Overview
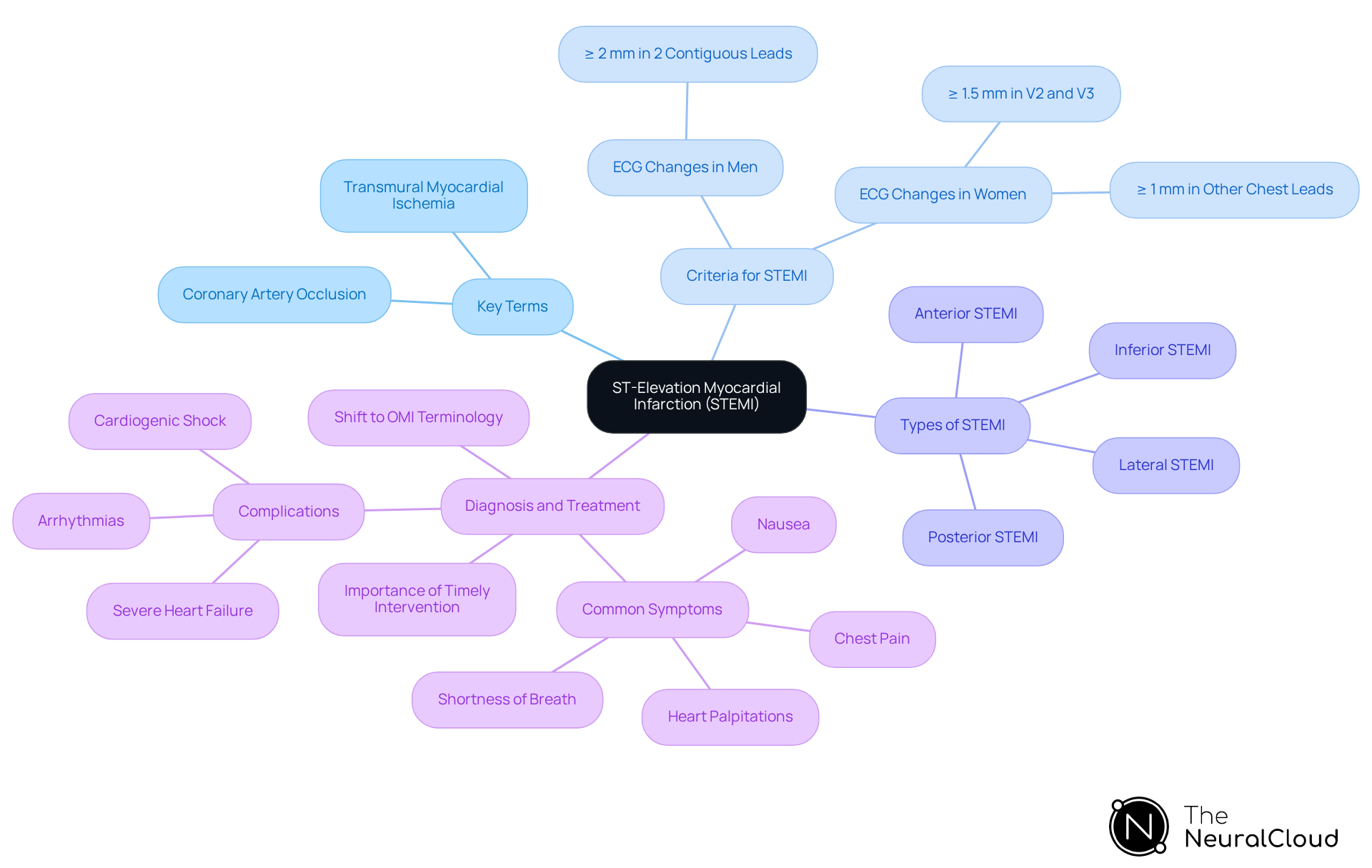
The article provides an overview of the criteria necessary for diagnosing and managing ST-Elevation Myocardial Infarction (STEMI). It emphasizes the critical role of recognizing ST-segment elevation on ECG and the necessity of timely intervention. By detailing specific diagnostic criteria and treatment protocols, such as reperfusion therapy, the article highlights the urgency of rapid care. This approach aims to minimize myocardial damage and ultimately improve patient outcomes.
Introduction
Understanding ST-Elevation Myocardial Infarction (STEMI) is essential for healthcare professionals, as timely recognition and intervention can significantly affect patient outcomes. This article explores the critical definitions, diagnostic criteria, and treatment protocols related to STEMI, providing insights into the complexities of this serious cardiac condition.
