Overview
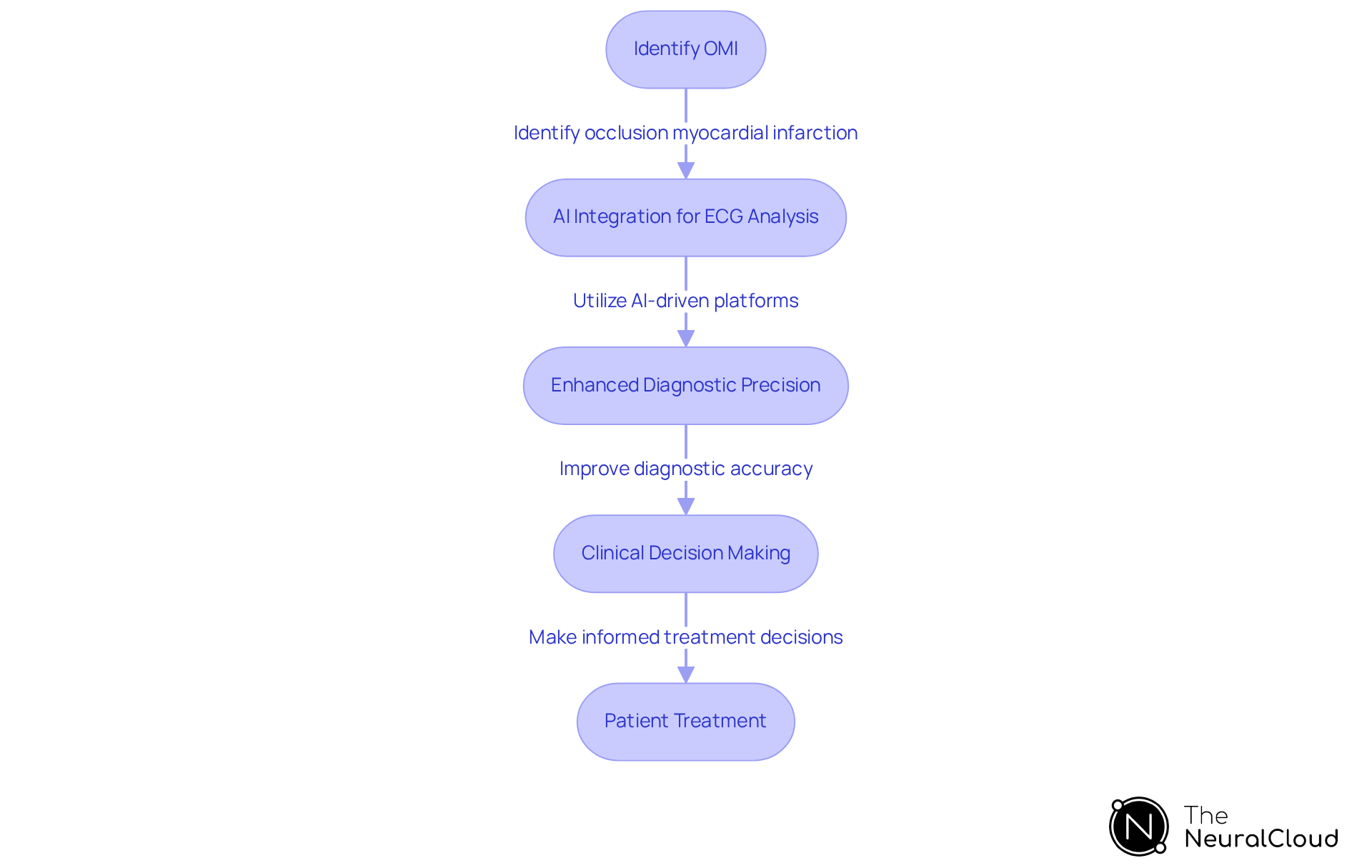
The article highlights the significance and applications of Occlusion Myocardial Infarction (OMI) within health technology. It underscores the critical nature of OMI and the advancements in diagnostic tools that enhance patient outcomes. Timely recognition and intervention for OMI are vital, as traditional methods frequently fail to identify this condition, resulting in treatment delays. The integration of AI-driven technologies notably improves diagnostic accuracy and facilitates quicker decision-making in acute care settings.
