Overview
Inferior infarct, also known as lower wall myocardial infarction, is a significant condition resulting from obstruction in the right coronary artery. This obstruction leads to ischemia and potential complications, making timely diagnosis and management essential. Effective diagnosis relies heavily on ECG analysis and cardiac biomarkers. Comprehensive management strategies, which include:
- Immediate interventions
- The use of advanced technologies
are crucial for improving patient outcomes. These strategies not only enhance the quality of care but also reduce the risk of further cardiac events.
Introduction
Understanding the complexities of inferior infarcts is essential for healthcare professionals. These lower wall myocardial infarctions account for a significant portion of heart attack cases. Timely recognition and effective management can mitigate the risks associated with these conditions, ultimately improving patient outcomes.
However, accurately diagnosing inferior infarcts presents challenges, alongside navigating the myriad of potential complications that may arise.
What are the key diagnostic criteria and management strategies that empower clinicians to tackle this critical aspect of cardiac care?
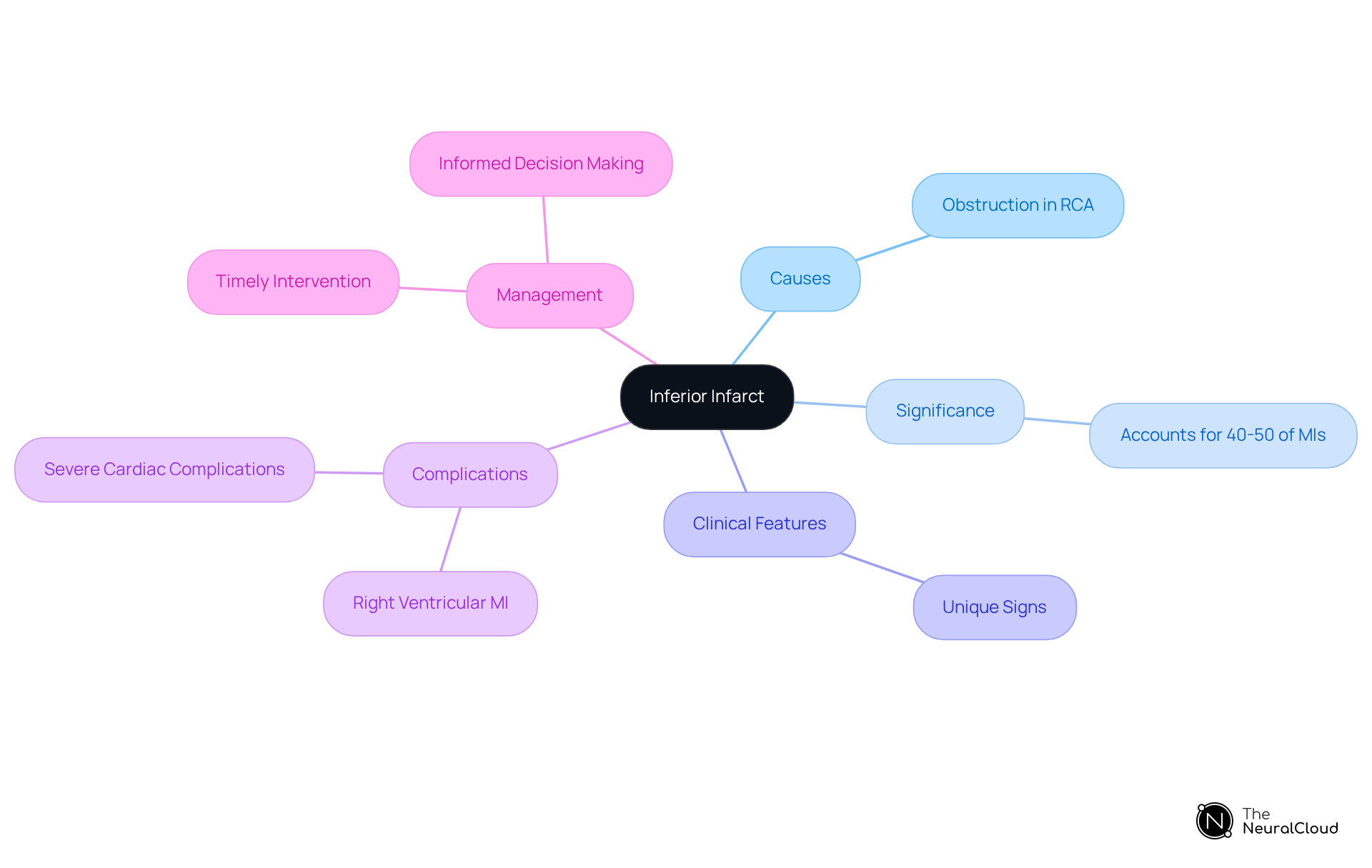
Define Inferior Infarct: Key Concepts and Importance
An infarct inferior, commonly known as lower wall myocardial infarction (MI), occurs when blood circulation to the heart's lower wall is obstructed, typically due to a blockage in the right coronary artery (RCA). This obstruction results in ischemia and subsequent necrosis of the myocardial tissue. Lower-quality heart attacks are particularly significant, accounting for approximately 40-50% of all MIs. They can present with unique clinical features, including potential complications such as right ventricular MI.