With evolving terminology and diagnostic techniques, practitioners must consider how to accurately identify and manage STEMI in a fast-paced clinical environment. By enhancing their understanding, healthcare providers can improve their response and ultimately benefit patient care.
Define and Classify STEMI: Core Concepts and Terminology
ST-Elevation Myocardial Infarction (STEMI) signifies a serious type of acute coronary syndrome characterized by the total blockage of a coronary artery, leading to considerable myocardial ischemia. The diagnosis hinges on identifying ST-segment elevation in specific ECG leads, which are critical components of the criteria for STEMI necessary for timely intervention. Key terms include:
- Transmural Myocardial Ischemia: This condition indicates that the entire thickness of the heart muscle is compromised due to prolonged ischemia, often leading to irreversible damage if not addressed promptly.
- Coronary Artery Occlusion: This term describes the blockage of one or more coronary arteries, which is the primary underlying cause of a specific type of heart attack. Notably, research indicates that nearly one in three patients diagnosed with NSTEMI may actually have an occluded coronary artery, underscoring the importance of accurate diagnosis.
- Criteria for STEMI: Specific changes on an electrocardiogram indicate the presence of a heart attack, particularly ST-segment elevation of at least 1 mm in contiguous leads. In men, this elevation is typically greater than or equal to 2 mm in at least two contiguous leads, while in women, it is greater than or equal to 1.5 mm in V2 and V3 leads or greater than or equal to 1 mm in other chest leads.
STEMI can be classified into several types based on the affected area of the heart and corresponding ECG changes, including anterior, inferior, lateral, and posterior STEMI. This classification is essential for deciding the suitable approach. Recent discussions among cardiology experts suggest a shift in terminology from STEMI/NSTEMI to OMI/non-OMI to enhance clarity in diagnosis and treatment. This shift emphasizes the need for urgent intervention in cases of . Such advancements in understanding and terminology reflect ongoing efforts to improve patient outcomes in the management of myocardial infarctions.
Diagnose STEMI: Key ECG Criteria and Interpretation Techniques
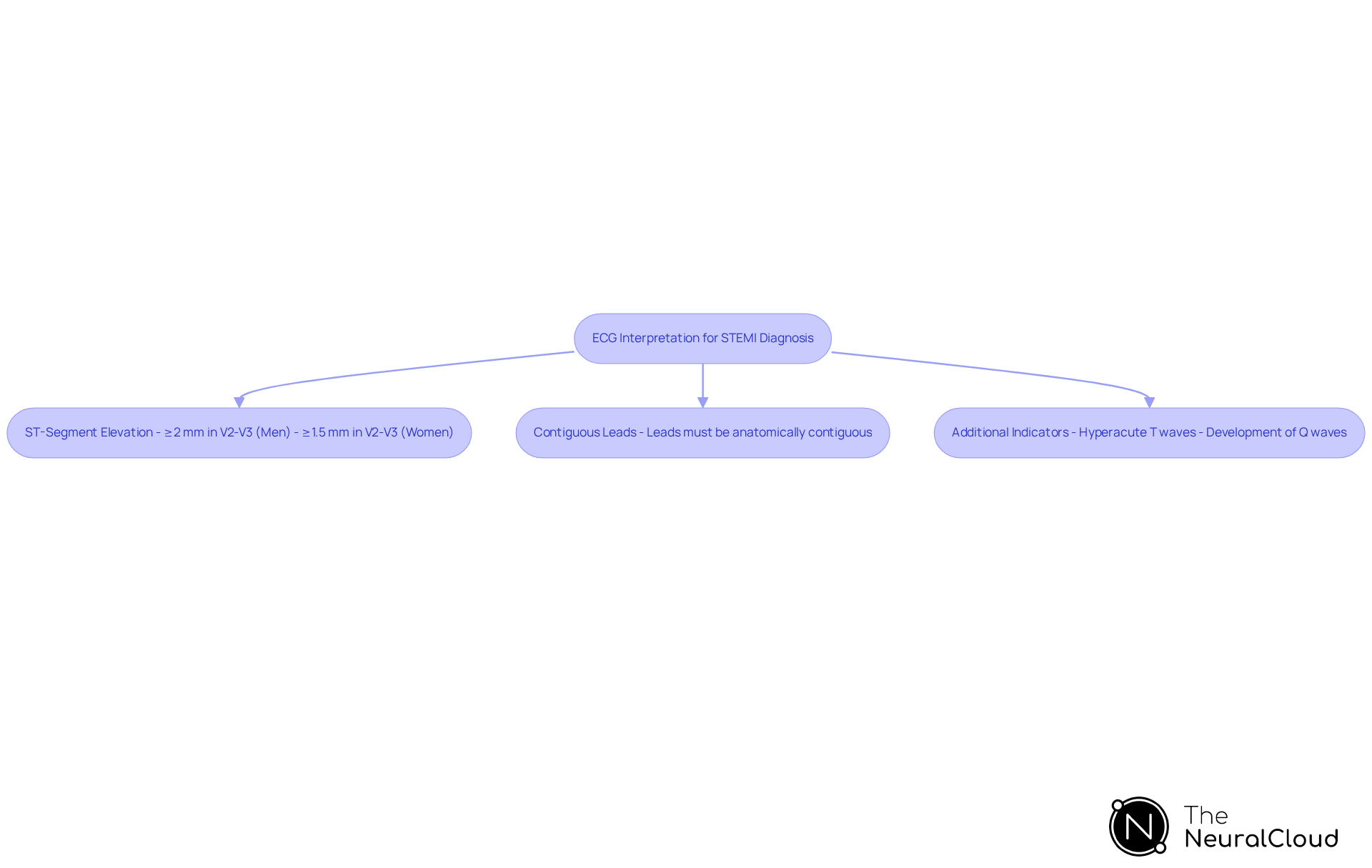
The identification of ST-Elevation Myocardial Infarction (STEMI) relies on the specific criteria for STEMI that healthcare professionals must acknowledge promptly. Key diagnostic points include:
- ST-Segment Elevation: A new ST-segment elevation at the J point in at least two contiguous leads is a definitive indicator of STEMI. For men, this elevation is typically ≥ 2 mm in leads V2-V3, while for women, it is ≥ 1.5 mm in the same leads. This differentiation is crucial for meeting the criteria for STEMI diagnosis.