Introduction
Understanding Occlusion Myocardial Infarction (OMI) is increasingly critical in health technology, representing a pivotal shift in the classification and treatment of myocardial infarctions. This article explores the significance of OMI, emphasizing its implications for timely intervention and improved patient outcomes through advanced diagnostic tools. However, a challenge persists: how can healthcare professionals ensure the accurate identification and management of OMI in a landscape where traditional criteria may overlook this life-threatening condition?
Defining OMI: Meaning and Significance
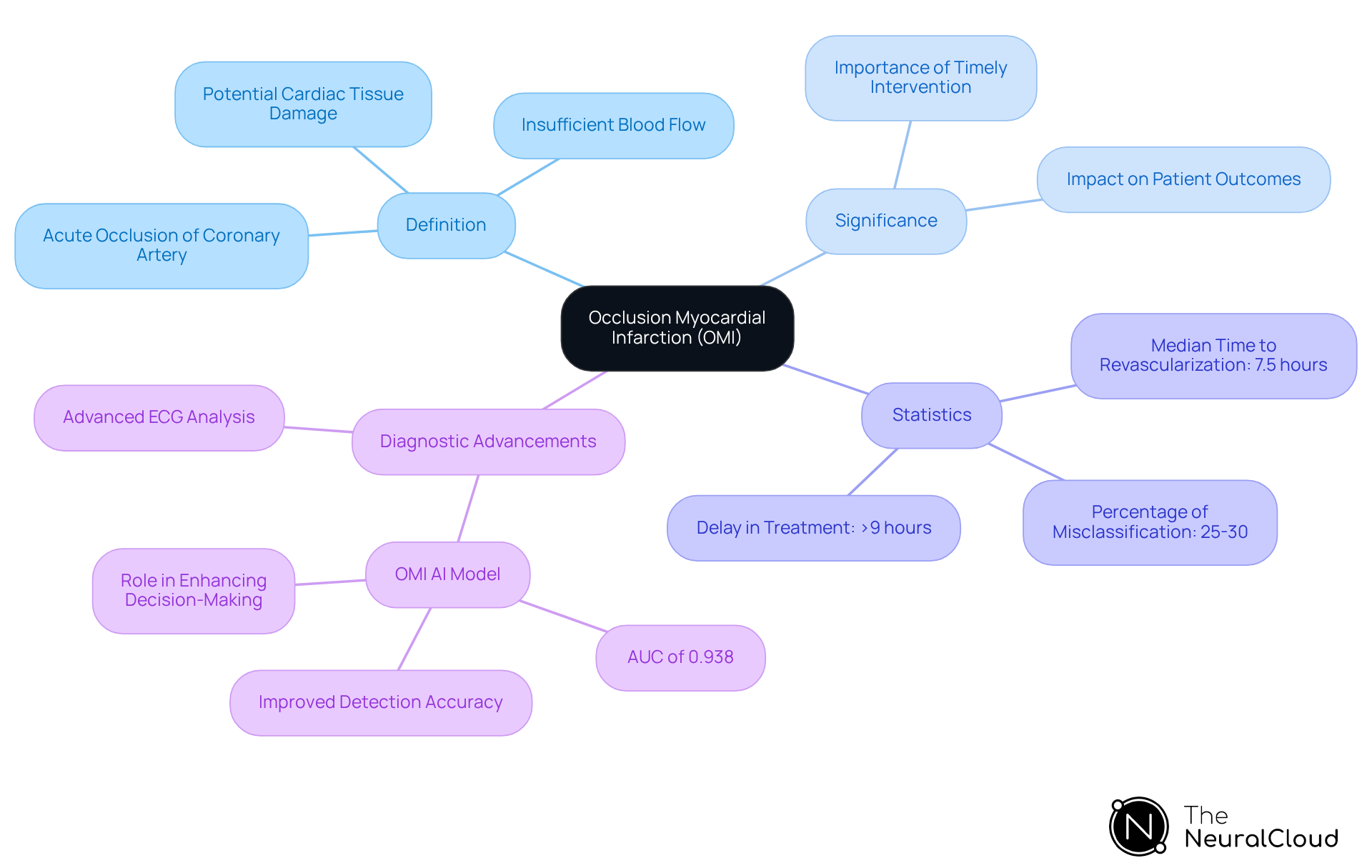
Occlusion Myocardial Infarction (OMI meaning) is a critical type of myocardial infarction, characterized by the acute or near-total occlusion of a coronary artery. This condition leads to insufficient blood flow to the heart muscle, potentially resulting in significant damage or necrosis of cardiac tissue if not addressed promptly. The differentiation of OMI meaning from other types of myocardial infarction, such as STEMI (ST-Elevation Myocardial Infarction), highlights the urgent need for immediate medical intervention to restore blood flow and mitigate heart damage.
Recognizing the OMI meaning is vital, as timely revascularization significantly enhances patient outcomes. Research indicates that individuals with what is known as OMI meaning who receive urgent reperfusion therapy experience substantial benefits, with the risks of the procedure outweighed by the potential for recovery. For example, less than half of OMI patients identified by standard STEMI criteria received timely revascularization, with a median delay exceeding nine hours, highlighting the severe consequences of misclassification. Approximately 25-30% of individuals with OMI meaning do not receive prompt treatment, which emphasizes the necessity of accurate identification of this condition.
Statistics demonstrate that the OMI AI model has shown superior accuracy in detecting the OMI meaning compared to traditional methods, achieving an area under the curve (AUC) of 0.938. This model plays a crucial role in accurately reclassifying one in three individuals presenting with chest pain, illustrating the importance for healthcare professionals