Recognizing the signs and manifestations of inadequate heart tissue damage is crucial for timely intervention and management. Delayed treatment can lead to severe cardiac complications or even death. Understanding the pathophysiology of infarct inferior events empowers healthcare professionals to make informed decisions regarding patient management and treatment strategies. This knowledge is essential for improving patient outcomes and ensuring effective care.
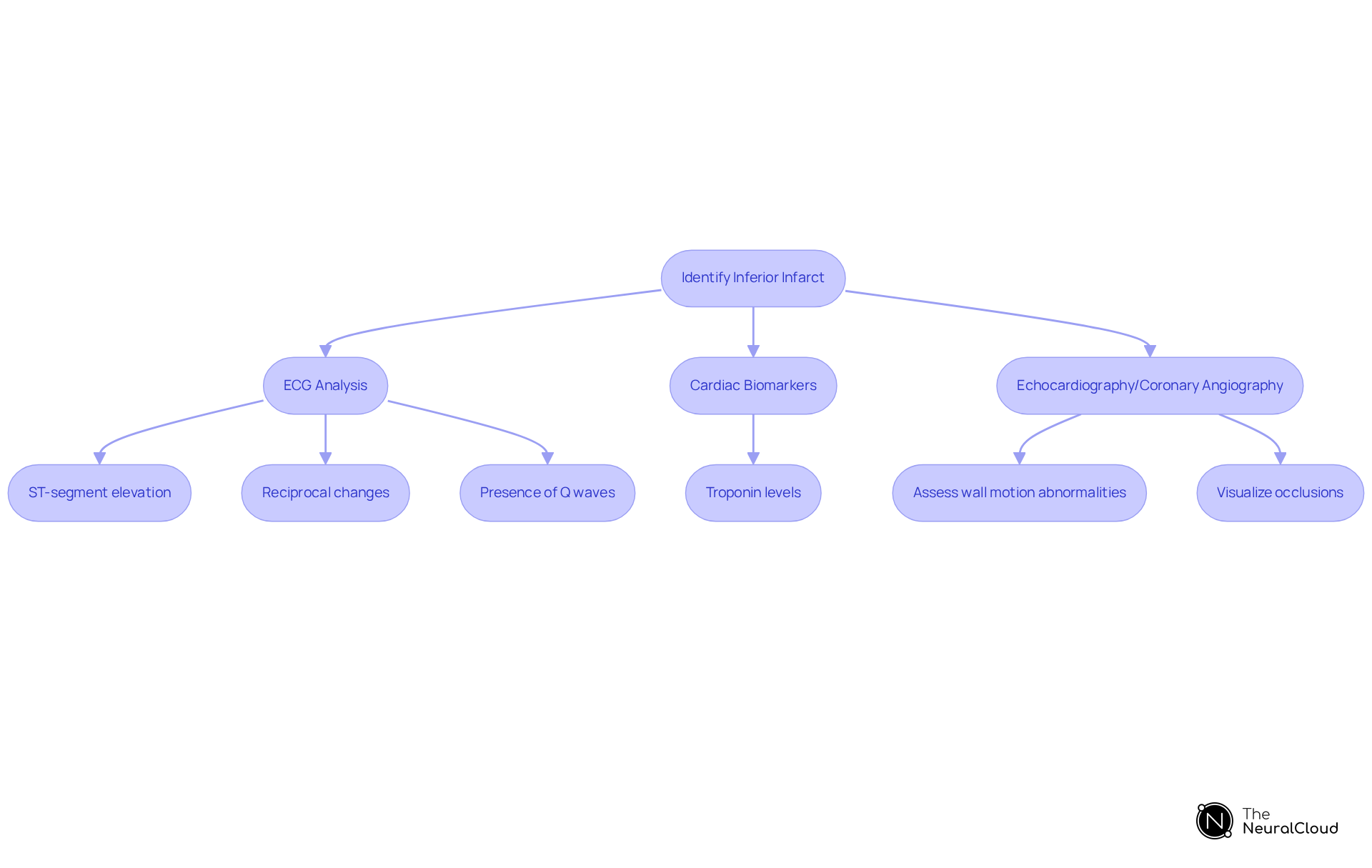
Diagnose Inferior Infarct: Criteria and Techniques
Identifying an infarct inferior in quality primarily depends on a thorough analysis of a 12-lead electrocardiogram (ECG). Essential criteria include:
- ST-segment elevation in leads II, III, and aVF, indicating involvement of the inferior wall.
- Reciprocal changes in leads I and aVL, which may indicate a lower myocardial infarction (MI).
- Presence of Q waves in the lower leads, indicating more advanced myocardial damage.
In addition to these ECG findings, clinicians often utilize complementary diagnostic techniques such as:
- Cardiac biomarkers, particularly troponin levels, to evaluate myocardial injury.
- Echocardiography to assess wall motion abnormalities and determine the extent of damage.
- Coronary angiography for direct visualization of any occlusions in the coronary arteries.