- Contiguous Leads: The criteria for STEMI specify that the leads used for diagnosis must be anatomically contiguous, meaning they are adjacent on the body surface. This ensures that the are relevant to the same myocardial territory according to the criteria for STEMI.
- Additional Indicators: Other significant ECG changes that fulfill the criteria for STEMI may include hyperacute T waves, which are often the first ischemic changes observed, and the development of Q waves over time, indicating myocardial necrosis.
Healthcare professionals should adopt a systematic approach to ECG interpretation, integrating patient history and clinical presentation with ECG findings. The MaxYield™ platform enhances this process by utilizing advanced noise filtering and distinct wave recognition, allowing for the rapid isolation of critical ECG waves even in recordings with high levels of noise and artifact. For practical application, users can refer to the user manual for step-by-step guidance on utilizing these features effectively in diagnosing heart attacks.
The urgency of swift identification and care cannot be overstated, as the expression 'time is muscle' highlights the essential nature of timely intervention in heart attack situations. Recent advancements in ECG interpretation methods, such as the use of automated algorithms like those in MaxYield™, can further improve diagnostic accuracy and efficiency, ensuring that individuals receive the critical care they need without delay. It is also crucial to maintain a high level of suspicion for unusual presentations of heart attacks, especially in older, diabetic, and female individuals, who may display symptoms like fatigue or epigastric discomfort. The objective Door to Needle time for administering thrombolytics is under 30 minutes, and the Door to Balloon time for PCI must be below 90 minutes, emphasizing the time-sensitive aspect of myocardial infarction care.
Manage STEMI: Comprehensive Treatment Approaches and Protocols
The management of ST Elevation Myocardial Infarction (STEMI) must follow the criteria for STEMI, necessitating a comprehensive approach focused on achieving rapid reperfusion and minimizing myocardial damage. Key treatment strategies include:
- Reperfusion therapy
- Medications
- Monitoring and support
- Post-management protocols
Reperfusion therapy aims to restore blood flow to the ischemic area of the heart. This can be accomplished through:
PCI is the preferred method for most patients, involving balloon angioplasty and stenting. According to the criteria for STEMI, current guidelines recommend PCI as the primary intervention, particularly when it can be performed within 120 minutes of symptom onset. If PCI is unavailable or delayed, thrombolytic therapy is utilized. Thrombolytics, such as alteplase and tenecteplase, effectively , especially when administered within the first 12 hours of symptom onset.