to adopt advanced diagnostic tools, such as Neural Cloud Solutions' offerings, which enhance decision-making in acute care settings. The system effectively maps ECG signals through noise, isolating and labeling key features, including P-wave, QRS complex, and T-wave onsets and offsets. This sophisticated noise filtering and automated analysis convert noisy ECG recordings into clear, actionable insights, allowing clinicians to identify cardiac events more effectively.
Cardiologists stress the importance of recognizing OMI meaning, with one expert stating, 'If you have ongoing chest pain with ECG changes, just because they don’t meet arbitrary criteria set down in a clinical trial for defining ST-elevation MI doesn’t mean that the vessel isn’t blocked.' This viewpoint reinforces the need for clinicians to remain attentive and responsive to . Furthermore, the necessity to reconsider the term ST-elevation MI is highlighted, as it can lead to misinterpretations that delay essential interventions.
In summary, understanding the OMI meaning is crucial for healthcare professionals, as it directly influences treatment strategies and outcomes for patients. Prompt intervention is essential, and the integration of cutting-edge diagnostic technologies can significantly enhance the detection and management of this life-threatening condition.
Contexts of OMI: Applications Across Industries
The omi meaning, which refers to occlusion myocardial infarction (OMI), is critical in various healthcare contexts, particularly in emergency medicine and cardiology. Rapid identification of OMI meaning in emergency departments is essential, as timely interventions such as percutaneous coronary intervention (PCI) can greatly preserve heart function. Notably, 24-35% of patients with non-STEMI exhibit total coronary occlusion, which underscores the omi meaning and the urgency for prompt diagnosis. The integration of AI-driven platforms, like Neural Cloud Solutions' offerings, enhances OMI detection by analyzing ECG data in real-time, enabling healthcare providers to make swift, informed decisions. This system transforms lengthy and noisy ECG recordings into clean signals, streamlining clinical workflows, especially in settings where immediate access to specialists may be limited.