Utilizing these diagnostic instruments alongside clinical evaluations allows for a of patients believed to have an infarct inferior, ensuring prompt and suitable care. Recent updates in 12-lead ECG interpretation emphasize the significance of ST-segment elevation patterns, which are critical for accurate diagnosis and effective treatment strategies.
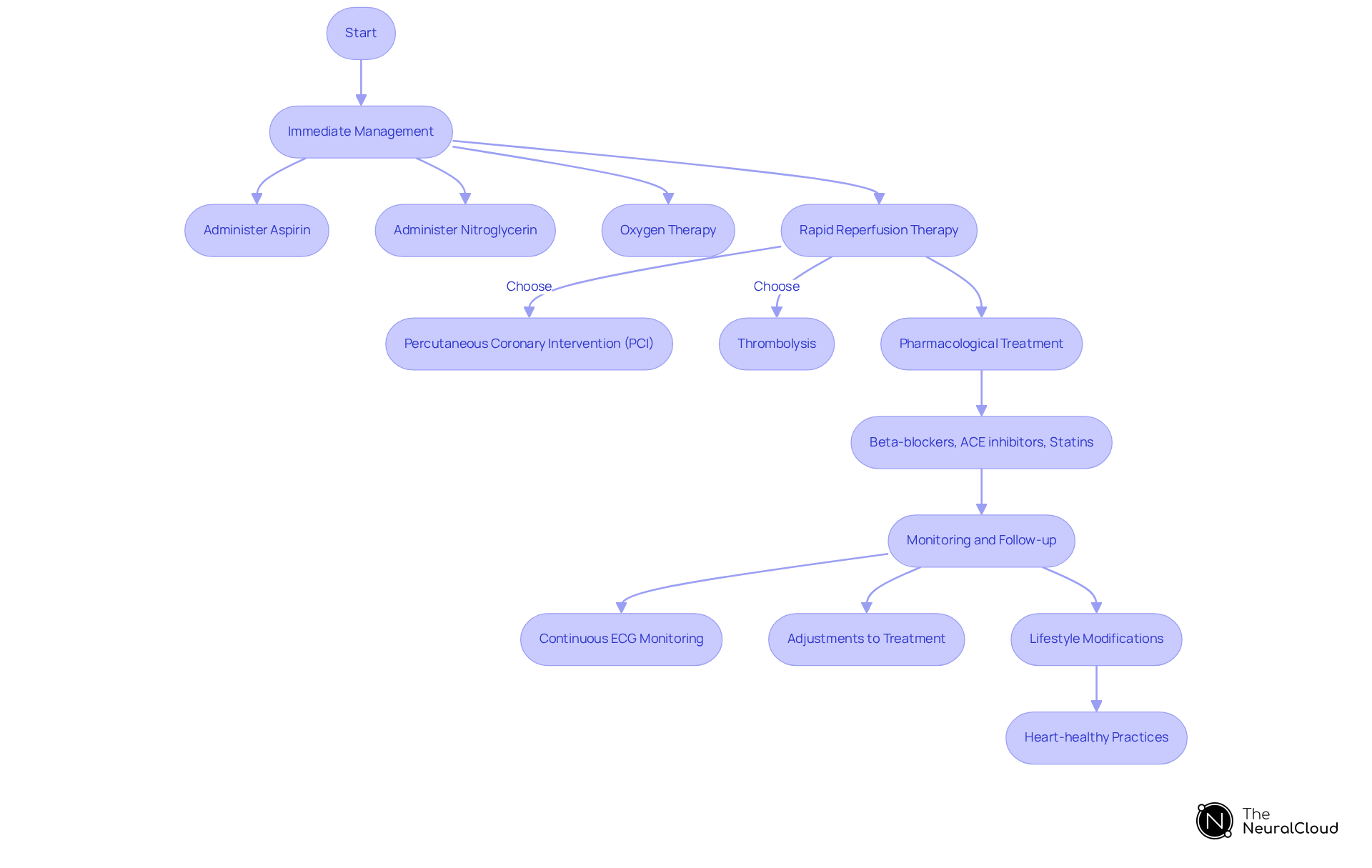
Management and Treatment Strategies for Inferior Infarct
Effective management of an infarct inferior myocardial infarction (MI) encompasses both immediate interventions and long-term treatment strategies.
Immediate Management: The initial response involves administering aspirin and nitroglycerin to mitigate clot formation and relieve chest pain. In cases of hypoxia, oxygen therapy is essential. Rapid reperfusion therapy, including percutaneous coronary intervention (PCI) or thrombolysis, is crucial for restoring blood flow to the affected area.
Pharmacological Treatment: A regimen typically includes beta-blockers, ACE inhibitors, and statins, which are vital for symptom management and the prevention of subsequent cardiac events. Furthermore, anticoagulants and antiplatelet agents are crucial in preventing additional clot formation, thus improving outcomes for individuals. The MaxYield™ platform from Neural Cloud Solutions enhances these pharmacological strategies by providing accurate ECG analysis that informs treatment decisions.
