into P-wave, QRS complex, and T-wave analysis, thereby enhancing the accuracy of ECG interpretation.
- Regular Rhythm: AJR typically presents a regular rhythm, which aids in differentiating it from other junctional rhythms.
Recognizing these characteristics is crucial for identifying the accelerated junctional rhythm rate on an ECG and distinguishing it from junctional escape rhythms and junctional tachycardia. The mechanisms underlying the accelerated junctional rhythm rate involve either the failure of the SA node to generate impulses or increased excitability of junctional pacemaker cells, influenced by factors such as digoxin toxicity and myocardial ischemia.
Identifying the underlying causes of accelerated junctional rhythm rate is vital for implementing effective management strategies. Treatment may involve medication adjustments or catheter ablation, especially in symptomatic cases. Recent studies underscore the prevalence of AJR in both asymptomatic individuals and those with underlying cardiovascular conditions, highlighting the necessity for tailored management strategies. Regular healthcare visits are essential for monitoring the progression or resolution of AJR, as untreated cases may lead to complications, including the progression to more severe arrhythmias. Utilizing advanced tools like MaxYield™ can significantly , fostering more confident clinical decision-making.
Clinical Significance and Treatment Approaches for Accelerated Junctional Rhythm
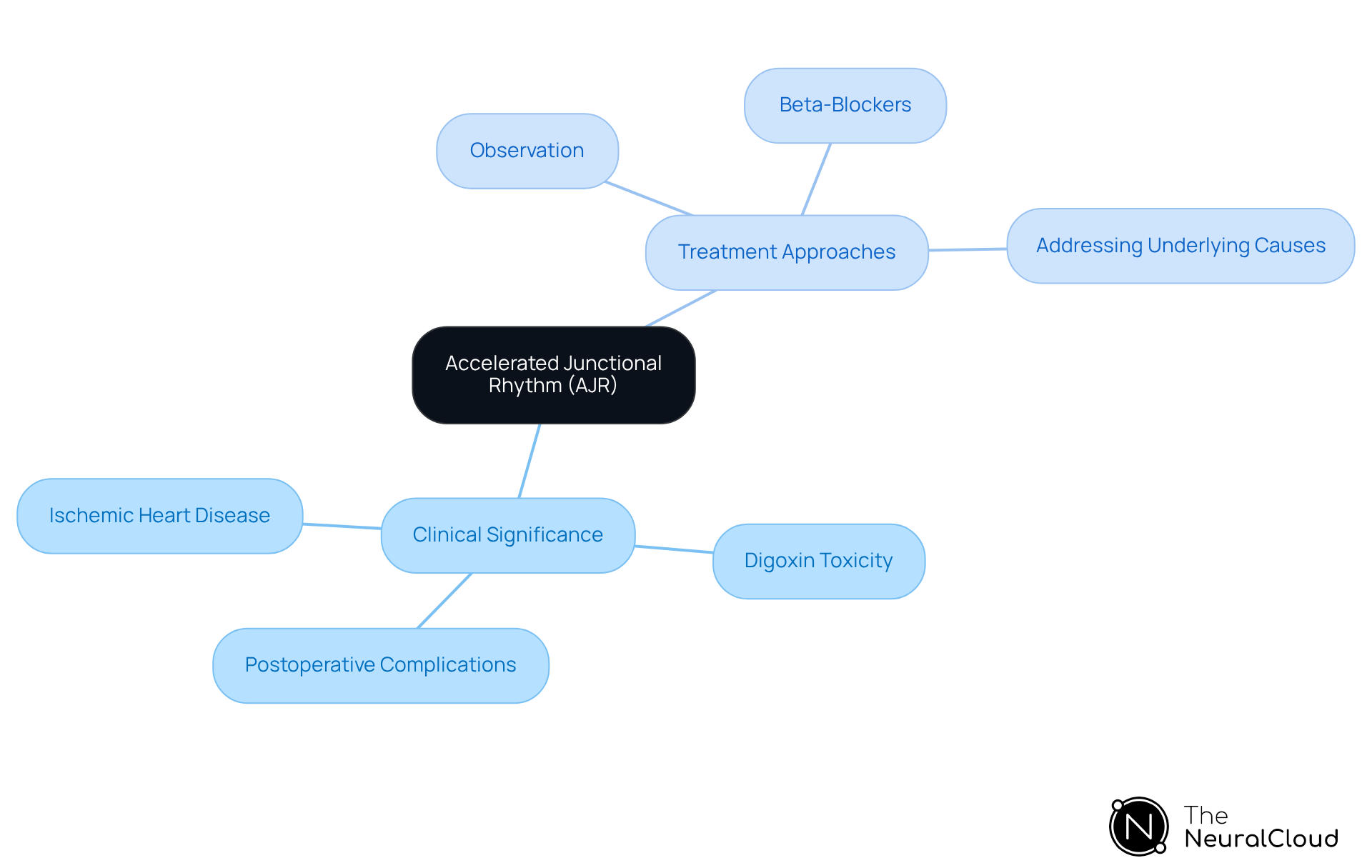
The clinical significance of [Accelerated Junctional Rhythm](https://healthline.com/health/accelerated-junctional-rhythm) (AJR) is noteworthy, as it may indicate underlying cardiac issues, including:
- Ischemic Heart Disease: AJR can suggest myocardial ischemia, which necessitates further evaluation.