By 2025, AI ECG analysis has evolved significantly, with machine learning models showcasing superior capabilities in identifying subtle ischemic changes, which are indicative of omi meaning. For instance, a recent study revealed that the random forest model achieved an area under the receiver operating characteristic (AUROC) of 0.91, markedly outperforming practicing clinicians, who had an AUROC of 0.79. This advancement illustrates the potential of AI, particularly through platforms like MaxYield, to , especially in telemedicine applications where understanding the omi meaning is vital for timely diagnosis. The findings underscore the effectiveness of machine learning in detecting subtle ischemic ECG changes in the absence of a STEMI pattern.
Healthcare professionals express optimism about AI's role in the detection of omi meaning. Many emphasize that these technologies, equipped with sophisticated noise filtering and wave recognition capabilities, not only enhance diagnostic precision but also alleviate the burden on clinicians, allowing them to focus on patient care rather than manual data interpretation. Furthermore, the OMI risk score illustrates the omi meaning by categorizing 66% more individuals as low risk compared to the HEART score, highlighting AI's effectiveness in improving diagnostic accuracy. As the principles of omi meaning become increasingly integrated into training programs, recognizing occlusive events in acute care settings is crucial, ensuring healthcare providers are prepared to respond effectively to cardiac emergencies. However, it is important to note that 25-30% of individuals with OMI meaning do not receive timely treatment, underscoring the need for improved diagnostic tools and processes that AI, particularly through Neural Cloud Solutions' offerings, can facilitate.
The Origin of OMI: Historical Context and Evolution
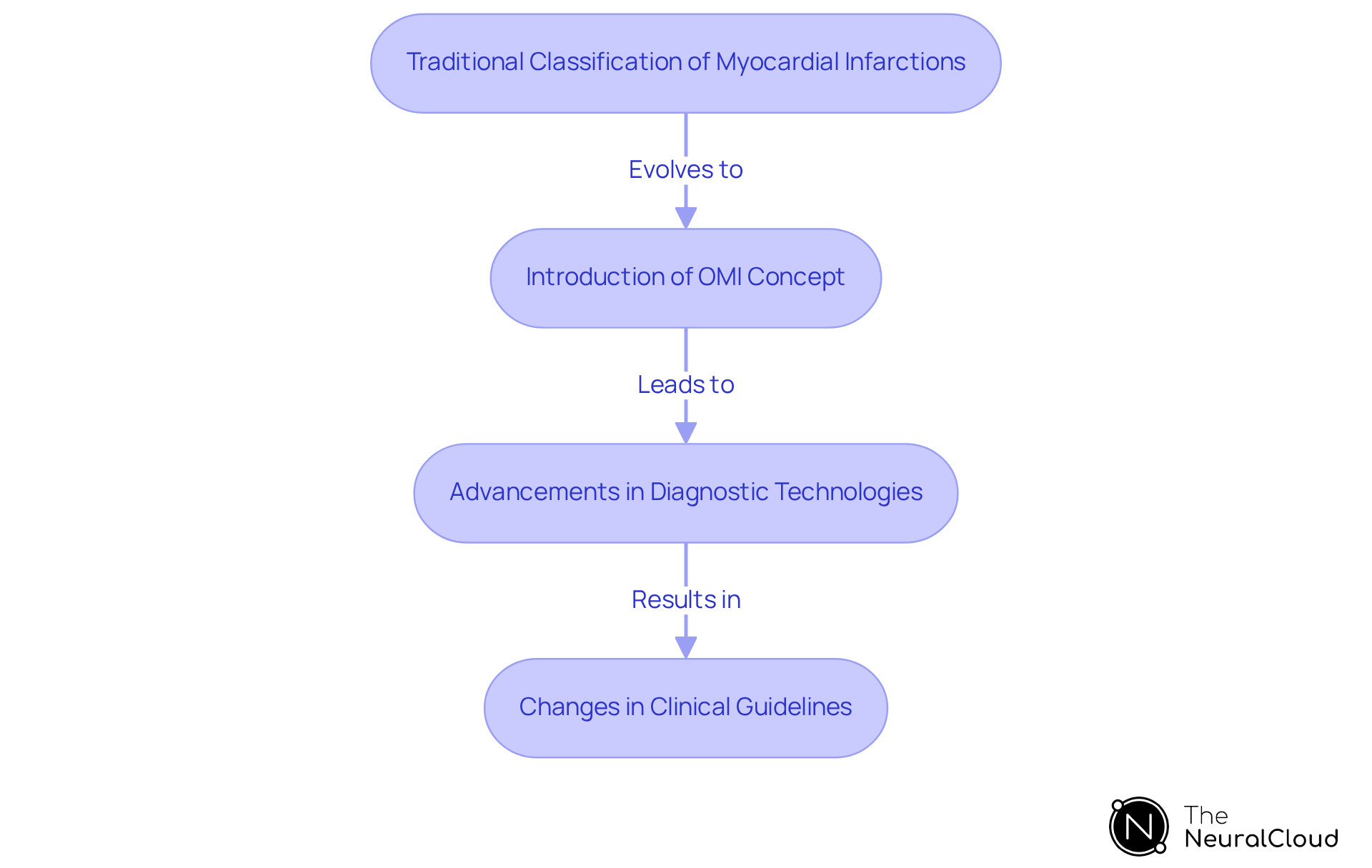
The concept of Occlusion Myocardial Infarction (OMI), or omi meaning, arose from the need to refine the classification of myocardial infarctions, particularly in light of advancements in diagnostic technologies. Traditionally, myocardial infarctions were categorized as either STEMI (ST-Elevation Myocardial Infarction) or NSTEMI (Non-ST-Elevation Myocardial Infarction). However, ongoing research has shown that occlusive events can occur without the classic ST-elevation patterns typically associated with STEMI. This discovery led to the introduction of the paradigm known as OMI meaning, which emphasizes the critical importance of recognizing acute coronary occlusions, regardless of conventional ECG criteria.