Monitoring and Follow-up: Continuous ECG monitoring is imperative to identify arrhythmias and other potential complications. The MaxYield™ platform utilizes to streamline ECG data processing, allowing healthcare providers to focus on high-level decision-making rather than time-consuming manual tasks. Regular follow-up appointments are necessary to evaluate cardiac function and make any necessary adjustments to the medication regimen.
Lifestyle Modifications: Encouraging patients to adopt heart-healthy practices is essential. This includes maintaining a balanced diet, engaging in regular physical activity, quitting smoking, and managing stress effectively.
By implementing these comprehensive strategies, healthcare providers can significantly reduce the risk of recurrent heart attacks and promote overall cardiac health.
Complications Associated with Inferior Infarct
Inferior infarcts can lead to several complications, including:
- Right Ventricular Infarction: Often associated with inferior MI, this condition can lead to right-sided heart failure and requires specific management strategies.
- Arrhythmias: These may include atrioventricular (AV) block, ventricular tachycardia, and fibrillation, all of which can be life-threatening and necessitate immediate intervention.
- Hypotension: Resulting from decreased cardiac output, this condition requires careful fluid oversight and inotropic support.
- Papillary Muscle Dysfunction: This can lead to mitral regurgitation and heart failure, potentially necessitating surgical intervention.
- Pericarditis: Inflammation of the pericardium can cause chest pain and requires anti-inflammatory treatment.