Immediate administration of antiplatelet agents, including aspirin and clopidogrel, is critical for preventing further clot formation. Additional medications may include beta-blockers, ACE inhibitors, and statins to manage symptoms and reduce the risk of subsequent events. However, recent evidence raises concerns about the safety and efficacy of frequently utilized therapies, such as morphine and early beta-blockers, emphasizing the need for careful consideration in their application.
Continuous monitoring of vital signs and ECG is essential during treatment to detect any complications early. Supportive care, including oxygen therapy and pain management, should also be provided to enhance comfort and outcomes. It is important to note that supplemental oxygen therapy may lack benefit and could potentially harm individuals without hypoxia.
After initial care, patients should be evaluated for secondary prevention strategies. This includes lifestyle modifications, such as dietary changes and exercise, as well as long-term medication adherence to prevent recurrence. Recent studies emphasize the criteria for STEMI, indicating that prompt intervention is important, as delays in care can significantly increase mortality rates. The ESC has set a goal of administering fibrinolytics within 10 minutes of STEMI diagnosis to optimize outcomes. Additionally, disparities in access to PCI in the US can influence treatment outcomes, highlighting the need for equitable healthcare access. Real-world examples demonstrate that patients undergoing PCI generally experience better outcomes compared to those receiving thrombolytic therapy, particularly regarding reinfarction rates and overall survival. As guidelines continue to evolve, staying updated on the latest recommendations for reperfusion therapy is crucial for healthcare professionals involved in STEMI management.

Conclusion
Understanding the criteria for ST-Elevation Myocardial Infarction (STEMI) is crucial for timely diagnosis and effective management of this acute condition. This article highlights the importance of recognizing key definitions, diagnostic techniques, and comprehensive treatment strategies that can significantly impact patient outcomes. By grasping core concepts such as ST-segment elevation, coronary artery occlusion, and the classification of STEMI, healthcare professionals can enhance their ability to respond swiftly and appropriately.
The discussion encompasses essential diagnostic criteria, emphasizing the need for accurate ECG interpretation and the importance of recognizing variations in presentation, particularly among different patient demographics. Furthermore, the article outlines critical management protocols, including reperfusion therapy and post-management strategies, which are vital for minimizing myocardial damage and improving survival rates. Adhering to established guidelines and remaining vigilant for advancements in treatment can make a significant difference in care delivery.
In summary, a thorough understanding of STEMI—ranging from its definitions and diagnostic criteria to effective management protocols—serves as a foundation for improving patient care in acute coronary events. As the landscape of cardiovascular medicine evolves, continuous education and adaptation to new guidelines are imperative for healthcare professionals. Prioritizing timely intervention and comprehensive care not only enhances individual patient outcomes but also contributes to broader public health goals in managing heart disease.
Frequently Asked Questions
What does STEMI stand for and what does it signify?
STEMI stands for ST-Elevation Myocardial Infarction, which is a serious type of acute coronary syndrome characterized by the total blockage of a coronary artery, leading to significant myocardial ischemia.
How is STEMI diagnosed?
The diagnosis of STEMI is based on identifying ST-segment elevation in specific ECG leads, which are critical for determining the presence of a heart attack.
What is transmural myocardial ischemia?
Transmural myocardial ischemia indicates that the entire thickness of the heart muscle is compromised due to prolonged ischemia, often leading to irreversible damage if not addressed promptly.
What does coronary artery occlusion mean?
Coronary artery occlusion refers to the blockage of one or more coronary arteries, which is the primary underlying cause of a specific type of heart attack.
What are the criteria for diagnosing STEMI based on ECG changes?
The criteria for diagnosing STEMI include ST-segment elevation of at least 1 mm in contiguous leads. For men, this elevation is typically greater than or equal to 2 mm in at least two contiguous leads, while for women, it is greater than or equal to 1.5 mm in V2 and V3 leads or greater than or equal to 1 mm in other chest leads.
How can STEMI be classified?
STEMI can be classified into several types based on the affected area of the heart and corresponding ECG changes, including anterior, inferior, lateral, and posterior STEMI.
What recent changes in terminology regarding STEMI have been discussed among cardiology experts?
Recent discussions suggest a shift in terminology from STEMI/NSTEMI to OMI/non-OMI to enhance clarity in diagnosis and treatment, emphasizing the need for urgent intervention in cases of acute coronary occlusion.