The OMI framework has gained significant traction in clinical guidelines and training programs, reflecting a broader shift towards more nuanced approaches in cardiac care. Studies indicate that event rate declines contributed to approximately two-thirds of the reductions in myocardial infarction mortality among women in regions such as Ontario and New Zealand. This underscores the omi meaning in enhancing patient outcomes.
Moreover, advancements in diagnostic technologies, particularly those provided by Neural Cloud Solutions, have been instrumental in clarifying omi meaning. The software efficiently labels P, QRS, and T Wave onsets, offsets, and time-series intervals in CSV format. This capability , allowing for the detection of subtle features that indicate occlusion. Consequently, this facilitates timely intervention and supports the identification of new digital biomarkers. Case studies suggest that integrating the omi meaning into clinical guidelines has led to improved recognition and management of myocardial infarction cases, ultimately enhancing care for individuals.
Expert opinions advocate that the incorporation of both ECG findings and clinical parameters into the OMI meaning should promote a comprehensive approach to acute myocardial infarction management. As Andrew Sharp notes, persistent chest pain accompanied by ECG changes should trigger immediate catheterization, irrespective of ST-elevation criteria. As the understanding of OMI continues to evolve, it is clear that this paradigm shift, supported by innovative solutions like MaxYield™, is essential for optimizing cardiac care and improving outcomes for patients.
Key Characteristics of OMI: Features and Implications
Key characteristics of Occlusive Myocardial Infarction (OMI) include the acute nature of coronary occlusion, the potential for significant myocardial damage, and the urgent need for intervention, which illustrates the OMI meaning. This condition presents unique challenges in , particularly because OMI can manifest with normal ECG findings. This complicates diagnosis without the aid of advanced analytical tools, leading to a substantial risk of misdiagnosis. Such errors can result in treatment delays, negatively affecting patient outcomes.