Recognizing and managing these complications promptly is crucial for and reducing mortality rates.
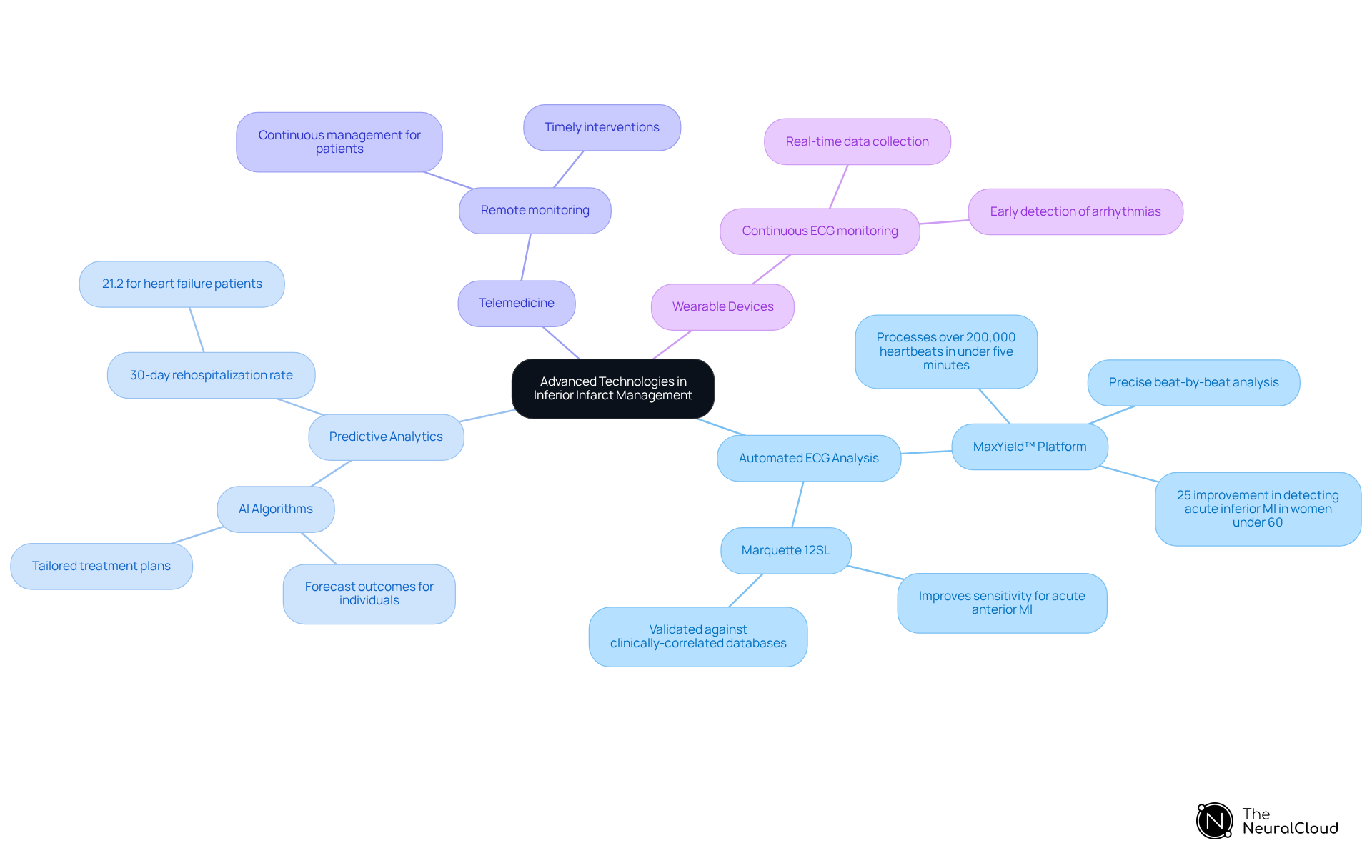
Role of Advanced Technologies in Inferior Infarct Management
Advanced technologies, particularly AI and machine learning, are revolutionizing the management of inferior infarcts in several key ways:
- Automated ECG Analysis: Platforms like Neural Cloud Solutions' MaxYield™ can process over 200,000 heartbeats in under five minutes, delivering precise beat-by-beat analysis. This includes the identification of critical features such as P-waves, QRS complexes, and T-wave intervals, significantly enhancing diagnostic accuracy and expediting clinical decision-making. The MaxYield™ platform builds upon advancements like the Marquette 12SL, which has shown a 25% relative improvement in detecting acute inferior myocardial infarction (MI) in women under 60.