- Digoxin Toxicity: Elevated digoxin levels may lead to an accelerated junctional rhythm rate, necessitating immediate attention to medication management.
- Postoperative Complications: Following cardiac surgery, the occurrence of an accelerated junctional rhythm rate (AJR) may arise, indicating the necessity for monitoring and potential intervention.
- Observation: For asymptomatic patients who are hemodynamically stable, observation may suffice.
- Beta-Blockers: Symptomatic patients often receive oral beta-blockers as the primary treatment to manage pulse rate and alleviate symptoms.
- Addressing Underlying Causes: Treatment should prioritize correcting any underlying issues, such as adjusting medications or managing electrolyte imbalances.
In instances where the accelerated junctional rhythm rate is symptomatic or persistent, further interventions, including catheter ablation, may be considered.
Diagnosis of Accelerated Junctional Rhythm: Techniques and Criteria
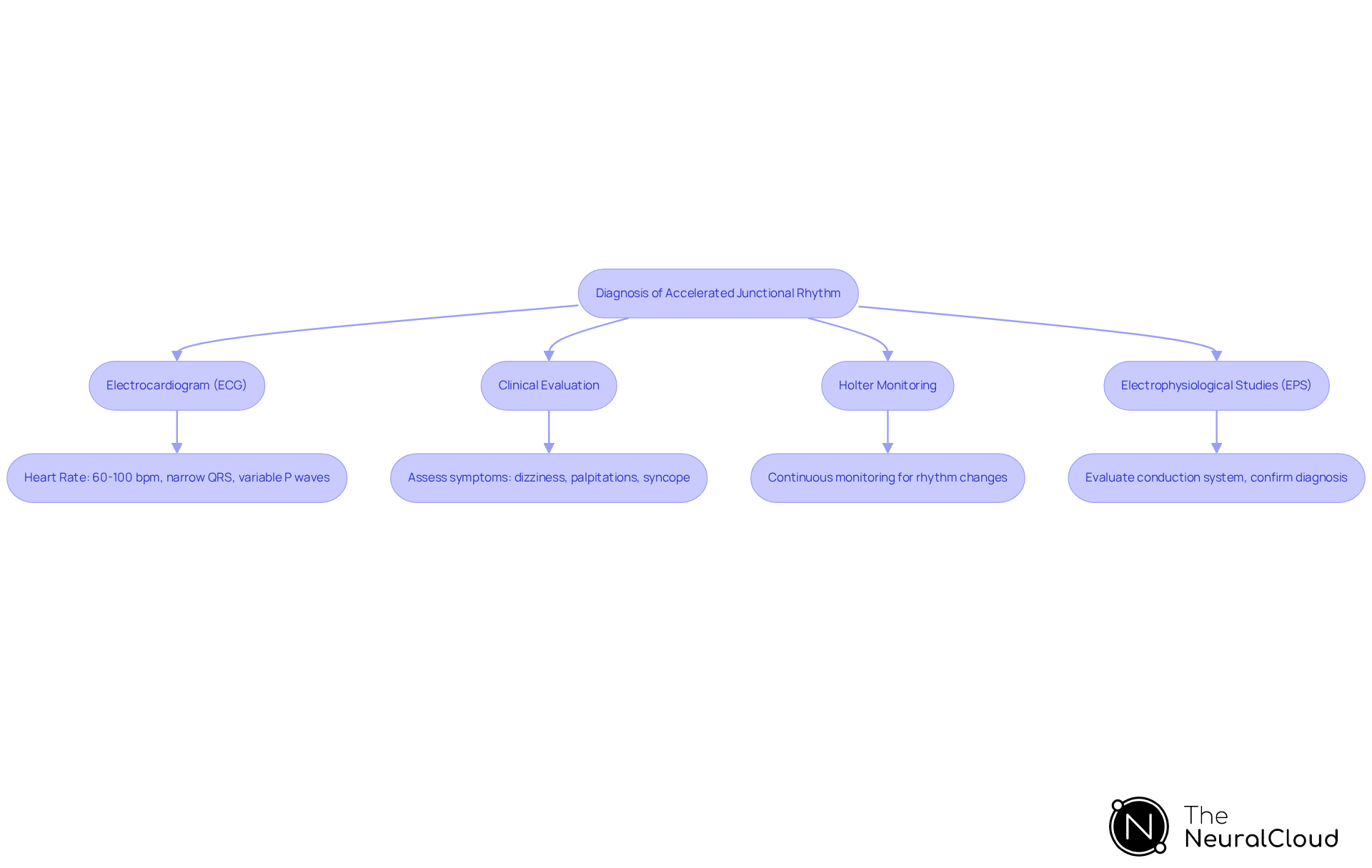
Diagnosing accelerated junctional rhythm rate (AJR) involves several key techniques and criteria.