Advanced technologies, especially [AI-driven ECG analysis platforms](https://theneuralcloud.com), play a pivotal role in understanding OMI meaning. These platforms meticulously analyze complex cardiac signals, delivering real-time alerts to healthcare providers. This capability not only enhances diagnostic accuracy but also streamlines clinical workflows, facilitating quicker decision-making in critical situations. As specialists have noted, conventional STEMI standards fail to recognize acute coronary occlusion in approximately 30% of NSTEMI individuals, highlighting the urgent need for enhanced diagnostic systems.
The integration of AI tools in ECG interpretation is essential for recognizing subtle EKG patterns that are indicative of OMI meaning. By improving the identification process, these technologies ultimately lead to better patient management and outcomes. The use of AI in this context represents a significant advancement in the medical field, ensuring that healthcare professionals can respond effectively to the complexities of the OMI meaning.

Conclusion
Understanding Occlusion Myocardial Infarction (OMI) is crucial for improving patient care and outcomes in healthcare settings. This condition, characterized by acute coronary artery blockage, necessitates immediate intervention to avert significant heart damage. Recognizing the distinct features of OMI and the urgency for prompt action can lead to enhanced treatment strategies, ultimately saving lives.
The article underscores the vital role of advanced diagnostic tools in the accurate identification of OMI. Traditional methods often prove inadequate, resulting in treatment delays that can negatively impact patient outcomes. The integration of AI-driven platforms, such as those developed by Neural Cloud Solutions, illustrates how technology can enhance the detection of OMI, enabling healthcare professionals to make swift, informed decisions. Additionally, the historical evolution of OMI classification emphasizes the continuous need for adaptation in clinical guidelines and training to address the complexities of this condition.
In summary, the importance of understanding OMI in the context of health technology is paramount. As healthcare evolves, adopting advanced diagnostic tools and raising awareness of OMI will be essential for improving cardiac care. By prioritizing timely recognition and intervention, the healthcare sector can significantly enhance patient outcomes, ensuring that individuals experiencing acute coronary events receive the urgent care they require.
Frequently Asked Questions
What does OMI stand for and what does it mean?
OMI stands for Occlusion Myocardial Infarction, which is a critical type of myocardial infarction characterized by the acute or near-total occlusion of a coronary artery, leading to insufficient blood flow to the heart muscle.
Why is recognizing OMI important?
Recognizing OMI is vital because timely revascularization significantly enhances patient outcomes. Prompt medical intervention can prevent significant damage or necrosis of cardiac tissue.
How does OMI differ from other types of myocardial infarction?
OMI differs from other types, such as STEMI (ST-Elevation Myocardial Infarction), in that it requires immediate medical intervention to restore blood flow and mitigate heart damage, even if it does not meet the standard criteria for STEMI.
What are the consequences of misclassifying OMI?
Misclassifying OMI can lead to delays in treatment; research shows that approximately 25-30% of individuals with OMI do not receive prompt treatment, resulting in severe consequences.
What is the OMI AI model and how does it improve detection?
The OMI AI model is a diagnostic tool that has shown superior accuracy in detecting OMI compared to traditional methods, achieving an area under the curve (AUC) of 0.938. It helps reclassify one in three individuals presenting with chest pain.
How does the OMI AI model analyze ECG signals?
The OMI AI model effectively maps ECG signals through noise, isolating and labeling key features such as P-wave, QRS complex, and T-wave onsets and offsets, converting noisy ECG recordings into clear insights.
What do cardiologists emphasize regarding OMI recognition?
Cardiologists stress the importance of recognizing OMI, indicating that ongoing chest pain with ECG changes should not be ignored, even if it does not meet the criteria for ST-elevation MI.
What is the significance of prompt intervention for OMI?
Prompt intervention is essential for the management of OMI, as it directly influences treatment strategies and outcomes for patients, making the integration of advanced diagnostic technologies crucial.