- Predictive Analytics: AI algorithms are increasingly utilized to forecast outcomes for individuals and identify those at heightened risk for complications. This capability enables healthcare providers to create tailored treatment plans, enhancing the overall handling of cardiac conditions. Notably, the overall 30-day rehospitalization rate for individuals with heart failure is 21.2%, underscoring the importance of effective ECG analysis in decreasing readmissions.
- Telemedicine: The integration of remote monitoring and consultation capabilities facilitates continuous management of individuals, particularly beneficial for those in remote or underserved areas. This approach ensures timely interventions and ongoing evaluation of individual health.
- Wearable Devices: Continuous ECG monitoring through wearable technology provides real-time data, enabling early detection of arrhythmias and other cardiac issues. This is crucial for timely interventions and enhanced outcomes for individuals.
Incorporating these advanced technologies into clinical practice can significantly enhance the efficiency and effectiveness of managing inferior infarct, ultimately leading to better patient outcomes. The continuous learning model of MaxYield™ further enhances algorithm accuracy over time, ensuring that healthcare professionals can maximize their diagnostic yield.
Conclusion
Understanding inferior infarcts is essential for effective diagnosis and management of myocardial infarction, particularly given the significant implications for patient health. Insights into the pathophysiology, diagnostic criteria, and management strategies underscore the importance of promptly recognizing and addressing inferior myocardial infarction to improve outcomes.
The article highlights crucial aspects, including:
- The reliance on a 12-lead ECG for diagnosis
- The role of advanced technologies in enhancing diagnostic accuracy
- The comprehensive management strategies required to address potential complications
From immediate interventions to long-term lifestyle changes, each element plays a vital role in ensuring that patients receive optimal care following an inferior infarct.
Ultimately, integrating advanced technologies, such as AI and telemedicine, into clinical practice presents an exciting opportunity to enhance the efficiency and effectiveness of managing inferior infarcts. By prioritizing timely diagnosis and treatment, healthcare professionals can significantly reduce the risk of complications and improve overall health outcomes for individuals experiencing this serious condition. Engaging with the latest advancements in diagnostic tools and treatment protocols is essential for all healthcare providers dedicated to improving cardiac care.
Frequently Asked Questions
What is an inferior infarct?
An inferior infarct, also known as lower wall myocardial infarction (MI), occurs when blood circulation to the heart's lower wall is obstructed, typically due to a blockage in the right coronary artery (RCA), leading to ischemia and necrosis of the myocardial tissue.
How common are inferior infarcts among heart attacks?
Inferior infarcts are significant, accounting for approximately 40-50% of all myocardial infarctions (MIs).
What are some unique clinical features of inferior infarcts?
Inferior infarcts can present with unique clinical features, including potential complications such as right ventricular myocardial infarction (MI).
Why is it important to recognize the signs of inferior infarcts?
Recognizing the signs and manifestations of inferior infarcts is crucial for timely intervention and management, as delayed treatment can lead to severe cardiac complications or even death.
What diagnostic criteria are used to identify an inferior infarct?
Key diagnostic criteria for identifying an inferior infarct include ST-segment elevation in leads II, III, and aVF, reciprocal changes in leads I and aVL, and the presence of Q waves in the lower leads.
What complementary diagnostic techniques are used alongside ECG for inferior infarcts?
Complementary diagnostic techniques include measuring cardiac biomarkers like troponin levels, echocardiography to assess wall motion abnormalities, and coronary angiography for direct visualization of occlusions in the coronary arteries.
How does the 12-lead ECG play a role in diagnosing inferior infarcts?
A thorough analysis of a 12-lead electrocardiogram (ECG) is essential for diagnosing inferior infarcts, with emphasis on ST-segment elevation patterns critical for accurate diagnosis and effective treatment strategies.