Electrocardiogram (ECG) serves as the cornerstone of diagnosis. An ECG typically reveals a heart rate between 60 and 100 beats per minute (bpm), characterized by narrow QRS complexes and variable presentations of P waves. In some cases, inverted P waves may precede the QRS complexes, indicating junctional activity.
Clinical evaluation is crucial. A comprehensive medical history and physical examination help assess symptoms such as dizziness, palpitations, or syncope. This evaluation aids in identifying potential underlying conditions that may contribute to the rhythm disturbance.
Holter monitoring is often employed for continuous ECG monitoring, particularly in symptomatic patients. This method captures intermittent episodes of , allowing for the documentation of rhythm changes over an extended period, thus enhancing diagnostic accuracy.
In complex cases, Electrophysiological Studies (EPS) may be necessary. These invasive studies evaluate the conduction system and confirm the diagnosis, offering detailed insights into the organ's electrical pathways. This assists in differentiating AJR from other arrhythmias.
The diagnostic criteria for AJR include:
- Heart Rate: Confirmation of a heart rate exceeding 60 bpm is essential.
- Rhythm Regularity: Assessing the regularity of the rhythm on the ECG is vital.
- P Wave Analysis: Identifying the presence, absence, or inversion of P waves in relation to the QRS complex is critical for distinguishing AJR from other arrhythmias.
By employing these techniques and criteria, healthcare professionals can accurately diagnose AJR and differentiate it from other arrhythmias. This ensures appropriate management and treatment strategies.
Conclusion
Accelerated junctional rhythm (AJR) represents a critical cardiac condition that necessitates thorough understanding and careful management. This article outlines the defining characteristics of AJR, including its typical heart rate range, ECG features, and the underlying mechanisms contributing to its occurrence. Recognizing these elements is essential for accurate diagnosis and effective treatment.
Key insights emphasize the importance of differentiating AJR from other arrhythmias through precise ECG analysis and clinical evaluation. The discussion of various treatment approaches—ranging from observation and medication adjustments to more invasive interventions like catheter ablation—highlights the necessity of tailored management strategies based on patient symptoms and underlying conditions.
Ultimately, the significance of mastering the diagnosis and treatment of accelerated junctional rhythm cannot be overstated. As healthcare professionals engage with recent research and advancements in diagnostic techniques, including tools like Holter monitoring and electrophysiological studies, they can enhance their clinical decision-making. This proactive approach not only improves patient outcomes but also fosters a deeper understanding of cardiac health, underscoring the need for continuous education and vigilance in the management of AJR.
Frequently Asked Questions
What is accelerated junctional rhythm (AJR)?
Accelerated junctional rhythm is characterized by a pulse rate typically ranging from 60 to 100 beats per minute, originating from the atrioventricular (AV) junction, occurring when the AV node's automatic firing surpasses that of the sinoatrial (SA) node.
What are the key characteristics of AJR?
Key characteristics of AJR include a narrow QRS complex (less than 120 milliseconds unless there is a bundle branch block), potentially absent or inverted P waves, and a regular rhythm.
How does the QRS complex appear in AJR?
The QRS complex in AJR is usually narrow, with a duration of less than 120 milliseconds, unless there is a pre-existing bundle branch block.
What can be observed regarding P waves in AJR?
In AJR, P waves may be absent, inverted, or occur after the QRS complex, which necessitates careful ECG analysis for accurate identification.
What tools can assist in analyzing AJR on an ECG?
Tools like MaxYield™ can help isolate and label key features of AJR on an ECG, providing detailed insights into P-wave, QRS complex, and T-wave analysis, even in noisy recordings.
What mechanisms lead to the occurrence of AJR?
The mechanisms underlying AJR include failure of the SA node to generate impulses or increased excitability of junctional pacemaker cells, often influenced by factors like digoxin toxicity and myocardial ischemia.
Why is identifying the underlying causes of AJR important?
Identifying the underlying causes of AJR is essential for implementing effective management strategies, which may involve medication adjustments or catheter ablation, particularly in symptomatic cases.
How prevalent is AJR in different populations?
Recent studies indicate that AJR is prevalent in both asymptomatic individuals and those with underlying cardiovascular conditions, highlighting the need for tailored management strategies.
What are the implications of untreated AJR?
Untreated AJR may lead to complications, including the progression to more severe arrhythmias, making regular healthcare visits important for monitoring its progression or resolution.
How can advanced tools like MaxYield™ improve clinical decision-making?
Advanced tools like MaxYield™ enhance the clarity of ECG readings, which fosters more confident clinical decision-making regarding the management of AJR.






